Half a Century of Heart Transplantation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007
Resident Handbook Division of Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007 For private use of residents only- not for public distribution Table of Contents Anatomic Transplantation Pathology Rotation Clinical Responsibilities of the Division ........................................................3 Categorizations of Specimens and Structure of Signout.................................3 Resident Responsibilities................................................................................4 Learning Resources.........................................................................................4 Transplantation Pathology on the World-Wide Web......................................4 Weekly Schedule ............................................................................................6 Staff Locations and Telephone Numbers........................................................7 Background Articles Landmarks in Transplantation ........................................................................8 Trends in Organ Donation and Transplantation US 1996-2005.....................18 Perspectives in Organ Preservation………....................................................26 Transplant Tolerance- Editorial……………………………………….…….36 Kidney Grading Systems Banff 2005 Update……………………….....................................................42 Banff 97 Components (I t v g etc.) ................................................................44 Readings Banff 05 Meeting Report………………………………………...................47 -

History of Lung Transplantation Akciğer Transplantasyonu Tarihçesi
REVIEW History of Lung Transplantation Akciğer Transplantasyonu Tarihçesi Gül Dabak Unit of Pulmonology, Kartal Kosuyolu Yüksek Ihtisas Teaching Hospital for Cardiovascular Diseases and Surgery, İstanbul ABSTRACT ÖZET History of lung transplantation in the world dates back to the early 20 Dünyada akciğer transplantasyonu tarihçesi, deneysel çalışmala- th century, continues to the first clinical transplantation performed rın yapılmaya başlandığı 20. yüzyılın ilk yıllarından itibaren Ja- by James Hardy in the United States of America in 1963 and comes mes Hardy’ nin Amerika Birleşik Devletleri’nde 1963’te yaptığı to the present with increased frequency. Over 40.000 heart-lung ilk klinik transplantasyona uzanır ve hızlanarak günümüze gelir. and lung transplantations were carried out in the world up to 2011 yılına kadar dünyada 40,000’in üzerinde kalp-akciğer ve 2011. The number of transplant centers and patients is flourishing akciğer transplantasyonu yapılmıştır. Transplantasyon alanındaki in accordance with the increasing demand and success rate in that artan ihtiyaca ve başarılara paralel olarak transplant merkezleri arena. Lung transplantations that started in Turkey at Sureyyapasa ve hasta sayıları da giderek artmaktadır. Türkiye’de 2009 yılında Teaching Hospital for Pulmonary Diseases and Thoracic Surgery Süreyyapaşa Göğüs Hastalıkları ve Cerrahisi Eğitim ve Araştırma in 2009 are being performed at two centers actively to date. This Hastanesi’ nde başlayan akciğer transplantasyonları günümüzde review covers a general outlook on lung transplantations both in iki merkezde aktif olarak yapılmaktadır. Bu derlemede, ülkemiz- the world and in Turkey with details of the first successful lung deki ilk başarılı akciğer transplantasyonu detaylandırılarak dün- transplantation in our country. yada ve ülkemizdeki akciğer transplantasyonu tarihçesi gözden Keywords: Lung transplantation, heart-lung transplantation, his- geçirilmektedir. -
The History of the First Kidney Transplantation
165+3 14 mm "Service to society is the rent we pay for living on this planet" The History of the Joseph E. Murray, 1990 Nobel-laureate who performed the first long-term functioning kidney transplantation in the world First Kidney "The pioneers sacrificed their scientific life to convince the medical society that this will become sooner or later a successful procedure… – …it is a feeling – now I am Transplantation going to overdo - like taking part in creation...” András Németh, who performed the first – a European Overview Hungarian renal transplantation in 1962 E d i t e d b y : "Professor Langer contributes an outstanding “service” to the field by a detailed Robert Langer recording of the history of kidney transplantation as developed throughout Europe. The authoritative information is assembled country by country by a generation of transplant professionals who knew the work of their pioneer predecessors. The accounting as compiled by Professor Langer becomes an essential and exceptional reference document that conveys the “service to society” that kidney transplantation has provided for all mankind and that Dr. Murray urged be done.” Francis L. Delmonico, M.D. Professor of Surgery, Harvard Medical School, Massachusetts General Hospital Past President The Transplantation Society and the Organ Procurement Transplant Network (UNOS) Chair, WHO Task Force Organ and Tissue Donation and Transplantation The History of the First Kidney Transplantation – a European Overview European a – Transplantation Kidney First the of History The ISBN 978-963-331-476-0 Robert Langer 9 789633 314760 The History of the First Kidney Transplantation – a European Overview Edited by: Robert Langer SemmelweisPublishers www.semmelweiskiado.hu Budapest, 2019 © Semmelweis Press and Multimedia Studio Budapest, 2019 eISBN 978-963-331-473-9 All rights reserved. -

Newsletteralumni News of the Newyork-Presbyterian Hospital/Columbia University Department of Surgery Volume 13, Number 1 Summer 2010
NEWSLETTERAlumni News of the NewYork-Presbyterian Hospital/Columbia University Department of Surgery Volume 13, Number 1 Summer 2010 CUMC 2007-2009 Transplant Activity Profile* Activity Kidney Liver Heart Lung Pancreas Baseline list at year start 694 274 174 136 24 Deceased donor transplant 123 124 93 57 11 Living donor transplant 138 17 — 0 — Transplant rate from list 33% 50% 51% 57% 35% Mortality rate while on list 9% 9% 9% 15% 0% New listings 411 217 144 68 23 Wait list at year finish 735 305 204 53 36 2007-June 2008 Percent 1-Year Survival No % No % No % No % No % Adult grafts 610 91 279 86 169 84 123 89 6 100 Adult patients 517 96 262 88 159 84 116 91 5 100 Pediatric grafts 13 100 38 86 51 91 3 100 0 — Pediatric patients 11 100 34 97 47 90 2 100 0 — Summary Data Total 2009 living donor transplants 155 (89% Kidney) Total 2009 deceased donor transplants 408 (30% Kidney, 30% Liver) 2007-June 2008 adult 1-year patient survival range 84% Heart to 100% Pancreas 2007-June 2008 pediatric 1-year patient survival range 90% Heart to 100% Kidney or lung *Health Resource and Service Administration’s Scientific Registry of Transplant Recipients (SRTR) Ed Note. The figure shows the US waiting list for whole organs which will only be partially fulfilled by some 8,000 deceased donors, along with 6,600 living donors, who will provide 28,000 to 29,000 organs in 2010. The Medical Center’s role in this process is summarized in the table, and the articles that follow my note expand on this incredible short fall and its potential solutions. -
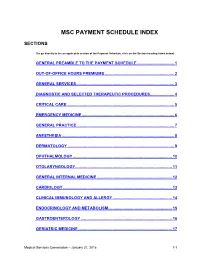
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -

Skin Grafts in Cutaneous Oncology* Enxertia De Pele Em Oncologia
RevABDV81N5.qxd 07.11.06 17:07 Page 465 465 Artigo de Revisão Enxertia de pele em oncologia cutânea* Skin grafts in cutaneous oncology* José Anselmo Lofêgo Filho1 Paula Dadalti2 Diogo Cotrim de Souza3 Paulo Roberto Cotrim de Souza4 Marcos Aurélio Leiros da Silva5 Cristina Maeda Takiya6 Resumo: Em oncologia cutânea depara-se freqüentemente com situações em que a confec- ção de um enxerto é uma boa alternativa para o fechamento do defeito cirúrgico. Conhecer aspectos referentes à integração e contração dos enxertos é fundamental para que os cirur- giões dermatológicos procedam de maneira a não contrariar princípios básicos do trans- plante de pele. Os autores fazem uma revisão da classificação e fisiologia dos enxertos de pele, acrescendo considerações cirúrgicas determinantes para o sucesso do procedimento. Palavras-chave: Neoplasias cutâneas; Transplante de pele; Transplante homólogo Abstract: In cutaneous oncology, there are many situations in which skin grafts could be a good alternative for closing surgical defect. Dermatological surgeons should have enough knowledge about graft integration and contraction in order to not contradict the basic prin- ciples of skin transplantation. The authors review skin graft classification and physiology and make some surgical considerations on successful procedures. Keywords: Skin neoplasms; Skin transplantation; Transplantation, homologous INTRODUÇÃO Enxerto é parte de um tecido vivo transplanta- tológica. São simples quando apresentam um único do de um lugar para outro no mesmo organismo ou tipo de tecido e compostos quando constituídos de em organismos distintos.1 Contudo, a utilização da dois ou mais tipos de tecidos. Em oncologia cutânea, terminologia enxerto para designar uma modalidade um enxerto composto é usado quando o defeito cirúrgica, apesar de errônea, tornou-se coloquial. -

81St, Baltimore, MD, August 5-8, 1998).MISCELLANEOUS
DOCUMENT RESUME ED 423 578 CS 509 922 TITLE Proceedings of the Annual Meeting of the Association for Education in Journalism and Mass Communication (81st, Baltimore, Maryland, August 5-8, 1998) . Miscellaneous. INSTITUTION Association for Education in Journalism and Mass Communication. PUB DATE 1998-08-00 NOTE 458p.; For other sections of these Proceedings, see CS 509 905-921. PUB TYPE Collected Works Proceedings (021) Reports Research (143) EDRS PRICE MF01/PC19 Plus Postage. DESCRIPTORS Ability Grouping; *Advertising; Biotechnology; Case Studies; Comparative Analysis; Computer Literacy; Computer Mediated Communication; *Disabilities; *Ethics; Higher Education; Internship Programs; Organizational Communication; Service Learning; *Television; Textbooks; Writing Research IDENTIFIERS Heart Transplants; *Media Coverage; Religious Movements ABSTRACT The Miscellaneous section of the Proceedings contains the following 15 papers: "Computer Literacy in the Newsroom: A Model for Learning" (Bruce Garrison); "Newspaper Source Use on the Environmental Beat: A Comparative Case Study" (Stephen Lacy and David C. Coulson); "Historical Survey of Media Coverage of Biotechnology in the United States, 1970 to 1996" (Bruce V. Lewenstein, Tracy Allaman, and Shobita Parthasarathy); "Essential and Constructed: Community and Identity in an Online Television Fandom" (Cinda L. Gillilan); "National Print Media Coverage of the Men and Religion Forward Movement, 1911-1917" (Dane S. Claussen); "Miracle in South Africa: A Historical Review of U.S. Magazines' Coverage of the First Heart Transplant" (Raymond N. Ankney); "Physiographic Aggregation and Segmentation: Inclusion of Visually-Detected Physically Impaired Role Models in Advertisements" (Dennis Ganahl and Jeff Kallem); "Effectiveness of Negative Political Advertising" (Won Ho Chang, Sung Wook Shim, and Jaejin Park); "Predicting Successful Internships" (Fred Beard and Linda Morton); "Evaluating Outcomes: Service Learning in the Communication Discipline" (Julia B. -

Cooperating Saves Lives Start Contents
Annual Report 2019 Cooperating saves lives start contents Contents Foreword 1. The Eurotransplant community 2. Eurotransplant: donation, allocation, transplantation and waiting lists This document is optimized for Acrobat Reader for best viewing 3. Report of the Board and the central office experience. 4. Histocompatibility Testing Download Acrobat Reader 5. Reporting of non-resident transplants in Eurotransplant 6. Transplant programs and their delegates in 2019 A high resolution version of this document is also available. 7. Scientific output in 2019 Download high resolution pdf 8. Eurotransplant personnel related statistics 9. Abbreviated financial statements All rights reserved. No part of this publication may be reproduced, stored in a retrieval system List of abbreviations or transmitted, in any form or by any means, electronic, mechanical, photocopying or elsewise, without prior permission of Eurotransplant. For permissions, please contact: [email protected] start contents Foreword Dear reader, We are proud to offer you the 2019, digital edition of the International organ exchange Eurotransplant Annual Report. In this environmentally In 2019, 6981 organs from 2042 deceased donors were friendly, digital report you can easily browse via the used for transplantation for patients on the waiting top menu. Weblinks are added to facilitate in finding list of Eurotransplant. This decrease of the number of more specific information on relevant websites. The reported donors is 5,5% compared to 2018 (2159). report provides an overview of the key statistics on 21.5% of organs were exchanged cross-border between organ donation, allocation and transplantation in all the Eurotransplant member states. Thanks to this Eurotransplant countries. international exchange, a suitable donor organ could be You can also read in the report activities within found for many patients in the different Eurotransplant Eurotransplant that took place, decisions that were member states. -

Analysis of the Trend Over Time of High-Urgency Liver Transplantation Requests in Italy in the 4-Year Period 2014-2017
Analysis of the Trend Over Time of High-Urgency Liver Transplantation Requests in Italy in the 4-Year Period 2014-2017 S. Trapani*, F. Puoti, V. Morabito, D. Peritore, P. Fiaschetti, A. Oliveti, M. Caprio, L. Masiero, L. Rizzato, L. Lombardini, A. Nanni Costa, and M. Cardillo Italian National Transplant Center, Italian Institute of Health, Rome, Italy ABSTRACT Background. The national protocol for the handling of high-urgency (HU) liver organ procurement for transplant is administered by the Italian National Transplant Center. In recent years, we have witnessed a change in requests to access the program. We have therefore evaluated their temporal trend, the need to change the access criteria, the percentage of transplants performed, the time of request satisfaction, and the follow-up. Methods. We analyzed all the liver requests for the HU program received during the 4-year period of 2014 to 2017 for adult recipients (18 years of age): all the variables linked to the recipient or to the donor and the organ transplants are registered in the Informative Transplant System as established by the law 91/99. In addition, intention to treat (ITT) survival rates were compared among 4 different groups: (1) patients on standard waiting lists vs (2) patients on urgency waiting lists, and (3) patients with a history of transplant in urgency vs (4) patients with a history of transplant not in urgency. Results. Out of the 370 requests included in the study, 291 (78.7%) were satisfied with liver transplantation. Seventy-nine requests (21.3%) have not been processed, but if we consider only the real failures, this percentage falls to 13.1% and the percentage of satisfied requests rises to 86.9%. -

2004 Final Program
The International Society for Heart and Lung Transplantation (a forum that includes basic science, the failing heart, and advanced lung disease) Twenty-Fourth Annual Meeting and Scientific Sessions April 21 – 24, 2004 Convening at the Hilton San Francisco San Francisco, CA Final Program Board of Directors President Jon Kobashigawa, MD, Los Angeles, CA President-Elect Alec Patterson, MD, St. Louis, MO Past President Stephan Schueler, MD, Newcastle, United Kingdom Secretary/Treasurer Robert C. Bourge, MD, Birmingham, AL Directors Paul A. Corris, MB, FRCP, Newcastle, United Kingdom F. Jay Fricker, MD, Gainesville, FL Katherine Hoercher, RN, Cleveland, OH Luigi Martinelli, MD, Genova, Italy Keith McNeil, MD, FRACP, Brisbane, Australia Mandeep R. Mehra, MD, New Orleans, LA Soon J. Park, MD, San Francisco, CA Hermann Reichenspurner, MD, PhD, Hamburg, Germany Bruce Rosengard, MD, FRCS, FACS, Cambridge, United Kingdom Heather J. Ross, MD, Toronto, Canada Adriana Zeevi, PhD, Pittsburgh, PA JHLT Editor James K. Kirklin, MD, Birmingham, AL Heart and Lung Transplant Registry Medical Director Marshall I. Hertz, MD, Minneapolis, MN Mechanical Circulatory Support Device Database Medical Director Mario C. Deng, MD, New York, NY Staff Amanda W. Rowe Executive Director Phyllis Glenn Assistant Executive Director Director of Membership Services Lisa Edwards Director of Meetings LeeAnn Mills Director of Operations 14673 Midway Road, Suite 200 Addison, TX 75001 Phone: 972-490-9495 Fax: 972-490-9499 www.ishlt.org [email protected] PAST PRESIDENTS 1981-1982 Michael Hess, MD 1982-1984 Jack Copeland, MD 1984-1986 Terence English, FRCS 1986-1988 Stuart Jamieson, MD 1988-1990 Bruno Reichart, MD 1990-1991 Margaret Billingham, MD 1991-1992 Christian Cabrol, MD 1992-1993 John O’Connell, MD 1993-1994 Eric Rose, MD 1994-1995 John Wallwork, FRCS 1995-1996 Sharon Hunt, MD 1996-1997 William Baumgartner, MD 1997-1998 Leslie Miller, MD 1998-1999 Alan Menkis, MD, FRCS(C) 1999-2000 Robert L. -

Historical Perspectives of Lung Transplantation: Connecting the Dots
4531 Review Article Historical perspectives of lung transplantation: connecting the dots Tanmay S. Panchabhai1, Udit Chaddha2, Kenneth R. McCurry3, Ross M. Bremner1, Atul C. Mehta4 1Norton Thoracic Institute, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA; 2Department of Pulmonary and Critical Care Medicine, Keck School of Medicine of University of Southern California, Los Angeles, CA, USA; 3Department of Cardiothoracic Surgery, Sydell and Arnold Miller Family Heart and Vascular Institute; 4Department of Pulmonary Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA Contributions: (I) Conception and design: TS Panchabhai, AC Mehta; (II) Administrative support: TS Panchabhai, RM Bremner, AC Mehta; (III) Provision of study materials or patients: TS Panchabhai, U Chaddha; (IV) Collection and assembly of data: TS Panchabhai, U Chaddha, AC Mehta; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Atul C. Mehta, MD, FCCP. Professor of Medicine, Cleveland Clinic Lerner College of Medicine, Cleveland, OH, USA; Staff Physician, Department of Pulmonary Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA. Email: [email protected]. Abstract: Lung transplantation is now a treatment option for many patients with end-stage lung disease. Now 55 years since the first human lung transplant, this is a good time to reflect upon the history of lung transplantation, to recognize major milestones in the field, and to learn from others’ unsuccessful transplant experiences. James Hardy was instrumental in developing experimental thoracic transplantation, performing the first human lung transplant in 1963. George Magovern and Adolph Yates carried out the second human lung transplant a few days later. -

HARBIN. NOVEMBER 2017. Sergio
POWER OVER LIFE AND DEATH Natalie Köhle ARBIN. NOVEMBER 2017. Sergio NESS is NOT in the BRAIN, which seeks HCanavero and Ren Xiaoping 任晓 to prove the existence of an eternal 平 announced that the world’s first hu- soul on the basis of near death experi- man head transplant was ‘imminent’. ence, as well as two guides on seducing They had just completed an eight- women. He also drops flippant refer- een-hour rehearsal on two human ca- ences to Stalin or the Nazi doctor Josef davers, and now claimed to be ready Mengele. for the real deal: the transplant of a human head from a living person with a degenerative disease onto a healthy, but brain-dead, donor body.1 Ren — a US-educated Chinese orthopaedic surgeon, was part of the team that performed the first hand transplant in Louisville in 1999. Canavero, an Italian, and former neu- rosurgeon at the university of Turin, is the more controversial, maverick per- sona of the team. In addition to many respected scientific publications, he Frankenstein’s Monster from The Bride of Frankenstein (1935) published Immortal: Why CONSCIOUS- Source: Commons Wikimedia 276 tor function and sensation. It would 277 also depend on the unproven capacity of the human brain to adjust to — and gain control over — a new body and a new nervous system without suffering debilitating pain or going mad.2 So far, Ren and Canavero have Sergio Canavero transplanted the heads of numerous Source: 诗凯 陆, Flickr lab mice and one monkey, and they Ren and Canavero see the head have also severed and subsequently Power over Life and Death Natalie Köhle transplant, formally known as cepha- mended the spinal cords of several POWER losomatic anastomosis, as the logical dogs.