Health Needs Assessment 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RDA Riverina Overview 2011 RDA Riverina Connecting Communities, Business & Government to Projects, Programs, Services Funding and Other People
RDA Riverina Overview 2011 RDA Riverina connecting communities, business & government to projects, programs, services funding and other people. A NSW Government Initiative Vision RDA Riverina will be a region renowned for its excellence in all dimensions – economic, social and environmental with emphasis on innovation, life long learning, healthy living and an optimistic outward looking culture based on confidence, resilience and social inclusion. Mission RDA Riverina will build partnerships that facilitate the development of a sustainable region. Hillston CARRATHOOL New South Wales SYDNEY GRIFFITH Hillston COOTAMUNDRA HAY TEMORA CANBERRA LEETONCARRATHOOL New South Wales MURRUMBIDGEE NARRANDERA COOLAMON JUNEE SYDNEY GRIFFITH Wagga Wagga GUNDAGAI COOTAMUNDRA HAY TEMORA CANBERRA WAGGA LEETON LOCKHART WAGGA MURRUMBIDGEE NARRANDERA COOLAMON JUNEE Wagga Wagga GUNDAGAI WAGGA LOCKHART WAGGA www.rdariverina.org.au Contents • Introduction 03 • A message from the Chairman 05 • Organisational Structure 06 • About this Report - Sub Commiitee 07 • Infrastructure 08 • Business Development 10 • Promotion 12 • Environmental Sustainability 15 • All of Government Approach 17 • Building Capacity 21 03 Regional Development Australia Riverina Overview 2011 Introduction Who is Regional Development Australia? Regional Development Australia (RDA) is a Australia, Local Government, Arts & Sport) & the partnership between the Australian, state, State Minister (The Hon. Andrew Stoner MP, NSW territory and local governments to develop and Minster for Trade & Investment). Members have strengthen the regional communities in Australia. a broad and diverse skills base developing local RDA includes the Department of Regional solutions to local problems. Australia, Local Government, Arts & Sport, State In New South Wales there are 14 RDAs. RDA Departments as well as a national network of Riverina is composed of 13 local government 55 committees (RDAs) that were established areas (LGAs): Carrathool, Coolamon, in August 2009. -

Talkabout-April-2016-.Pdf
Volume 19 No 1 April 2016 The 1950/51 Infants' Section decided to play football with the Small Schools' Division. PRESIDENT’S MESSAGE Can you find a fellow student of WWTC? Can you help? Have you done your homework? Have you any WWTC memorabilia? As President of the WWTCAA these questions have been the challenges issued over the past year to our membership. I am pleased to report that the responses to these challenges have been fantastic. We have found more members and traced some of those lost to the mailing list. There are more alumni actively involved in organisation and operations of the association. Homework submissions for publication in Talkabout have come from a broad range of our membership and many of our retirees are digging into their garages and cupboards to find memorabilia for archives. How good is Talkabout? The contributions from members always make this publication an interesting read. Expressions of appreciation are always forthcoming. It certainly serves the function of keeping people informed and in touch with their colleagues and provides a forum for disseminating information about our association’s activities. It was pleasing to have reports from three of our most recent scholar- ship holders as they complete their course and commence their careers in education. Our Association has been able to increase the amount offered from $6000 to $8000 to the successful final year student(s) in education thanks to the support of our members. Cont’d p2 PRESIDENT’S MESSAGE Cont’d There has been an increasing nous Scholarship Foundation of It would be remiss of me not to interest in developing and en- a school is made. -

Murrumbidgee Regional Fact Sheet
Murrumbidgee region Overview The Murrumbidgee region is home The river and national parks provide to about 550,000 people and covers ideal spots for swimming, fishing, 84,000 km2 – 8% of the Murray– bushwalking, camping and bird Darling Basin. watching. Dryland cropping, grazing and The Murrumbidgee River provides irrigated agriculture are important a critical water supply to several industries, with 42% of NSW grapes regional centres and towns including and 50% of Australia’s rice grown in Canberra, Gundagai, Wagga Wagga, the region. Narrandera, Leeton, Griffith, Hay and Balranald. The region’s villages Chicken production employs such as Goolgowi, Merriwagga and 350 people in the area, aquaculture Carrathool use aquifers and deep allows the production of Murray bores as their potable supply. cod and cotton has also been grown since 2010. Image: Murrumbidgee River at Wagga Wagga, NSW Carnarvon N.P. r e v i r e R iv e R v i o g N re r r e a v i W R o l g n Augathella a L r e v i R d r a W Chesterton Range N.P. Charleville Mitchell Morven Roma Cheepie Miles River Chinchilla amine Cond Condamine k e e r r ve C i R l M e a nn a h lo Dalby c r a Surat a B e n e o B a Wyandra R Tara i v e r QUEENSLAND Brisbane Toowoomba Moonie Thrushton er National e Riv ooni Park M k Beardmore Reservoir Millmerran e r e ve r i R C ir e e St George W n i Allora b e Bollon N r e Jack Taylor Weir iv R Cunnamulla e n n N lo k a e B Warwick e r C Inglewood a l a l l a g n u Coolmunda Reservoir M N acintyre River Goondiwindi 25 Dirranbandi M Stanthorpe 0 50 Currawinya N.P. -

161024Road Condition Report
LACHLAN SHIRE COUNCIL PO BOX 216 CONDOBOLIN NSW 2877 PHONE: (02) 68 951 900 FAX: (02) 68 953 478 ROAD CONDITION REPORT To: Media Release From: Keith Dawe Company: Councils & Communication Outlets Date: 24 October 2016 Report Number: 66 Time: 3:00PM Next review: Tuesday 25th October 2016 3 pages Many roads in Lachlan Shire are impacted by flooding as noted below. Long distance travel through Condobolin is not recommended with roads flooded and damaged. Road closures variously restrict light vehicles, heavy vehicles or all vehicles. Please take a safer alternate route or better still, defer travel if not essential. See attached map. Condobolin access to West Wyalong via Gipps Way is open – temporary repairs have been completed on the road. Caution as water remains over the road in a number of locations. Access for high clearance 4wd vehicles less than 3 tonne is available from Condobolin to Tullibigeal, Lake Cargelligo and West Wyalong via SR230 Lachlan Valley Way and SR1029 Tullibigeal Road. Caution as road condition is deteriorating Extra caution is advised as many roads are affected by current flooding or the residual effects from flooding, including soft shoulders, washouts, bog holes, potholes, slippery road surfaces, debris, water on roads and hidden hazards under the water. Conditions can change quickly. More land holders may lose access – make preparations before roads are closed by flooding . Tottenham area – residual damage from flooding, caution is advised: • Tullamore–Narromine road now open to vehicles under 3 tonne – severe road damage. • MR347 Dandaloo Road , Albert-Trangie – open with caution , temporary repairs. • SR3 Tabratong Crossing Road , Tottenham-Nevertire – open with caution , temporary repairs and one lane traffic access. -

Howlong News My Golf
Friday 13th March, 2020 HOWLONG NEWS MY GOLF Pictured: Some of our MyGolf participants practicing their putting skills on Sunday 1st March In case you’re wondering, the putt on the right went in! FROM PRESIDENT KIM GRAY Welcome to our March newsletter. 2020 at Clubhouse reception for absentee members who present themselves at reception. The Club’s Financial Report has been completed and externally audited, reviewed by the Board Under the triennial system three positions will and approved for the year ended 30th be vacated by rotation and any qualifying November 2019. A Profit of $52,742 has been member may nominate for a position on the reported for the year and whilst this is below Board for a three year term. I am available to our initial budget expectations we understand discuss with any prospective member any the stresses which have prevailed during the details regarding the role of a Director prior to year. An opportunity to detail our result will be the closure of nominations on Monday 16th open to members at our Information evening to April at 5:00pm. I intend re-nominating for the be held at 5pm on Monday 30th March at the President’s position. club. An important resolution has also been passed by Our Annual General Meeting is scheduled for the Board which will disallow the use of Monday 20th April 2020 and I am pleased to Members Points for the payment of advise that a change to voting process has been Membership fees with effect forthwith. We approved by the Board, which will allow pre understand this may not necessarily be popular AGM Voting. -

Albury CLSD Minutes 26 August 2020, 1:30-3:30, Via Video Conference
Albury CLSD Minutes 26 August 2020, 1:30-3:30, via video conference Present: Winnecke Baker (Legal Aid NSW), Simon Crase (CLSD Coordinator, UMFC/HRCLS), Kerry Wright (Legal Aid NSW WDO Team), Julie Maron (Legal Aid NSW), Sue Beddowes (Interreach Albury), Jesmine Coromandel (Manager, WDVCAS), Michelle Conroy (One Door Family and Carer Mental Health Program), Susan Morris (One Door Family and Carer Mental Health Program), Diane Small (Albury City Council), Scott Boyle (Anglicare Financial Counselling), Heidi Bradbrun (Justice Conect), Nicole Stack (Legal Aid WDO Team), Julie Bye (EWON), Britt Cooksey (Amaranth Foundation Corowa), Natalie Neumann (Legal Aid NSW), Diana Elliot (Mirambeena Community Centre), Kim Andersen (Centacare South West NSW), Navinesh Nand (Legal Aid NSW), Stacey Telford (Safety Action Meeting Coordinator), Jenny Rawlings (Department of Communities and Justice – Housing), Nicole Dwyer (SIC Legal Aid NSW Riverina/Murray), Andrea Georgiou (HRCLS) Apologies: Jenny Ryder (Amaranth Foundation) Agenda Item Discussion Action/Responsibility/Time 1. Welcome, Simon acknowledged the respective Aboriginal lands that partners called in from today and welcomed purpose & everyone to the meeting. acknowledgement 2. Service check-in Susan Morris and Michelle Conroy – One Door Family and Carer Mental Health Susan: [email protected] 0488 288 707 (mon-wed) Michelle: 0481 010 728 [email protected] (tues, wed, thurs) FREE service that people can engage with as many times as they need to. Support groups are available in Albury, Corowa and Deniliquin. Both mostly working from home, but Michelle is getting back on the road. Albury CLSD Program Albury Regional Coordinator [email protected] – 0488 792 366 1 Nicole Stack and Kerry Wright – Legal Aid WDO team 4228 8299 or [email protected] Cover the NSW South Coast and Riverina/Murray. -

A Response to the Draft Guide to the Murray Darling Basin Plan
A Response to the Draft Guide to the Murray Darling Basin Plan 152 Oaklands Road Berrigan 2712 NSW ‐ 03 5885 2392 0416 156429 [email protected] 1 | Page A Brief History of West Corurgan P.I.D: The concept of the West Corurgan Private Irrigation District was first recorded in a document ‘The Case for Corugan’ published in 1938. From that point the commitment of the proponents of the scheme was unwavering right up to the commissioning of the West Corurgan Private Irrigation District on the 12th of April 1969. The District straddles the municipalities of Berrigan, Corowa, Jerilderie and Urana, covering a tract of land 212,000 hectares, delivering irrigation to 21,200 hectares via 565 kilometres of open channel. The Headworks is located 10 kilometres downstream of Corowa, lifting water 13 metres via 5 pumps into the Main Channel. From there the water is dispersed via gravity over the entire length and breadth of the district as far northwest as the Billabong Creek. The district is bounded by the townships of Berrigan, Corowa, Oaklands, Jerilderie and Urana. Agribusiness in the district includes but is not limited to beef, dairy, lamb and pork production, wool as well as rice, wheat, barley, potato and fodder cropping. Future agribusiness enterprises include but are not limited to fruit and vegetable production utilising open and reticulating irrigation practices together with wine grapes, flowers and aquaculture enterprises. The W.C.P.I.D is privately owned and fully funded by its membership. It does not enjoy the benefit of any funding or financial assistance by the State or Federal government. -

Listing and Sitting Arrangements, Nsw Local Court
LISTING AND SITTING ARRANGEMENTS, NSW LOCAL COURT Listing and sitting arrangements of the NSW Local Court Click on the links below to find the listing and sitting arrangements for each court. CHAMBER DAYS – Please note that Chamber Days have been cancelled from August 2020 to March 2021 to allow for the listing of defended work Albion Park Broken Hill Deniliquin Albury Burwood Downing Centre Armidale Byron Bay Dubbo Assessors - Small Claims Camden Dunedoo Ballina Campbelltown Dungog Bankstown Campbelltown Children's Eden Batemans Bay Casino Fairfield Bathurst Central Finley Bega Cessnock Forbes Bellingen Cobar Forster Belmont Coffs Harbour Gilgandra Bidura Children's Court Commonwealth Matters - Glen Innes (Glebe) (see Surry Hills see Downing Centre Gloucester Children’s Court) Condobolin Gosford Blayney Cooma Goulburn Blacktown Coonabarabran Grafton Boggabilla Coonamble Grenfell Bombala Cootamundra Griffith Bourke Corowa Gulgong Brewarrina Cowra Broadmeadow Children's Gundagai Crookwell Court Circuits Gunnedah 1 LISTING AND SITTING ARRANGEMENTS, NSW LOCAL COURT Hay Manly Nyngan Hillston Mid North Coast Children’s Oberon Court Circuit Holbrook Orange Milton Hornsby Parkes Moama Hunter Children’s Court Parramatta Circuit Moree Parramatta Children’s Court Illawarra Children's Court Moruya Peak Hill (Nowra, Pt. Kembla, Moss Moss Vale Vale and Goulburn) Penrith Mt Druitt Inverell Picton Moulamein Junee Port Kembla Mudgee Katoomba Port Macquarie Mullumbimby Kempsey Queanbeyan Mungindi Kiama Quirindi Murrurundi Kurri Kurri Raymond Terrace Murwillumbah -

Outback NSW Regional
TO QUILPIE 485km, A THARGOMINDAH 289km B C D E TO CUNNAMULLA 136km F TO CUNNAMULLA 75km G H I J TO ST GEORGE 44km K Source: © DEPARTMENT OF LANDS Nindigully PANORAMA AVENUE BATHURST 2795 29º00'S Olive Downs 141º00'E 142º00'E www.lands.nsw.gov.au 143º00'E 144º00'E 145º00'E 146º00'E 147º00'E 148º00'E 149º00'E 85 Campground MITCHELL Cameron 61 © Copyright LANDS & Cartoscope Pty Ltd Corner CURRAWINYA Bungunya NAT PK Talwood Dog Fence Dirranbandi (locality) STURT NAT PK Dunwinnie (locality) 0 20 40 60 Boonangar Hungerford Daymar Crossing 405km BRISBANE Kilometres Thallon 75 New QUEENSLAND TO 48km, GOONDIWINDI 80 (locality) 1 Waka England Barringun CULGOA Kunopia 1 Region (locality) FLOODPLAIN 66 NAT PK Boomi Index to adjoining Map Jobs Gate Lake 44 Cartoscope maps Dead Horse 38 Hebel Bokhara Gully Campground CULGOA 19 Tibooburra NAT PK Caloona (locality) 74 Outback Mungindi Dolgelly Mount Wood NSW Map Dubbo River Goodooga Angledool (locality) Bore CORNER 54 Campground Neeworra LEDKNAPPER 40 COUNTRY Region NEW SOUTH WALES (locality) Enngonia NAT RES Weilmoringle STORE Riverina Map 96 Bengerang Check at store for River 122 supply of fuel Region Garah 106 Mungunyah Gundabloui Map (locality) Crossing 44 Milparinka (locality) Fordetail VISIT HISTORIC see Map 11 elec 181 Wanaaring Lednapper Moppin MILPARINKA Lightning Ridge (locality) 79 Crossing Coocoran 103km (locality) 74 Lake 7 Lightning Ridge 30º00'S 76 (locality) Ashley 97 Bore Bath Collymongle 133 TO GOONDIWINDI Birrie (locality) 2 Collerina NARRAN Collarenebri Bullarah 2 (locality) LAKE 36 NOCOLECHE (locality) Salt 71 NAT RES 9 150º00'E NAT RES Pokataroo 38 Lake GWYDIR HWY Grave of 52 MOREE Eliza Kennedy Unsealed roads on 194 (locality) Cumborah 61 Poison Gate Telleraga this map can be difficult (locality) 120km Pincally in wet conditions HWY 82 46 Merrywinebone Swamp 29 Largest Grain (locality) Hollow TO INVERELL 37 98 For detail Silo in Sth. -

MIGRATION to AUSTRALIA in the Mid to Late Nineteenth Expected to Be a Heavy Loser, Were Buried in the Meant That the Men’S Social Chinese, in Particular Their Portant
Step Back In Time MIGRATION TO AUSTRALIA In the mid to late nineteenth expected to be a heavy loser, were buried in the meant that the men’s social Chinese, in particular their portant. century a combination of as the whole of his vegetable denominational sections of lives were pursued largely readiness to donate money to For other men the powerful push and pull garden would be ruined, and the local cemetery. outside a family environment the local hospitals and help in Australian family was factors led to an expected other market After a time the graves in and that sexual relations other fund raising efforts. paramount. Emboldened by unprecedented rise in gardeners along the river to the Chinese cemeteries were involved crossing the racial Alliances and associations an intricate system of inter- Chinese migration to other also suffer. exhumed and the bones and cultural divide. began to change over time. marriage, clan and family parts of Asia, the Americas In the mid 1870s the transported to China for Most social activity in the Many Chinese men, part- allegiances and networks, and Australia. Chinese began cultivating reburial. camps took place in the icularly the storekeepers, many Chinese men in The principal source of tobacco and maize, focusing Exhumations were temples, lodges, gambling were members of one of the Australia went on to create migrants was Guangdong their efforts on the Tumut and elaborate and painstaking houses and opium rooms, Christian churches and miniature dynasties and (Kwangtung) Province in Gundagai areas. undertakings and were although home visits and married, mostly to European become highly respected southern China, in the south The growth of the industry carried out through the hui or entertainments also occ- women, although a number within their local comm- west of the province and areas was rapid. -
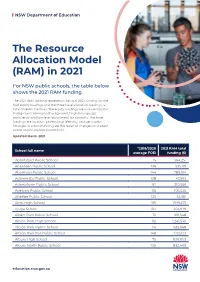
The Resource Allocation Model (RAM) in 2021
NSW Department of Education The Resource Allocation Model (RAM) in 2021 For NSW public schools, the table below shows the 2021 RAM funding. The 2021 RAM funding represents the total 2021 funding for the four equity loadings and the three base allocation loadings, a total of seven loadings. The equity loadings are socio-economic background, Aboriginal background, English language proficiency and low-level adjustment for disability. The base loadings are location, professional learning, and per capita. Changes in school funding are the result of changes to student needs and/or student enrolments. Updated March 2021 *2019/2020 2021 RAM total School full name average FOEI funding ($) Abbotsford Public School 15 364,251 Aberdeen Public School 136 535,119 Abermain Public School 144 786,614 Adaminaby Public School 108 47,993 Adamstown Public School 62 310,566 Adelong Public School 116 106,526 Afterlee Public School 125 32,361 Airds High School 169 1,919,475 Ajuga School 164 203,979 Albert Park Public School 111 251,548 Albion Park High School 112 1,241,530 Albion Park Public School 114 626,668 Albion Park Rail Public School 148 1,125,123 Albury High School 75 930,003 Albury North Public School 159 832,460 education.nsw.gov.au NSW Department of Education *2019/2020 2021 RAM total School full name average FOEI funding ($) Albury Public School 55 519,998 Albury West Public School 156 527,585 Aldavilla Public School 117 681,035 Alexandria Park Community School 58 1,030,224 Alfords Point Public School 57 252,497 Allambie Heights Public School 15 -

Deliverabiliy of Environmental Water in the Murray Valleyx
Deliverability of Environmental Water in the Murray Valley Report to Murray Group of Concerned Communities May 2012 Final Report Version: 3.0 Page 1 of 41 Citation Murray Catchment Management Authority (2012) Deliverability of Environmental Water in the Murray Valley. © 2012 Murray Catchment Management Authority This work is copyright. With the exception of the photographs, any logo or emblem, and any trademarks, the work may be stored, retrieved and reproduced in whole or part, provided that it is not sold or used for commercial benefit. Any reproduction of information from this work must acknowledge Murray Group of Concerned Communities, Murray Catchment Management Authority, or the relevant third party, as appropriate as the owner of copyright in any selected material or information. Apart from any use permitted under the Copyright Act 1968 (Cth) or above, no part of this work may be reproduced by any process without prior written permission from Murray Group of Concerned Communities or Murray Catchment Management Authority. Murray Group of Concerned Communities Disclaimer This report has been prepared for Murray Group of Concerned Communities and is made available for general use to assist public knowledge and discussion regarding the development of the Draft Murray Darling Basin Plan. The opinions, comments and analysis (including those of third parties) expressed in this document are for information purposes only. This document does not indicate the Murray Group of Concerned Communities’ commitment to undertake or implement a particular