Update on Tayside Wide Mental Health Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Putting Quality, Into Life
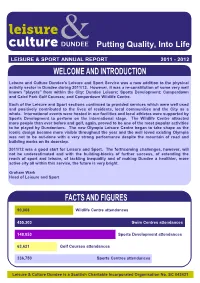
Putting Quality, Into Life LEISURE & SPORT ANNUAL REPORT 2011 - 2012 Leisure and Culture Dundee's Leisure and Sport Service was a new addition to the physical activity sector in Dundee during 2011/12. However, it was a re-constitution of some very well known "players" from within the City: Dundee Leisure; Sports Development; Camperdown and Caird Park Golf Courses; and Camperdown Wildlife Centre. Each of the Leisure and Sport sections continued to provided services which were well used and positively contributed to the lives of residents, local communities and the City as a whole. International events were hosted in our facilities and local athletes were supported by Sports Development to perform on the international stage. The Wildlife Centre attracted more people than ever before and golf, again, proved to be one of the most popular activities to be played by Dundonians. The new Olympia Leisure Centre began to take shape as the iconic design became more visible throughout the year and the well loved existing Olympia was not to be out-done with a very strong performance despite the mountain of road and building works on its doorstep. 2011/12 was a good start for Leisure and Sport. The forthcoming challenges, however, will not be underestimated and with the building-blocks of further success, of extending the reach of sport and leisure, of tackling inequality and of making Dundee a healthier, more active city all within this service, the future is very bright. Graham Wark Head of Leisure and Sport 90,068 Wildlife Centre attendances 455,303 Swim Centres attendances 148,053 Sports Development attendances 63,621 Golf Courses attendances 336,750 Sports Centres attendances Leisure & Culture Dundee is a Scottish Charitable Incorporated Organisation No. -

BMA Scotland – Guide to Information Available Through the Model Publication Scheme for GP Practices
BMA Scotland – Guide to information available through the model publication scheme for GP practices BMA Scotland – Guide to information available through the model publication scheme for GP practices Carnoustie Medical Group Guide to information available through the Scottish Information Commissioner’s Model Publication Scheme This guide was last updated on 24 July 2019 BMA Scotland – Guide to information available through the model publication scheme for GP practices Index Section 1 Introduction Section 2 About Carnoustie Medical Group Section 3 Our functions and services Section 4 How we take decisions and what we have decided Section 5 What we spend and how we spend it Section 6 Accessing information under the scheme Section 7 Information that we may withhold Section 8 Our charging policy Section 9 Our copyright policy Section 10 Our records management and disposal policy Section 11 Feedback Section 12 Complaints Section 13 How to access information which is not available under this scheme Section 14 Classes of information BMA Scotland – Guide to information available through the model publication scheme for GP practices Section 1: Introduction The Freedom of Information (Scotland) Act 2002 requires Scottish public authorities to produce and maintain a publication scheme. Authorities are under a legal obligation to: Publish the classes of information they make routinely available Tell the public how to access the information and what it might cost Carnoustie Medical Group has adopted the Model Publication Scheme produced by the Scottish Information Commissioner. The scheme will be reviewed from time to time and updated in line with guidance from the Scottish Information Commissioner. You can see the model publication scheme on the Commissioner’s website at www.itspublicknowledge.info/mps or by contacting us at the address provided below. -

New University Chancellor, Jocelyn Bell Burnell. Turn
TURN TO PAGE 8 TO READ ABOUT OUR NEW UNIVERSITY CHANCELLOR, JOCELYN BELL BURNELL. Contents Alumni Magazine 2019 University of Dundee 05 Welcome from the Principal 06 Our University in numbers 08 Introducing our Chancellor: Jocelyn Bell Burnell 11 Graduation is icing on the cake 12 Transforming the lives of children in Indonesia 14 At the movies Hello from Alumni Relations 16 Degree Show 2019 The 2019 edition of The Bridge is a mixture of fantastic stories about you, our alumni, and the excellent research that is taking 18 Building a screen against cancer place here in Dundee. As a graduate we hope you take real pride in your University and our work which is changing lives 20 Communicating science to business around the world. If you haven’t done so already, please do sign up to Dundee 22 DUSA celebrates 50 years! Connect, our exclusive mentoring and networking platform for alumni and students. From offering CV advice, to providing 24 Dundee... the best place to live, work and study information about your company, Dundee Connect is a great way to share your expertise and experience with others. We 26 By royal appointment have recently upgraded the platform and there are plans to launch a Dundee Connect app so please do watch this space. 27 Doing doctoral studies differently Like last year, we are delighted to offer you the opportunity to return to Dundee to walk down memory lane and witness all 28 Journey to success the changes that have taken place in the city in recent years. Please find more details in the centre of the magazine. -

NHS Tayside CONSULTANT PSYCHIATRIST
NHS Tayside CONSULTANT PSYCHIATRIST General Adult Psychiatry VACANCY Consultant in General Adult Psychiatry (x2 posts) Wedderburn House / Carseview Centre: Dundee Community Mental Health Team 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent NHS Tayside is looking for committed, innovative and enthusiastic Consultant Psychiatrists (full or part time) to join our Community Mental Health Team based in Dundee the ‘City of Discovery’. These posts include opportunities to see and treat a wide variety of psychiatric disorders in patients aged from eighteen to sixty-five years old, with the support of our enthusiastic and well staffed multi-disciplinary and multi- agency social work and health Community Mental Health Team with access to our 20 bed inpatient unit. We have local drug and alcohol, forensic, eating disorder, liaison and advanced intervention services as well as psychotherapy and psychology services available for our patients, and enjoy excellent relations with our local General Practitioners and voluntary service colleagues. There are many learning and training opportunities, including the teaching and supervision of 4th year medical students and Specialty Trainees attached to our team. There is a monthly continuing professional development programme and other continuing professional development will also be encouraged. Active involvement in service improvement is available through membership of our Service Improvement Group. We have close links with the University of Dundee division of Neuroscience where academic and research opportunities are available: http://medicine.dundee.ac.uk/medical-research-institute/divisions/division- neuroscience. Dundee is a coastal city on the Firth of Tay estuary in eastern Scotland. Its regenerated waterfront has the new Victoria and Albert Museum which stands on the banks of the Tay and two nautical museums: RRS Discovery, Captain Scott’s Antarctic expedition ship, and 19th-century warship, HM Frigate Unicorn. -

Colorectal Service Appointment Changes If You Need to Cancel Or Change Your Appointment Please Telephone the Number on Your Appointment Card Or Letter
After your investigations you will be informed of the results and any further management. What happens at a clinic appointment? • At the clinic you will be seen either by a Doctor or a Specialist Nurse. • You will be asked to give details about your symptoms and you will be examined. • The examination will include feeling your abdomen and possibly examination of your back passage with a gloved finger. • After your examination is over, the doctor or nurse will discuss the findings with you. It may be necessary to arrange some further investigations in order to make a diagnosis. Tayside Colorectal Service Appointment Changes If you need to cancel or change your appointment please telephone the number on your appointment card or letter. Patient Information and Advice This may allow us to give your appointment time to another patient. This document can be made available in other languages and formats on request. Contact NHS Tayside Communications Department on 01382 424138. Ninewells Hospital, Dundee Tel: 01382 632493 Developed by Colorectal Service Team Perth Royal Infirmary Tel: 01738 473610 Revised 07/2007 Review 07/2009 LN1032 Stracathro Hospital Tel: 01356 665012 The aim of this leaflet is to give you information and advice • After the procedure the doctor will discuss the findings about the Tayside Colorectal Service as your G.P. has and may arrange a further test, clinic visit or discharge referred you to further investigate your bowel symptoms. you back to the care of your G.P. What happens next? Your G.P. will be sent a copy of the report. -

National System for Sexual Health (Nash)
National System for Sexual Health (NaSH) Protecting your Personal Information How do you protect my personal information? NHS Scotland cares about your personal data and it’s important that you know how we use it and keep it safe. We use a computer system, just for sexual health clinics in Scotland, called ‘NaSH’. You may be asked to complete a registration form so we can create an electronic record using your personal details. Some people will register directly through our on-line booking site. We prefer to download your name and address details electronically, using your NHS Scotland number (CHI number), as this saves time and reduces errors. The registration form will record your permission to use CHI. You can also choose to use an assumed (‘made-up’) name and not use your CHI number but please be aware that we would not be able to refer you for any x-ray investigations or communicate with your GP or other health professional under an assumed name. You will be given a sexual health clinic number called a ‘NaSH number’ which starts with ‘AN’ (e.g. AN012345678). Please keep this number safe as it may be required to access your test results. You can use this number to access care in any specialist sexual health clinic in NHS Scotland. We are committed to protecting your privacy and will only process personal confidential data in accordance with the Data Protection Act 2018. Who can access the NaSH system and my personal information? The NaSH system can only be accessed by staff working under the oversight of specialist sexual health and HIV services in Scotland who have a legal duty to keep information about you confidential. -

Foi202000130010
The First Minister’s 2019 Christmas Card Project will benefit the following charities: Marine Conservation Society Glasgow & Clyde Rape Crisis Friends of Victoria & Whyteman’s Brae Hospitals Celebrated and named as one of the 100 Greatest Singers of All Time by Rolling Stone Magazine, Annie Lennox’s iconic musical career spans over four decades. Her collaboration with partner Dave Stewart formed Eurythmics in the early ‘80s. Lennox has also enjoyed a widely acclaimed solo career, selling over 83 million albums worldwide altogether. In 2012, Annie Lennox was awarded the Order of the British Empire for her work towards the eradication of AIDS and poverty in Africa. She is a Royal Academician, a respected social activist and philanthropist, and the first female Chancellor of Glasgow Caledonian University. Her work in the visual arts has included an exhibition at the Victoria and Albert Museum, London; ‘The House of Annie Lennox’ which travelled to Manchester, Aberdeen; and The National Portrait Gallery of Edinburgh. Her installation ‘Now I Let You Go’… is currently exhibited at Massachusetts Museum of Contemporary Art. Annie has been awarded the Royal Scottish Geographical Society’s ‘Livingstone Medal’ and, in 2017, her philanthropic work was honoured with the George Harrison Global Citizen Award, and a second prestigious German Sustainability Award. Merry Christmas and a Happy New Year Nollaig Chridheil agus Bliadhna Mhath Ùr Season’s Greetings Beannachdan aig àm na Nollaige The Rt Hon Nicola Sturgeon MSP and Mr Peter Murrell Bute ButeHouse, -

NHS Guidlines
NHSScotland Identity guidelines Identikit Introduction In December 2000, Susan Deacon MSP, In this publication, the Minister said: “The public relate to and recognise Minister for Health and Community Care, the NHS. They believe their care is launched ‘Our National Health: provided by a national health service and staff take pride in the fact that a plan for action, a plan for change’ they work for the NHS. Research tells us that the variety of differently which set out a clear direction for the NHS named NHS bodies confuses the in Scotland with the aims of improving public and alienates staff. As part of our proposals to rebuild the National people’s health and creating a 21st century Health Service we will promote a new identity for the NHS in Scotland.” health service. The guidelines that follow provide an essential design toolkit to establish “Alongside the changes in NHS this new identity. The guidelines cover signage, vehicles, uniforms, stationery, boardrooms, we will re-establish literature, forms and other items. The a national identity for the aim is to replace, over time, the array of existing identities within NHS NHS in Scotland.” organisations with the single NHS identity while avoiding wastage and unnecessary expenditure. Our National Health: a plan for action, a plan for change section 3/page 31 2 Contents Section 1 Our national identity 4 Exclusion zone 6 Minimum size 6 Section 2 Identity structure 7 Essential elements 9 Identity variants 10 Caring device 12 Positioning the identity 14 Other identities 15 Working in partnership 16 Section 3 Identities for ideas & initiatives 17 Initiatives 18 Section 4 NHSScotland typefaces 19 Stone Sans 20 Arial 24 Garamond 25 Times New Roman 26 Literature 27 Section 5 Colour 28 Using colour 29 Primary colours 30 Colour palette 31 Tints 32 Printing the identity 33 3 Section One Our national identity Together, the initials ‘NHS’ and the caring symbol form the foundations of our identity. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

Consultant in Trauma and Orthopaedics, Perth Royal Infirmary
Consultant in Trauma and Orthopaedics, Perth Royal Infirmary Information Pack Closing date: 21 November 2019 Reference: AR.25.19 Welcome from Grant Archibald, Chief Executive, NHS Tayside Thank you for your interest in this post. As you’ll see we have put together some information on this site both about NHS Tayside and where we are located in Scotland. I hope that you find this useful and that you translate your interest in this post into a formal application. NHS Tayside has a strong track record in delivering high-quality, safe and effective care for all our patients. However, like other NHS Boards across Scotland, NHS Tayside is facing significant challenges including growing demand for all services, workforce challenges that are impacting upon how we deliver services and continuing pressures on our finances. In response to these challenges, NHS Tayside has embarked up on a programme of transformation to ensure that services are safe, affordable and, importantly, sustainable for the future. Transforming Tayside aims to deliver Better Health, Better Care, Better Workplace and Better Value for the population of Tayside. The programme is clinically-led and is being delivered in partnership with our staff and trades unions and our local health and social care partnerships. It is structured to respond to issues and make changes to services in the short to medium-term, as well as presenting an ambitious vision of transformation for Tayside in the longer term. It will provide clear and credible choices for transforming the future of local healthcare. A new, innovative leadership model for clinical directorates is now in place to drive the changes necessary in health and social care across the whole system. -

NHS Tayside's Draft One Year Operational Delivery Plan 2017-18
DRAFT One Year Operational Delivery Plan 2017-2018 Operational Delivery Plan | 2017-2018 Section Item Page 1 Introduction 3 2 Our Strategic Context 4 3 Partnership, Values and Culture 5 4 Clinical Strategy, Quality, Safety & Governance 7 5 Planning Assumptions 9 6 Our Programme of Transformation 10 7 Service Plans 12 Primary Care 12 Medicines Management 14 Planned Care 17 Unscheduled Care 23 Mental Health 30 Older People 32 Women and Child Health 35 Cancer 37 Support Services 40 Estates and Infrastructure 43 8 Workforce 45 9 eHealth 49 10 Financial Plan 50 11 Property Asset Disposal 56 12 Communications and Engagement 57 2 NHS Tayside People Matter Strategy | 2016-2021 1 Introduction NHS Tayside provides high-quality health services quality standards to a high level. Our plan for from a number of acute and community sites and 2017-18 responds to the regional and national in people’s own homes. This document summarises context and the drivers of the Health and Social our Operational Plan for 2017-18, setting out the Care Delivery Plan, the National Clinical Strategy, actions we will take over the next year to improve Realising Realistic Medicine and the benchmarking the quality, safety and cost-effectiveness of our data provided by Scottish Government to all health services and ensure we remain resilient in light of boards relating to productive opportunities. the challenges we face. We acknowledge that we will need the continued The one-year plan has been developed within the support of Scottish Government with tailored context of our five-year Transformation Programme support to achieve the challenging objectives set out for Tayside. -

Newsletter February 2019
Newsletter February 2019 Call for Evidence Over 200 people have submitted written documents/personal statements to the Inquiry team and there have been 61 oral evidence sessions. Volunteers from both the Dundee and Perth Samaritans have supported almost all of the oral evidence sessions which were held in the Inquiry offices in Springfield, Dundee. Evidence has been submitted to the Inquiry from patients, families, carers, NHS employees and third sector organisations. The Inquiry team have also been to take evidence in Carseview, Rohallion Forensic Psychiatric Hospital, Murray Royal Infirmary, Whitehills Community Hospital (Forfar), Stracathro Hospital, Perth Royal Infirmary, HMP Perth and individuals’ homes. Evidence has also been submitted from Police Scotland (Tayside Division), Universities Student Welfare Teams (counselling and mental health support services), Dundee Fairness Commission, Dundee Drugs Commission, Scottish Government Suicide Prevention Strategy Leadership Group, and third sector organisations such as Support in MIND and Voluntary Health Scotland. A significant piece of work was undertaken September-November 2018 by the Health and Social Care Alliance Scotland (ALLIANCE), who held focus groups around the whole of the NHS Tayside region to capture the voices of those with lived experience of mental health provision in Tayside. Their report is available here: https://www.alliance-scotland.org.uk/blog/resources/independent-inquiry-into-mental-health-services-in-tayside- hearing-the-voices-of-people-with-lived-experience/ The Alliance have continued to manage the Stakeholder Participation Group (SPG), and have submitted evidence to the Inquiry on behalf of individuals. The Employee Participation Group (EPG) conducted an online staff survey during November and December and held focus group meetings for all those employed to work in NHS Tayside mental health services.