Pregabalin for the Treatment of Drug and Alcohol Withdrawal Symptoms: a Comprehensive Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
“GABA” 'Bout? Pregabalin and Gabapentin Abuse
3/19/18 What’s All the “GABA” ‘Bout? Pregabalin and Gabapentin Abuse Courtney Kominek, PharmD, BCPS, CPE Disclosures .Courtney Kominek, PharmD, BCPS, CPE –Axial Healthcare – Consultant .The views and opinions expressed in this presentation are those of the authors and do not necessarily reflect the official policy or position of any agency of the United States government, including the Department of Veterans Affairs. 1 3/19/18 Learning Objectives .Review the proposed mechanisms of action (MOA) for gabapentin and pregabalin. .Explain the proposed rationale as to why gabapentin and pregabalin have become drugs of abuse. .Identify signs and symptoms of withdrawal that an addicted or tolerant patient may experience upon abrupt discontinuation of gabapentin or pregabalin. .Discuss updates on changes in pain management given the increase in gabapentin and pregabalin abuse. Current Situation Opioid overdose public health crisis Rising use of nonopioid medications including gabapentin Opioids and concomitant gabapentin increase risk for overdose Reports of gabapentinoid abuse Changes in PDMP and scheduling at state level http://www.register-herald.com/news/manchin-asks-fda-dea-to-consider-rescheduling-gabapentin/article_442fa04b-7ed9-5bf8-8d19-b5440e9c278b.html 2 3/19/18 Gabapentin and Pregabalin: Pharmacology and Pharmacokinetics Fact or Alternate Fact? .Gabapentin and pregabalin work on GABA. 3 3/19/18 Mechanism of Action Structurally related to GABA and has GABA-mimetic properties Do not • Alter uptake or breakdown • Convert into GABA • Bind to GABAa or GABAB Binds to the α2-δ subunit of the voltage-gated calcium channel Reduces the Ca2+ -dependent release of pro-nociceptive neurotransmitters Decreases release of glutamate, NE, and substance P Dworkin RH et al. -

Membrane Stabilizer Medications in the Treatment of Chronic Neuropathic Pain: a Comprehensive Review
Current Pain and Headache Reports (2019) 23: 37 https://doi.org/10.1007/s11916-019-0774-0 OTHER PAIN (A KAYE AND N VADIVELU, SECTION EDITORS) Membrane Stabilizer Medications in the Treatment of Chronic Neuropathic Pain: a Comprehensive Review Omar Viswanath1,2,3 & Ivan Urits4 & Mark R. Jones4 & Jacqueline M. Peck5 & Justin Kochanski6 & Morgan Hasegawa6 & Best Anyama7 & Alan D. Kaye7 Published online: 1 May 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Neuropathic pain is often debilitating, severely limiting the daily lives of patients who are affected. Typically, neuropathic pain is difficult to manage and, as a result, leads to progression into a chronic condition that is, in many instances, refractory to medical management. Recent Findings Gabapentinoids, belonging to the calcium channel blocking class of drugs, have shown good efficacy in the management of chronic pain and are thus commonly utilized as first-line therapy. Various sodium channel blocking drugs, belonging to the categories of anticonvulsants and local anesthetics, have demonstrated varying degrees of efficacy in the in the treatment of neurogenic pain. Summary Though there is limited medical literature as to efficacy of any one drug, individualized multimodal therapy can provide significant analgesia to patients with chronic neuropathic pain. Keywords Neuropathic pain . Chronic pain . Ion Channel blockers . Anticonvulsants . Membrane stabilizers Introduction Neuropathic pain, which is a result of nervous system injury or lives of patients who are affected. Frequently, it is difficult to dysfunction, is often debilitating, severely limiting the daily manage and as a result leads to the progression of a chronic condition that is, in many instances, refractory to medical This article is part of the Topical Collection on Other Pain management. -

Intranasal Pregabalin Administration: a Review of the Literature and the Worldwide Spontaneous Reporting System of Adverse Drug Reactions
brain sciences Perspective Intranasal Pregabalin Administration: A Review of the Literature and the Worldwide Spontaneous Reporting System of Adverse Drug Reactions Mohamed Elsayed *, René Zeiss, Maximilian Gahr, Bernhard J. Connemann and Carlos Schönfeldt-Lecuona Department of Psychiatry and Psychotherapy III, University of Ulm, Leimgrubenweg 12-14, 89075 Ulm, Germany; [email protected] (R.Z.); [email protected] (M.G.); [email protected] (B.J.C.); [email protected] (C.S.-L.) * Correspondence: [email protected]; Tel.: +49-(0)-731-500-61411; Fax: +49-(0)-731-500-61412 Received: 2 October 2019; Accepted: 11 November 2019; Published: 13 November 2019 Abstract: Background: It is repeatedly reported that pregabalin (PRG) and gabapentin feature a potential for abuse/misuse, predominantly in patients with former or active substance use disorder. The most common route of use is oral, though reports of sublingual, intravenous, rectal, and smoking administration also exist. A narrative review was performed to provide an overview of current knowledge about nasal PRG use. Methods: A narrative review of the currently available literature of nasal PRG use was performed by searching the MEDLINE, EMBASE, and Web of Science databases. The abstracts and articles identified were reviewed and examined for relevance. Secondly, a request regarding reports of cases of nasal PRG administration was performed in the worldwide spontaneous reporting system of adverse drug reactions of the European Medicines Agency (EMA, EudraVigilance database). Results: The literature search resulted in two reported cases of nasal PRG use. In the analysis of the EMA-database, 13 reported cases of nasal PRG use (11 male (two not specified), mean age of users = 34.2 years (four not specified)) were found. -

Gabapentin Enacarbil (Horizant) Monograph
Gabapentin enacarbil (Horizant) Monograph ® Gabapentin Enacarbil (Horizant ) National Drug Monograph March 2012 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. These documents will be updated when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. Executive Summary: Gabapentin enacarbil (Horizant®) is a prodrug of gabapentin which binds with high affinity to the α2δ subunit of voltage-activated calcium channels in vitro studies. It is unknown how the binding of gabapentin enacarbil (GEn) to the α2δ subunit corresponds to the treatment of restless leg syndrome (RLS) symptoms. Indication: GEn is FDA approved for treatment of RLS. Pharmacokinetics: GEn is primarily excreted by the kidneys and neither gabapentin nor GEn is substrate, inhibitor, or inducer of the major CYP450 system. In addition, GEn is not an inhibitor or substrate of p-glycoprotein in vitro. Dose: The recommended dosage is 600 mg once daily taken with food at about 5 PM. Efficacy: Several studies examining GEn have shown efficacy over placebo in patients with RLS; improvement in RLS symptoms was observed within 7 days of starting treatment.6-8, 12-14 Three studies demonstrated 1200 mg/day GEn significantly reduced International Restless Legs Syndrome (IRLS) scale total score and improved Clinical Global Impression– Improvement (CGI-I) scale compared with placebo.6-8 Two studies demonstrated efficacy at lower dose of 600 mg/day GEn; however, another study did not.7,12,13 These results are comparable to those seen with dopamine agonists.8,12 Adverse Drug Events: Commonly reported adverse effects for the approved dose of 600 mg/day GEn are somnolence, sedation and dizziness. -

Novel Treatments for Cocaine and Opioid Use Disorder
Novel Treatments for Cocaine and Opioid Use Disorder Kyle M. Kampman M.D. Department of Psychiatry Perelman School of Medicine University of Pennsylvania [email protected] “How about cocaine?” Outline • Medications for Cocaine Use Disorder • A lot of pilot trials / a lot of failure • Topiramate +/- amphetamine for CUD • Cocaine biomarkers • Metyrapone and oxazepam for CUD • Medications for Opioid Use Disorder • Injectables / Implantables • Rapid detoxification protocols Cocaine overdose deaths are common in AAs Annals of Internal Medicine 2018 168 (6) 453-455 Targets for cocaine meds - GABAA Glu Prefrontal Cortex + & Hippocampus, PPT Glutamate Ventral Amygdala, Thalamus Pallidum D1 - D2 GABA - GABAA Glu Nucleus Glu + + Accumbens κ-opioid D1 GABA Dopamine DAT - - D2 Dynorphin - D2 Enkephalin - GABAA Ventral Output Tegmentum Treatment of cocaine dependence - topiramate Topiramate is Associated with Cocaine Abstinence Drug Alcohol Depend. 2004;75(3):233-40. Topiramate for cocaine dependence Topiramate Associated with Greater End of Trial Abstinence Drug Alcohol Depend. 2013;133(1):94-9 Topiramate for cocaine dependence Topiramate Reduced Cocaine Use JAMA Psychiatry. 2013;70(12):1338-46 Dopaminergic Medications: Dextroamphetamine Long-Acting Dextroamphetamine Reduced Cocaine Use J Clin Psychopharmacol 2001; 21:522-6 Dopaminergic Medications: Methamphetamine Long-Acting Methamphetamine Reduced Cocaine Use Drug Alcohol Depend 2009; 101:34-41 Glutamatergic / Dopaminergic Combinations: MAS + Topiramate The Combination of MAS and -

Acute Pain Management in Patients with Drug Dependence Syndrome Jane Quinlan, FRCA, Ffpmrcaa,*, Felicia Cox, Frcnb
Acute pain management in patients with drug dependence syndrome Jane Quinlan, FRCA, FFPMRCAa,*, Felicia Cox, FRCNb Keywords: acute pain, opioid substitution therapy, analgesics, opioid, behavior, addiction The patients we describe in this review are those who use illicit Key Points opioids, such as heroin, those who use diverted prescription opioids for nonmedical use, or those who take other illicit drugs. These drugs include stimulants (amphetamines, cocaine), 1. Engaging in open and honest discussions with the patient depressants (alcohol, barbiturates, benzodiazepines), and others and caregivers to agree to a management and discharge including cannabis, mescaline, and LSD. plan with clear, achievable goals. 2. Using strategies that both provide effective analgesia and prevent withdrawal syndrome, which are 2 separate 1. Definitions goals. The nomenclature around the illicit use of drugs remains 3. The early recognition and treatment of symptoms and confusing, but the recent International Statistical Classification behavioral changes that might indicate withdrawal. of Diseases and Related Health Problems (ICD-10, released by 4. Using tamper-proof and secure analgesia administration the World Health Organization in 2016) uses “dependence procedures. syndrome” as the preferred term.32 Other terms such as 5. Using regional analgesia where possible, although it may “addiction,” “substance use disorder,” and “substance misuse” be a challenge in patients who have depressed immunity relate to the same condition, but for the purpose of clarity and or local or systemic sepsis from injections. simplicity we use “dependence syndrome” in this review. Dependence syndrome is defined as follows: abstinent are no longer physically dependent on the drug but are particularly vulnerable to relapse, owing to the chronic A cluster of behavioral, cognitive, and physiological phe- changes induced by drug use. -

Potential Benefits of N-Acetylcysteine in Preventing Pregabalin-Induced Seeking-Like Behavior
healthcare Article Potential Benefits of N-Acetylcysteine in Preventing Pregabalin-Induced Seeking-Like Behavior Atiah H. Almalki 1,2 , Hashem O. Alsaab 2,3, Walaa F. Alsanie 2,4, Ahmed Gaber 2,5 , Turki Alkhalifa 6, Ahmad Almalki 6, Omar Alzahrani 2, Ana Maria Gregio Hardy 7, Qasim Alhadidi 8, Zahoor A. Shah 9 and Yusuf S. Althobaiti 2,6,10,* 1 Department of Pharmaceutical Chemistry, College of Pharmacy, Taif University, P.O. Box 11099, Taif 21944, Saudi Arabia; [email protected] 2 Addiction and Neuroscience Research Unit, Taif University, P.O. Box 11099, Taif 21944, Saudi Arabia; [email protected] (H.O.A.); [email protected] (W.F.A.); [email protected] (A.G.); [email protected] (O.A.) 3 Department of Pharmaceutics and Pharmaceutical Technology, College of Pharmacy, Taif University, P.O. Box 11099, Taif 21944, Saudi Arabia 4 Department of Clinical Laboratories Sciences, The Faculty of Applied Medical Sciences, Taif University, P.O. Box 11099, Taif 21944, Saudi Arabia 5 Department of Biology, College of Science, Taif University, P.O. Box 11099, Taif 21944, Saudi Arabia 6 Ministry of Interior, General Directorate of Narcotics Control, General Administration for Precursors and Laboratories, Riyadh 11564, Saudi Arabia; [email protected] (T.A.); [email protected] (A.A.) 7 Department of Physiology and Pharmacology, College of Medicine and Life Sciences, University of Toledo, Toledo, OH 43614, USA; [email protected] 8 Citation: Almalki, A.H.; Alsaab, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford Medical School, H.O.; Alsanie, W.F.; Gaber, A.; Stanford University, Stanford, CA 94305, USA; [email protected] 9 Department of Medicinal and Biological Chemistry, College of Pharmacy and Pharmaceutical Sciences, Alkhalifa, T.; Almalki, A.; Alzahrani, University of Toledo, Toledo, OH 43614, USA; [email protected] O.; Hardy, A.M.G.; Alhadidi, Q.; 10 Department of Pharmacology and Toxicology, College of Pharmacy, Taif University, P.O. -

Augmentation Suffering and What Can Be Done About It
AUGMENTATION SUFFERING AND WHAT CAN BE DONE ABOUT IT John W. Winkelman MD PhD Massachusetts General Hospital Harvard Medical School Boston, MA Disclosure Information Type of Affiliation Commercial Entity Consultant/Honoraria UCB Research Grant Purdue Pharma UCB WHITE PAPER SUMMARY OF RECOMMENDATIONS FOR THE PREVENTION AND TREATMENT OF RLS/WED AUGMENTATION A COMBINED TASK FORCE OF THE IRLSSG, EURLSSG AND THE RLS-FOUNDATION AUGMENTATION Augmentation is a long-term (6 months-years) complication of RLS treatment with dopaminergic medications Dopaminergic (DA) medications: Levodopa (Sinemet) Pramipexole (Mirapex) Ropinirole (Requip) Rotigotine (Neupro) AUGMENTATION DEFINITION Compared to before medication was initiated there is: Advance in the time of symptom onset More intense symptoms Symptoms start faster after lying down/sitting Extension of symptoms to arms In short, RLS gets worse with medication treatment! AUGMENTATION SEVERITY EXISTS ALONG A CONTINUUM Pre-augmentation/tolerance: DA medication dose needs to be increased to maintain effectiveness but there is no change in timing of symptoms Mild: 2-4 hour advance in time of RLS symptom onset, most days Severe: 4-8 hour advance in the time of RLS symptom onset, most days Very severe: RLS symptoms present much of the day and night WHAT WORSENS RLS BUT ISN’T AUGMENTATION Iron deficiency Medication effects Antidepressants Antihistamines Dopamine blockers (anti-nausea or antipsychotics) Sleep disruption/deprivation (eg sleep apnea, insomnia) More time spent immobile (in -
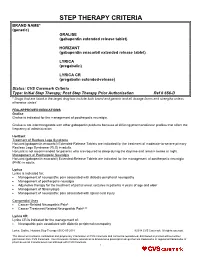
STEP THERAPY CRITERIA BRAND NAME* (Generic) GRALISE (Gabapentin Extended Release Tablet)
STEP THERAPY CRITERIA BRAND NAME* (generic) GRALISE (gabapentin extended release tablet) HORIZANT (gabapentin enacarbil extended release tablet) LYRICA (pregabalin) LYRICA CR (pregabalin extended-release) Status: CVS Caremark Criteria Type: Initial Step Therapy; Post Step Therapy Prior Authorization Ref # 656-D * Drugs that are listed in the target drug box include both brand and generic and all dosage forms and strengths unless otherwise stated FDA-APPROVED INDICATIONS Gralise Gralise is indicated for the management of postherpetic neuralgia. Gralise is not interchangeable with other gabapentin products because of differing pharmacokinetic profiles that affect the frequency of administration. Horizant Treatment of Restless Legs Syndrome Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the treatment of moderate-to-severe primary Restless Legs Syndrome (RLS) in adults. Horizant is not recommended for patients who are required to sleep during the daytime and remain awake at night. Management of Postherpetic Neuralgia Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the management of postherpetic neuralgia (PHN) in adults. Lyrica Lyrica is indicated for: Management of neuropathic pain associated with diabetic peripheral neuropathy Management of postherpetic neuralgia Adjunctive therapy for the treatment of partial onset seizures in patients 4 years of age and older Management of fibromyalgia Management of neuropathic pain associated with spinal cord injury Compendial Uses Cancer-Related Neuropathic Pain6 Cancer Treatment Related Neuropathic Pain6,12 Lyrica CR Lyrica CR is indicated for the management of: Neuropathic pain associated with diabetic peripheral neuropathy Lyrica, Gralise, Horizant Step Therapy 656-D 05-2018 ©2018 CVS Caremark. All rights reserved. This document contains confidential and proprietary information of CVS Caremark and cannot be reproduced, distributed or printed without written permission from CVS Caremark. -

Drugs and New Potentially Dangerous Chemical Substances, with a Brief Review of the Problem
INTERNATIONAL JOURNAL OF ENVIRONMENTAL & SCIENCE EDUCATION 2016, VOL. 11, NO. 14, 6697-6703 OPEN ACCESS Approach to Classifying “Design” Drugs and New Potentially Dangerous Chemical Substances, With a Brief Review of the Problem Azat R. Asadullina, Elena Kh. Galeevab, Elvina A. Achmetovaa and Ivan V. Nikolaevb aBashkir State Medical University of the Ministry of Health of the Russian Federation, Ufa, RUSSIA; bRepublican Narcological Dispensary No.1 of the Ministry of Health of the Republic of Bashkortostan, Ufa, RUSSIA ABSTRACT The urgency of this study has become vivid in the light of the growing problem of prevalence and bBPHFuse Republican of new synthetic Narcological drug types. DispensaryLately there has No.1 been of a thetendency Ministry of expanding of Health the rangeof the of psychologically active substances (PAS) used by addicts with the purpose of their illegal taking. RepublicThe aim of Bashkortostan,of this research is anPushkin attempt str.,of systematizing 119/1, Ufa, and RB. classifying “design” drugs according to their chemical structure, neurochemical mechanisms of action and clinical manifestations. As a result, we have found that they can be divided into ten big groups. This classification will allow to better arrange new clinical phenomenology in modern addictology. This paper would be useful for psychiatrists, experts in narcology, as well as for personnel of institutions and agencies engaged in anti-drug activity. KEYWORDS ARTICLE HISTORY Opiates, cannabinoids, cathinones, tryptamine, Received 20 April 2016 cocaine, pregabalin, new “design” drugs, Revised 28 May 2016 classification Accepted 29 Мау 2016 Introduction Urgency of the problem Recently, the sphere of illegal turnover of narcotic substances has shown an apparent trend of producing the so-called “design drugs” (DN): new potentially dangerous psychologically active substances (NPDPAS) obtained by means of chemical synthesis, possessing a high narcotic effect and manufactured with the CORRESPONDENCE Azat R. -

Anticonvulsants As Anxiolytics, Part 2 Pregabalin And
B R A I N S T O R M S Clinical Neuroscience Update Anticonvulsants as Anxiolytics, Part 2 Pregabalin and Gabapentin as α2δ Ligands at Voltage-Gated Calcium Channels Stephen M. Stahl, M.D., Ph.D. α δ Issue: Anticonvulsants that act as ligands at 2 subunits of voltage- gated calcium channels may also prove to be novel anxiolytics. ctivation of fear circuits tion of neurotransmitter release.5–10 If increased during neurotransmission, is a leading hypothesis this reduction happens in amygdala- neurotransmitter release is thus en- A for explaining symptoms centered fear circuits, it might have hanced. On the other hand, when the 1–3 α δ in anxiety disorders, and returning anxiolytic actions. 2 ligands pregabalin and gabapen- neurotransmission in these circuits to tin bind to these channels and thereby a more normal pattern may reduce KNOW YOUR CALCIUM CHANNELS: decrease calcium flow through them, certain symptoms.4 For example, anti- VOLTAGE-SENSITIVE OR the release of several neurotrans- convulsants may theoretically reduce LIGAND-GATED? mitters from presynaptic neurons is seizures by decreasing excessive out- decreased.5–10 put from epileptic neurons, and could, Most clinicians have heard of cal- Another subtype of voltage-gated by analogy, reduce symptoms of anxi- cium channels, but only recently has it calcium channels is an L channel, ety if these agents were also able to become clear that there are multiple which resides in membranes of vascu- decrease neuronal activation within subtypes of calcium channels, some lar smooth muscle and