Ebola Risk Assessment in the Pig Value Chain in Uganda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Land Reform and Sustainable Livelihoods
! M4 -vJ / / / o rtr £,/- -n AO ^ l> /4- e^^/of^'i e i & ' cy6; s 6 cy6; S 6 s- ' c fwsrnun Of WVELOPMENT STUDIES LIBRARY Acknowledgements The researchers would like to thank Ireland Aid and APSO for funding the research; the Ministers for Agriculture and Lands, Dr. Kisamba Mugerwa and Hon. Baguma Isoke for their support and contribution; and the Irish Embassy in Kampala for its support. Many thanks also to all who provided valuable insights into the research topic through interviews, focus group discussions and questionnaire surveys in Kampala and Kibaale District. Finally: a special word of thanks to supervisors and research fellows in MISR, particularly Mr Patrick Mulindwa who co-ordinated most of the field-based activities, and to Mr. Nick Chisholm in UCC for advice and direction particularly at design and analysis stages. BLDS (British Library for Development Studies) Institute of Development Studies Brighton BN1 9RE Tel: (01273) 915659 Email: [email protected] Website: www.blds.ids.ac.uk Please return by: Executive Summary Chapter One - Background and Introduction This report is one of the direct outputs of policy orientated research on land tenure / land reform conducted in specific areas of Uganda and South Africa. The main goal of the research is to document information and analysis on key issues relating to the land reform programme in Uganda. It is intended that that the following pages will provide those involved with the land reform process in Kibaale with information on: • how the land reform process is being carried out at a local level • who the various resource users are, how they are involved in the land reform, and how each is likely to benefit / loose • empirical evidence on gainers and losers (if any) from reform in other countries • the gender implications of tenure reform • how conflicts over resource rights are dealt with • essential supports to the reform process (e.g. -

Accessibility to First-Mile Health Services: a Time-Cost Model for Rural Uganda
Social Science & Medicine 265 (2020) 113410 Contents lists available at ScienceDirect Social Science & Medicine journal homepage: http://www.elsevier.com/locate/socscimed Accessibility to First-Mile health services: A time-cost model for rural Uganda Roberto Moro Visconti a,*, Alberto Larocca b, Michele Marconi c a Department of Business Management, Catholic University of Sacred Heart, Via Ludovico Necchi, 7, 20123, Milan, Italy b Cosmo Ltd., A183/20, 11th Close South Odorkor Estate Greater Accra, Ghana c Universita` Politecnica delle Marche, Dipartimento di Scienze della, Vita e dell’Ambiente, Via Brecce Bianche, 60126, Ancona, Italy ARTICLE INFO ABSTRACT Keywords: This study estimates the geographical disconnection in rural Low-Middle-Income Countries (LMIC) between Barriers to care First-Mile suppliers of healthcare services and end-users. This detachment is due to geographical barriers and to a Remote diagnosis shortage of technical, financial,and human resources that enable peripheral health facilities to perform effective Geographic information systems and prompt diagnosis. End-users typically have easier access to cell-phones than hospitals, so mHealth can help Home-patient to overcome such barriers, transforming inpatients/outpatients into home-patients, decongesting hospitals, Results-based financing Healthcare cost-effectiveness especially during epidemics. This generates savings for patients and the healthcare system. The advantages of mHealth are well known, but there is a literature gap in the description of its economic returns. This study applies a geographical model to a typical LMIC, Uganda, quantifying the time-cost to reach an equipped medical center. Time-cost measures the disconnection between First-Mile hubs and end-users, the potential demand of mHealth by remote end-users, and the consequent savings. -

WHO UGANDA BULLETIN February 2016 Ehealth MONTHLY BULLETIN
WHO UGANDA BULLETIN February 2016 eHEALTH MONTHLY BULLETIN Welcome to this 1st issue of the eHealth Bulletin, a production 2015 of the WHO Country Office. Disease October November December This monthly bulletin is intended to bridge the gap between the Cholera existing weekly and quarterly bulletins; focus on a one or two disease/event that featured prominently in a given month; pro- Typhoid fever mote data utilization and information sharing. Malaria This issue focuses on cholera, typhoid and malaria during the Source: Health Facility Outpatient Monthly Reports, Month of December 2015. Completeness of monthly reporting DHIS2, MoH for December 2015 was above 90% across all the four regions. Typhoid fever Distribution of Typhoid Fever During the month of December 2015, typhoid cases were reported by nearly all districts. Central region reported the highest number, with Kampala, Wakiso, Mubende and Luweero contributing to the bulk of these numbers. In the north, high numbers were reported by Gulu, Arua and Koti- do. Cholera Outbreaks of cholera were also reported by several districts, across the country. 1 Visit our website www.whouganda.org and follow us on World Health Organization, Uganda @WHOUganda WHO UGANDA eHEALTH BULLETIN February 2016 Typhoid District Cholera Kisoro District 12 Fever Kitgum District 4 169 Abim District 43 Koboko District 26 Adjumani District 5 Kole District Agago District 26 85 Kotido District 347 Alebtong District 1 Kumi District 6 502 Amolatar District 58 Kween District 45 Amudat District 11 Kyankwanzi District -

Killing the Goose That Lays the Golden Egg
KILLING THE GOOSE THAT LAYS THE GOLDEN EGG An Analysis of Budget Allocations and Revenue from the Environment and Natural Resource Sector in Karamoja Region Caroline Adoch Eugene Gerald Ssemakula ACODE Policy Research Series No.47, 2011 KILLING THE GOOSE THAT LAYS THE GOLDEN EGG An Analysis of Budget Allocations and Revenue from the Environment and Natural Resource Sector in Karamoja Region Caroline Adoch Eugene Gerald Ssemakula ACODE Policy Research Series No.47, 2011 Published by ACODE P. O. Box 29836, Kampala Email: [email protected]; [email protected] Website: http://www.acode-u.org Citation: Adoch, C., and Ssemakula, E., (2011). Killing the Goose that Lays the Golden Egg: An Analysis of Budget Allocations and Revenue from the Environment and Natural Resource Sector in Karamoja Region. ACODE Policy Research Series, No. 47, 2011. Kampala. © ACODE 2011 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher. ACODE policy work is supported by generous donations and grants from bilateral donors and charitable foundations. The reproduction or use of this publication for academic or charitable purposes or for purposes of informing public policy is excluded from this restriction. ISBN 978997007077 Contents LIST OF FIGURES ................................................................................................. v LIST OF TABLES .................................................................................................. -

Cipla Prospectus.Pdf
IPO Prospectus QCIL Cipla Cipla_prospect_2018_Cover.indd 1 8/9/18 6:35 PM CiplaQCIL Prospectus This Prospectus provides detailed information about the Company and the Offer. Potential investors in respect of the Offer Shares are advised to read this document carefully and retain it for future reference. In the event that a potential investor is not clear about the action to take, he/she should consult his/her stockbroker, banker, lawyer, auditor and/or other financial, legal and tax advisor for guidance and carefully review the risks associated with an investment in the Company. 1 Cipla_prospect_Intro pages.indd 1 8/10/18 7:12 PM CiplaQCIL IPO Prospectus CAUTION: This document is important and requires your careful attention. This document is a prospectus inviting the public to acquire the Offer Shares under the terms of application set out herein. If you wish to apply for the Offer Shares, then you must complete the procedures for application and payment set out in Section 19 of this document. A copy of this Prospectus has been delivered to the CMA for approval and to the Uganda Registration Services Bureau, the Registrar of Companies. The Uganda Registration Services Bureau has not checked and will not check the accuracy of any statements made and accepts no responsibility for it or for financial soundness of the Company or the value of the securities concerned. The securities offered have not been approved or disapproved by the CMA. Prospective investors should carefully consider the matters set forth under the caption “Risk Factors”. Your attention is also drawn to the selling restrictions and other information in the “Important Information” Section of this Prospectus. -

COVID-19 Effects on the Construction Industry
Issue No. 15, August 2020 THEME: COVID-19 & CONSTRUCTION SAFETY: Keep your site safe during COVID-19 crisis COVID-19: Govt’s intervention to aid sector ’s recovery is crucial RULES: Strict regulation key in eliminating shoddy work COVID-19 effects on the construction industry www.unabcec.co.ug UNABCEC UNABCEC_UG AUGUST, 2020 1 COVID-19 should The Contractor Magazine is a quarterly publication that acts as the voice for the leave you with AUTHENTIC ICON construction industry. We print and distribute The Contractor free of charge to UNABCEC many lessons members and all stakeholders in the construc- tion industry, international and local partners, am excited about this particular is- ministries, departments and agencies, works sue of The Contractor, you should and technical officers of all central and local I too, and this is why. Government entities, Members of Parliament, The lockdown was lifted and for banks, embassies, academic institutions and most sectors, work has resumed nor- the general public. We highlight issues and mally. Although operations of the con- possible solutions relating to the construction struction sector had not been halted as that usually happen at construction business community. Visit our website today to sites. Therefore, in addition to wear- access soft copies of the recent issues. part of measures to prevent the spread of the pandemic, operations were ing masks, do not downplay helmets, Call for articles made difficult by several restrictions, boots, reflectors and other safety gear. All articles on construction experiences, including movement of workers and More than this, insure your workers opinions on developing the industry, policy closure of material outlets. -

Art As Social Practice: Transforming Lives Using Sculpture in HIV/AIDS
cultural geographies 18(3) 275–296 Art as social practice: transforming © The Author(s) 2010 Reprints and permission: sagepub. co.uk/journalsPermissions.nav lives using sculpture in HIV/AIDS DOI: 10.1177/1474474010377548 awareness and prevention in Uganda http://cgj.sagepub.com Lilian Nabulime Makerere University, Uganda Cheryl McEwan Geography Department, Durham University Abstract This article explores the possibilities of art as social practice in the context of the fight against HIV/AIDS. It is inspired by notions of art having the capacity to move beyond the spaces of galleries into an expanded field, and thus beyond the visual and into the social. The article examines the potential for sculpture to play a transformative role in HIV/AIDS awareness and prevention, and in transforming the gender relations that shape the dynamics of the spread of the disease. These ideas are developed through discussion of research conducted in Uganda and in the UK, which sought to develop forms of sculptural practice for HIV/AIDS awareness and prevention in Uganda. The article explores the ways in which a series of soap sculptures are an effective tool in the fight against the disease, particularly in communities with high rates of illiteracy and in which discussion of sex and sexuality remains largely taboo. The article contends that countering taboo and facilitating dialogue between women and men, thus encouraging attitudinal and behavioural change, are perhaps the most significant impacts that this form of sculpture can make. This is because while awareness of the disease in Uganda is often high, having the capacity to discuss and act upon this awareness is often problematic, largely because of fear, stigma and taboo, and the unequal gender relations that determine the nature of men and women’s sexual lives. -

Forests, Livelihoods and Poverty Alleviation: the Case of Uganda Forests, Livelihoods and Poverty Alleviation: the Case of Uganda
Forests, livelihoods and poverty alleviation: the case of Uganda Forests, livelihoods and poverty alleviation: the case of Uganda G. Shepherd and C. Kazoora with D. Mueller Food and Agriculture Organization of the United Nations Rome, 2013 The Forestry Policy and InstitutionsWorking Papers report on issues in the work programme of Fao. These working papers do not reflect any official position of FAO. Please refer to the FAO Web site (www.fao.org/forestry) for official information. The purpose of these papers is to provide early information on ongoing activities and programmes, to facilitate dialogue and to stimulate discussion. The Forest Economics, Policy and Products Division works in the broad areas of strenghthening national institutional capacities, including research, education and extension; forest policies and governance; support to national forest programmes; forests, poverty alleviation and food security; participatory forestry and sustainable livelihoods. For further information, please contact: Fred Kafeero Forestry Officer Forest Economics, Policy and Products Division Forestry Department, FAO Viale Delle terme di Caracalla 00153 Rome, Italy Email: [email protected] Website: www.fao.org/forestry Comments and feedback are welcome. For quotation: FAO.2013. Forests, Livelihoods and Poverty alleviation: the case of Uganda, by, G. Shepherd, C. Kazoora and D. Mueller. Forestry Policy and Institutions Working Paper No. 32. Rome. Cover photo: Ankole Cattle of Uganda The designations employed and the presentation of material in this information product do not imply the expression af any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Round Table Report
Uganda ROUNDTABLE REPORT Stakeholders meeting on Tsetse and Trypanosomiasis in Uganda February, 2014 Uganda Trypanosomiasis Control Council (UTCC) SECRETARIAT Coordination Office for Control of Trypanosomiasis in Uganda (COCTU) P.O. Box 16345 KAMPALA (U) E-mail: [email protected] 1 Pictorial highlights of the Roundtable Introduction Convening of the Round Table The meeting was convened by the Uganda Trypanosomiasis Control Council (UTCC) through its Secretariat the Coordinating Office for Control of Trypanosomiasis in Uganda (COCTU). Overtime, UTCC had observed that several interventions in the area of Tsetse and Trypanosomiasis were being implemented in Uganda with several groups working in the same area which led to duplication of effort while other areas ended up being unattended to. Also COCTU needed to understand the approach of the major players in Tsetse and Trypanosomiasis and to enlighten the meeting on its mandate of coordination of all tsetse and trypanosomiaisis activities in Uganda. The meeting was attended by delegates from different partners from University of Edinburgh, Ceva Santé Animale, Veterinarians without Boarders, Makerere University (College of Veterinary Medicine Animal Resources), IK Investment Partners/IK Aid and Relief Enterprise, Liverpool School of Tropical Medicine, and Ugandan participants. Mandate of UTCC The Uganda Trypanosomiasis Control Council which is a body corporate is mandated among others to: - . Ensure effective and efficient implementation of all Tsetse and Trypanosomiasis programs . Formulate policies and determine priorities for Tsetse and Trypanosomiasis . Advise Government and make recommendations for Financial , Human and other resource requirements . In consultation with Uganda National Council for Science and Technology (UNCST) (Act Cap, 209) consider and approve research projects related to Tsetse and Trypanosomiasis and assign them to any institution within or outside the Council. -
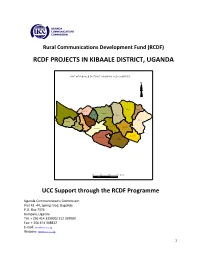
Rcdf Projects in Kibaale District, Uganda
Rural Communications Development Fund (RCDF) RCDF PROJECTS IN KIBAALE DISTRICT, UGANDA MAP O F KIBAAL E DISTRIC T SHO WIN G SUB CO UNTIES N N alwe yo Kisiita R uga sha ri M pee fu Kiry a ng a M aba al e Kakin do Nko ok o Bw ika ra Ky an aiso ke Kag ad i M uho ro Kyeb an do Kasa m by a M uga ra m a Kib aa le TC Bwan s wa Bw am iram ira M atale 10 0 10 20 Kms UCC Support through the RCDF Programme Uganda Communications Commission Plot 42 -44, Spring road, Bugolobi P.O. Box 7376 Kampala, Uganda Tel: + 256 414 339000/ 312 339000 Fax: + 256 414 348832 E-mail: [email protected] Website: www.ucc.co.ug 1 Table of Contents 1- Foreword……………………………………………………………….……….………..………....……3 2- Background…………………………………….………………………..…………..….….….…..……4 3- Introduction………………….……………………………………..…….…………….….….………..4 4- Project profiles……………………………………………………………………….…..…….……...5 5- Stakeholders’ responsibilities………………………………………………….….…........…12 6- Contacts………………..…………………………………………….…………………..…….……….13 List of tables and maps 1- Table showing number of RCDF projects in Kibaale district………….………..….5 2- Map of Uganda showing Kibaale district………..………………….………...……..….14 10- Map of Kibaale district showing sub counties………..…………………………..….15 11- Table showing the population of Kibaale district by sub counties…………..15 12- List of RCDF Projects in Kibaale district…………………………………….…….……..16 Abbreviations/Acronyms UCC Uganda Communications Commission RCDF Rural Communications Development Fund USF Universal Service Fund MCT Multipurpose Community Tele-centre PPDA Public Procurement and Disposal Act of 2003 POP Internet Points of Presence ICT Information and Communications Technology UA Universal Access MoES Ministry of Education and Sports MoH Ministry of Health DHO District Health Officer CAO Chief Administrative Officer RDC Resident District Commissioner 2 1. -

Governance and Development of the East African Community: the Ethical Sustainability Framework
Governance and Development of the East African Community: The Ethical Sustainability Framework Dickson Kanakulya Faculty of Arts and Sciences Studies in Applied Ethics 16 Linköping University, Department of Culture and Communication Linköping 2015 Studies in Applied Ethics 16 Distributed by: Department of Culture and Communication Linköping University 581 83 Linköping Sweden Dickson Kanakulya Governance and Development of the East African Community: The Ethical Sustainability Framework Licentiate thesis Edition 1:1 ISSN 1402‐4152:16 ISBN 978‐91‐7685‐894‐3 © The author Department of Culture and Communication 2015 Declaration: I declare that this study is my original work and a product of my personal critical research and thought. …………………………………………….. Kanakulya Dickson, Kampala, Uganda November, 2015 ii Approval: This research report has been submitted with the approval of my supervisor: Prof. Goran Collste --2015--11--09----- Co-Supervisor’s name: Signature: Date iii © 2015 Kanakulya Dickson All rights reserved iv Dedication: This work is dedicated to the Lord of all Spirits and Letters; accept it as a feeble effort to serve your eternal purposes.To Caroline Kanakulya, a beautiful and kindred spirit. To the healing of the spirit of East Africans.To the watchers who stood steadfast in the days of the multiplication. Great mysteries await across! v Acknowledgements: I acknowledge the Swedish Agency for International Development (Sida) and Makerere University for funding this research; and the staff of Makerere Directorate of Graduate Research and Training for support during the study. My deepest gratitude goes to my wife Caroline Kanakulya, my travel companion in life’s journey; thanks for standing my flaws and supporting me. -

Kibaale District Estimates.Pdf
Local Government Budget Estimates Vote: 524 Kibaale District Structure of Budget Estimates - PART ONE A: Overview of Revenues and Expenditures B: Detailed Estimates of Revenue C: Detailed Estimates of Expenditure D: Status of Arrears Page 1 Local Government Budget Estimates Vote: 524 Kibaale District A: Overview of Revenues and Expenditures Revenue Performance and Plans 2013/14 2014/15 Approved Budget Receipts by End Draft Budget Dec UShs 000's 1. Locally Raised Revenues 670,245 305,658 622,009 2a. Discretionary Government Transfers 2,983,851 1,343,609 3,021,423 2b. Conditional Government Transfers 25,683,207 13,246,056 25,760,436 2c. Other Government Transfers 1,239,235 934,292 1,064,136 3. Local Development Grant 630,022 315,010 630,570 4. Donor Funding 625,438 100,550 625,438 Total Revenues 31,831,998 16,245,176 31,724,013 Expenditure Performance and Plans 2013/14 2014/15 Approved Budget Actual Draft Budget Expenditure by UShs 000's end of Dec 1a Administration 1,360,589 678,287 1,385,819 2 Finance 569,656 255,677 586,085 3 Statutory Bodies 1,191,672 633,033 881,088 4 Production and Marketing 3,527,916 1,862,626 3,414,448 5 Health 4,133,793 1,594,624 4,129,932 6 Education 15,885,248 8,358,540 15,862,642 7a Roads and Engineering 3,237,216 342,301 3,580,630 7b Water 503,557 204,243 528,906 8 Natural Resources 224,651 89,243 221,176 9 Community Based Services 790,471 287,371 760,471 10 Planning 233,769 110,342 219,681 11 Internal Audit 173,460 37,638 153,135 Grand Total 31,831,997 14,453,925 31,724,013 Wage Rec't: 17,375,141 8,567,467 17,375,141 Non Wage Rec't: 8,754,857 3,477,988 9,208,814 Domestic Dev't 5,076,562 2,323,174 4,514,621 Donor Dev't 625,438 85,295 625,438 Page 2 Local Government Budget Estimates Vote: 524 Kibaale District B: Detailed Estimates of Revenue 2013/14 2014/15 UShs 000's Approved Budget Receipts by End Draft Budget of Dec 1.