Adrenal Insufficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Adrenal Hyperplasia in the Newborn
The Leo Fung Center for CAH and Disorders of Sex Development Congenital Adrenal Hyperplasia in the Newborn Contents Introduction 1 What is congenital adrenal hyperplasia? 1 Types of CAH 3 Diagnosing CAH in newborns 4 Treating CAH 5 Untreated CAH 7 CAH in children and young adults 8 Frequently asked questions 9 Glossary 11 Resources 13 Acknowledgments 14 Congenital Adrenal Hyperplasia in the Newborn 1 Introduction This handbook will provide you and your family information about congenital adrenal hyperplasia (CAH). While this guide will not answer all of your questions, it will provide basic medical facts that will help you to talk to your doctors. It is important to know that CAH cannot be cured but it can be treated. Your child will need to take medicine for the rest of his or her life. If your child takes this medicine, he or she should have a completely normal life in every way. Successful treatment requires teamwork between you and your doctor. The doctor will monitor your child in order to know what dose of medicine is needed. We ask that you give your baby the medication on the schedule recommended by your doctor. Your family is not alone. The Leo Fung Center for CAH and Disorders of Sex Development (DSD) at University of Minnesota Amplatz Children’s Hospital, provides a large network of support, including medical specialists, therapists and counselors who all have expertise in caring for patients with CAH. What is congenital adrenal hyperplasia? Let’s begin by examining each word. • Congenital means existing at birth (inherited). • Adrenal means that the adrenal glands are involved. -

Conduct Protocol in Emergency: Acute Adrenal Insufficiency
ORIGINAL ARTICLE FARES AND SANTOS Conduct protocol in emergency: Acute adrenal insufficiency ADIL BACHIR FARES1*, RÔMULO AUGUSTO DOS SANTOS2 1Medical Student, 6th year, Faculdade de Medicina de São José do Rio Preto (Famerp), São José do Rio Preto, SP, Brazil 2Degree in Endocrinology and Metabology from Sociedade Brasileira de Endocrinologia e Metabologia (SBEM). Assistant Physician at the Internal Medicine Service of Hospital de Base. Researcher at Centro Integrado de Pesquisa (CIP), Hospital de Base, São José do Rio Preto. Endocrinology Coordinator of the Specialties Outpatient Clinic (AME), São José do Rio Preto, SP, Brazil SUMMARY Introduction: Acute adrenal insufficiency or addisonian crisis is a rare comor- bidity in emergency; however, if not properly diagnosed and treated, it may progress unfavorably. Objective: To alert all health professionals about the diagnosis and correct treatment of this complication. Method: We performed an extensive search of the medical literature using spe- cific search tools, retrieving 20 articles on the topic. Results: Addisonian crisis is a difficult diagnosis due to the unspecificity of its signs and symptoms. Nevertheless, it can be suspected in patients who enter the emergency room with complaints of abdominal pain, hypotension unresponsive to volume or vasopressor agents, clouding, and torpor. This situation may be associated with symptoms suggestive of chronic adrenal insufficiency such as hyperpigmentation, salt craving, and association with autoimmune diseases such as vitiligo and Hashimoto’s thyroiditis. Hemodynamically stable patients Study conducted at Faculdade may undergo more accurate diagnostic methods to confirm or rule out addiso- de Medicina de São José do nian crisis. Delay to perform diagnostic tests should be avoided, in any circum- Rio Preto (Famerp), São José do Rio Preto, SP, Brazil stances, and unstable patients should be immediately medicated with intravenous glucocorticoid, even before confirmatory tests. -

1 Progesterone: an Enigmatic Ligand for the Mineralocorticoid Receptor
Progesterone: An Enigmatic Ligand for the Mineralocorticoid Receptor Michael E. Baker1 Yoshinao Katsu2 1Division of Nephrology-Hypertension Department of Medicine, 0735 University of California, San Diego 9500 Gilman Drive La Jolla, CA 92093-0735 2Graduate School of Life Science Hokkaido University Sapporo, Japan Correspondence to: M. E. Baker; E-mail: [email protected] Y. Katsu; E-mail: [email protected] Abstract. The progesterone receptor (PR) mediates progesterone regulation of female reproductive physiology, as well as gene transcription in non-reproductive tissues, such as brain, bone, lung and vasculature, in both women and men. An unusual property of progesterone is its high affinity for the mineralocorticoid receptor (MR), which regulates electrolyte transport in the kidney in humans and other terrestrial vertebrates. In humans, rats, alligators and frogs, progesterone antagonizes activation of the MR by aldosterone, the physiological mineralocorticoid in terrestrial vertebrates. In contrast, in elephant shark, ray-finned fishes and chickens, progesterone activates the MR. Interestingly, cartilaginous fishes and ray-finned fishes do not synthesize aldosterone, raising the question of which steroid(s) activate the MR in cartilaginous fishes and ray-finned fishes. The simpler synthesis of progesterone, compared to cortisol and other corticosteroids, makes progesterone a candidate physiological activator of the MR in elephant sharks and ray-finned fishes. Elephant shark and ray-finned fish MRs are expressed in diverse tissues, including heart, brain and lung, as well as, ovary and testis, two reproductive tissues that are targets for progesterone, which together suggests a multi-faceted physiological role for progesterone activation of the MR in elephant shark and ray-finned fish. -

Preventable Deaths: Panhypopituitarism and Adrenal Insufficiency
Preventable Deaths: Panhypopituitarism and adrenal insufficiency. What you need to know What is panhypopituitarism? Your child has been diagnosed with a big scary sounding word, and all you can think is: 'What does this mean? and 'Why have I never heard of this?' Simply put, panhypopituitarism means that your child's pituitary gland does not function properly and as a result, your child is deficient in one or several hormones. Some children have congenital panhypopituitarism, meaning they are born with it. Others have acquired panhypopituitarism following an event such as head trauma, brain tumor surgery, or brain radiation. It is rare enough that is entirely possible, in fact, probable, that you will not initially know anyone else with this disorder. What will my child need? Although the diagnosis and condition can seem intimidating, it is very manageable once you understand what is needed. Unfortunately the condition cannot be cured or reversed, but again, it can be effectively managed. Your child will need to take medications to replace the missing hormones. These might include thyroid hormone, growth hormone, cortisol, and/or possibly others. Your doctor will go over these with you, as dosages vary from child to child. Most medications are taken orally, but growth hormone must be taken by daily injection. Your endocrinologist will work with you and your child to achieve the proper dosages and will guide you in how to administer any necessary medications. Why is it sometimes life threatening? What is adrenal insufficiency? Of the hormone deficiencies your child may have, the most critical is cortisol, also known as the 'stress hormone.' Cortisol is essential for life , and is therefore the central focus of this guide. -

Mineralocorticoid Receptor Mutations
234 1 M-C ZENNARO and MR mutations 234:1 T93–T106 Thematic Review F FERNANDES-ROSA 30 YEARS OF THE MINERALOCORTICOID RECEPTOR Mineralocorticoid receptor mutations Maria-Christina Zennaro1,2,3 and Fabio Fernandes-Rosa1,2,3 Correspondence 1INSERM, Paris Cardiovascular Research Center, Paris, France should be addressed 2Université Paris Descartes, Sorbonne Paris Cité, Paris, France to M-C Zennaro 3Assistance Publique-Hôpitaux de Paris, Hôpital Européen Georges Pompidou, Service de Génétique, Email Paris, France maria-christina.zennaro@ inserm.fr Abstract Aldosterone and the mineralocorticoid receptor (MR) are key elements for maintaining Key Words fluid and electrolyte homeostasis as well as regulation of blood pressure. Loss-of- f mineralocorticoid function mutations of the MR are responsible for renal pseudohypoaldosteronism type receptor 1 (PHA1), a rare disease of mineralocorticoid resistance presenting in the newborn with f pseudohypoaldosteronism type 1- PHA1 weight loss, failure to thrive, vomiting and dehydration, associated with hyperkalemia f aldosterone and metabolic acidosis, despite extremely elevated levels of plasma renin and f hormone receptors aldosterone. In contrast, a MR gain-of-function mutation has been associated with a f nuclear receptor familial form of inherited mineralocorticoid hypertension exacerbated by pregnancy. In Endocrinology addition to rare variants, frequent functional single nucleotide polymorphisms of the of MR are associated with salt sensitivity, blood pressure, stress response and depression in the general population. This review will summarize our knowledge on MR mutations in Journal PHA1, reporting our experience on the genetic diagnosis in a large number of patients performed in the last 10 years at a national reference center for the disease. -

Endocrine Drugs
PharmacologyPharmacologyPharmacology DrugsDrugs thatthat AffectAffect thethe EndocrineEndocrine SystemSystem TopicsTopicsTopics •• Pituitary Pituitary DrugsDrugs •• Parathyroid/Thyroid Parathyroid/Thyroid DrugsDrugs •• Adrenal Adrenal DrugsDrugs •• Pancreatic Pancreatic DrugsDrugs •• Reproductive Reproductive DrugsDrugs •• Sexual Sexual BehaviorBehavior DrugsDrugs FunctionsFunctionsFunctions •• Regulation Regulation •• Control Control GlandsGlandsGlands ExocrineExocrine EndocrineEndocrine •• Secrete Secrete enzymesenzymes •• Secrete Secrete hormoneshormones •• Close Close toto organsorgans •• Transport Transport viavia bloodstreambloodstream •• Require Require receptorsreceptors NervousNervous EndocrineEndocrine WiredWired WirelessWireless NeurotransmittersNeurotransmitters HormonesHormones ShortShort DistanceDistance LongLong Distance Distance ClosenessCloseness ReceptorReceptor Specificity Specificity RapidRapid OnsetOnset DelayedDelayed Onset Onset ShortShort DurationDuration ProlongedProlonged Duration Duration RapidRapid ResponseResponse RegulationRegulation MechanismMechanismMechanism ofofof ActionActionAction HypothalamusHypothalamusHypothalamus HypothalamicHypothalamicHypothalamic ControlControlControl PituitaryPituitaryPituitary PosteriorPosteriorPosterior PituitaryPituitaryPituitary Target Actions Oxytocin Uterus ↑ Contraction Mammary ↑ Milk let-down ADH Kidneys ↑ Water reabsorption AnteriorAnteriorAnterior PituitaryPituitaryPituitary Target Action GH Most tissue ↑ Growth TSH Thyroid ↑ TH secretion ACTH Adrenal ↑ Cortisol Cortex -

Agonistic and Antagonistic Properties of Progesterone Metabolites at The
European Journal of Endocrinology (2002) 146 789–800 ISSN 0804-4643 EXPERIMENTAL STUDY Agonistic and antagonistic properties of progesterone metabolites at the human mineralocorticoid receptor M Quinkler, B Meyer, C Bumke-Vogt, C Grossmann, U Gruber, W Oelkers, S Diederich and V Ba¨hr Department of Endocrinology, Klinikum Benjamin Franklin, Freie Universita¨t Berlin, Hindenburgdamm 30, 12200 Berlin, Germany (Correspondence should be addressed to M Quinkler; Email: [email protected]) Abstract Objective: Progesterone binds to the human mineralocorticoid receptor (hMR) with nearly the same affinity as do aldosterone and cortisol, but confers only low agonistic activity. It is still unclear how aldosterone can act as a mineralocorticoid in situations with high progesterone concentrations, e.g. pregnancy. One mechanism could be conversion of progesterone to inactive compounds in hMR target tissues. Design: We analyzed the agonist and antagonist activities of 16 progesterone metabolites by their binding characteristics for hMR as well as functional studies assessing transactivation. Methods: We studied binding affinity using hMR expressed in a T7-coupled rabbit reticulocyte lysate system. We used co-transfection of an hMR expression vector together with a luciferase reporter gene in CV-1 cells to investigate agonistic and antagonistic properties. Results: Progesterone and 11b-OH-progesterone (11b-OH-P) showed a slightly higher binding affinity than cortisol, deoxycorticosterone and aldosterone. 20a-dihydro(DH)-P, 5a-DH-P and 17a-OH-P had a 3- to 10-fold lower binding potency. All other progesterone metabolites showed a weak affinity for hMR. 20a-DH-P exhibited the strongest agonistic potency among the metabolites tested, reaching 11.5% of aldosterone transactivation. -
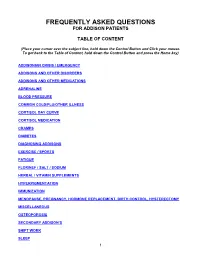
Frequently Asked Questions for Addison Patients
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

6. Endocrine System 6.1 - Drugs Used in Diabetes Also See SIGN 116: Management of Diabetes, 2010
1 6. Endocrine System 6.1 - Drugs used in Diabetes Also see SIGN 116: Management of Diabetes, 2010 http://www.sign.ac.uk/guidelines/fulltext/116 Insulin Prescribing Guidance in Type 2 Diabetes http://www.fifeadtc.scot.nhs.uk/media/6978/insulin-prescribing-in-type-2-diabetes.pdf 6.1.1 Insulins (Type 2 Diabetes) 6.1.1.1 Short Acting Insulins 1st Choice S – Insuman ® Rapid (Human Insulin) S – Humulin S ® S – Actrapid ® 2nd Choice S – Insulin Aspart (NovoRapid ®) (Insulin Analogues) S – Insulin Lispro (Humalog ®) 6.1.1.2 Intermediate and Long Acting Insulins 1st Choice S – Isophane Insulin (Insuman Basal ®) (Human Insulin) S – Isophane Insulin (Humulin I ®) S – Isophane Insulin (Insulatard ®) 2nd Choice S – Insulin Detemir (Levemir ®) (Insulin Analogues) S – Insulin Glargine (Lantus ®) Biphasic Insulins 1st Choice S – Biphasic Isophane (Human Insulin) (Insuman Comb ® ‘15’, ‘25’,’50’) S – Biphasic Isophane (Humulin M3 ®) 2nd Choice S – Biphasic Aspart (Novomix ® 30) (Insulin Analogues) S – Biphasic Lispro (Humalog ® Mix ‘25’ or ‘50’) Prescribing Points For patients with Type 1 diabetes, insulin will be initiated by a diabetes specialist with continuation of prescribing in primary care. Insulin analogues are the preferred insulins for use in Type 1 diabetes. Cartridge formulations of insulin are preferred to alternative formulations Type 2 patients who are newly prescribed insulin should usually be started on NPH isophane insulin, (e.g. Insuman Basal ®, Humulin I ®, Insulatard ®). Long-acting recombinant human insulin analogues (e.g. Levemir ®, Lantus ®) offer no significant clinical advantage for most type 2 patients and are much more expensive. In terms of human insulin. The Insuman ® range is currently the most cost-effective and preferred in new patients. -

Systolic Blood Pressure
Iatrogenic Cushing’s Syndrome secondary to the Combined Oral Contraceptive Pill in a patient with Congenital Adrenal Hyperplasia Satish Artham, Yaasir Mamoojee, Simon Ashwell. Department of Diabetes and Endocrinology, The James cook University Hospital, Middlesbrough, UK Introduction: Systolic blood pressure: Congenital Adrenal Hyperplasia (CAH) is a rare genetic disorder characterised by deficiency of cortisol and/or mineralocorticoid hormones with over production of sex steroids. 21-hydroxylase deficiency is the commonest cause of CAH accounting for 95% of cases1,2. Severe form of classic CAH occurs in 1 in 15,000 livebirths worldwide3,4. The goals of treating 21-hydroxylase deficiency in women is to replace the deficient steroid hormones, to lower the adrenal precursors and sex steroids. Most commonly used regimens are prednisolone once a day or hydrocortisone split into two or three doses. Case: Discussion: A 30 year old women with CAH diagnosed at birth was on replacement with hydrocortisone and fludrocortisone. She was investigated for ongoing diarrhoea Cortisol is the main glucocorticoid hormone, the majority of by the gastroenterologist and was subsequently diagnosed with Irritable Bowel which is circulated bound to Cortisol Binding Globulin (CBG). Syndrome (IBS). She was then started on buscopan and codeine phosphate for Only about 5% of the circulating cortisol is free. Cortisol action symptom relief. However during her menstrual cycle her abdominal symptoms is terminated by conversion into inactive forms by various were not sufficiently controlled. She was thus commenced on Microgynon, enzymes. It is mainly metabolised in the liver. It is reduced, a Combined Oral Contraceptive Pill (COCP). Within a year of initiation she oxidised and hydroxylated, the products of which are made developed cushingoid features, became hypertensive and started gaining weight. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid.