SGLT2 Inhibitors: a Review of Their Antidiabetic and Cardioprotective Effects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

Therapeutic Medications Against Diabetes: What We Have and What We Expect
Advanced Drug Delivery Reviews 139 (2019) 3–15 Contents lists available at ScienceDirect Advanced Drug Delivery Reviews journal homepage: www.elsevier.com/locate/addr Therapeutic medications against diabetes: What we have and what we expect Cheng Hu a,b, Weiping Jia a,⁎ a Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Key Clinical Center for Metabolic Diseases, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, 600 Yishan Road, Shanghai 200233, People's Republic of China b Shanghai Jiao Tong University Affiliated Sixth People's Hospital South Campus, 6600 Nanfeng Road, Shanghai 200433, People's Republic of China article info abstract Article history: Diabetes has become one of the largest global health and economic burdens, with its increased prevalence and Received 28 June 2018 high complication ratio. Stable and satisfactory blood glucose control are vital to reduce diabetes-related compli- Received in revised form 1 September 2018 cations. Therefore, continuous attempts have been made in antidiabetic drugs, treatment routes, and traditional Accepted 27 November 2018 Chinese medicine to achieve better disease control. New antidiabetic drugs and appropriate combinations of Available online 5 December 2018 these drugs have increased diabetes control significantly. Besides, novel treatment routes including oral antidia- betic peptide delivery, nanocarrier delivery system, implantable drug delivery system are also pivotal for diabetes Keywords: fi Diabetes control, with its greater ef ciency, increased bioavailability, decreased toxicity and reduced dosing frequency. Treatment Among these new routes, nanotechnology, artificial pancreas and islet cell implantation have shown great poten- Drug delivery tial in diabetes therapy. Traditional Chinese medicine also offer new options for diabetes treatment. -

Dapagliflozin – Structure, Synthesis, and New Indications
Pharmacia 68(3): 591–596 DOI 10.3897/pharmacia.68.e70626 Review Article Dapagliflozin – structure, synthesis, and new indications Stefan Balkanski1 1 Bulgarian Pharmaceutical Union, Sofia, Bulgaria Corresponding author: Stefan Balkanski ([email protected]) Received 24 June 2021 ♦ Accepted 4 July 2021 ♦ Published 4 August 2021 Citation: Balkanski S (2021) Dapagliflozin – structure, synthesis, and new indications. Pharmacia 68(3): 591–596.https://doi. org/10.3897/pharmacia.68.e70626 Abstract Dapagliflozin is a sodium-glucose co-transporter-2 (SGLT2) inhibitors used in the treatment of patients with type 2 diabetes. An aryl glycoside with significant effect as glucose-lowering agents, Dapagliflozin also has indication for patients with Heart Failure and Chronic Kidney Disease. This review examines the structure, synthesis, analysis, structure activity relationship and uses of the prod- uct. The studies behind this drug have opened the doors for the new line of treatment – a drug that reduces blood glucoses, decreases the rate of heart failures, and has a positive effect on patients with chronic kidney disease. Keywords Dapagliflozin, SGLT2-inhibitor, diabetes, heart failure Structure of dapagliflozin against diabetes (Lee et al. 2005; Lemaire 2012; Mironova et al. 2017). Embodiments of (SGLT-2) inhibitors include C-glycosides have a remarkable rank in medicinal chemis- dapagliflozin, canagliflozin, empagliflozin and ipragliflozin, try as they are considered as universal natural products shown in Figure 1. It has molecular formula of C24H35ClO9. (Qinpei and Simon 2004). Selective sodium-dependent IUPAC name (2S,3R,4R,5S,6R)-2-[4-chloro-3-[(4- glucose cotransporter 2 (SGLT-2) inhibitors are potent ethoxyphenyl)methyl]phenyl]-6-(hydroxymethyl)oxa- medicinal candidates of aryl glycosides that are functional ne-3,4,5-triol;(2S)-propane-1,2-diol;hydrate. -

Think Medicines!
Think Issue 13 August 2016 MHRA Drug Safety SGLT2 inhibitors: updated advice on the risk of diabetic Medicines!Updates can be found ketoacidosis (DKA) at the following link. The MHRA are advising health care professionals to test for raised ketones in patients with ketoacidosis symptoms, who are taking SGLT2 inhibitors even if New higher strength Humalog® plasma glucose levels are near-normal. SGLT2 inhibitors include: Canagliflozin, 200 units/ml KwikPen™ Dapagliflozin and Empagliflozin. Serious, life-threatening, and fatal cases of In order to minimize medication DKA have been reported in patients taking an SGLT2 inhibitor. In several cases, errors. blood glucose levels were only moderately elevated (e.g. <14mmol/L) Insulin lispro 200 units/ml representing an atypical presentation for DKA, which could delay diagnosis and solution for injection should treatment. ONLY be administered using the Advice for health Care Professionals: Humalog 200 units/ml pre-filled Inform patients of the signs of diabetic ketoacidosis (DKA) and advise them to pen (KwikPen). seek immediate medical advice if they develop any of these symptoms (e.g. When switching from one rapid weight loss, feeling sick or being sick, stomach pain, fast and deep Humalog strength to another, breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the dose does not need to be the mouth, or a different odour to urine or sweat). converted. Unnecessary dose Discuss the risk factors of DKA with patients. conversion may lead to under/ Discontinue treatment with the SGLT2 inhibitor immediately if DKA is over dosing and resultant hyper/ suspected or diagnosed. -

Steglujan, INN-Ertugliflozin-Sitagliptin
25 January 2018 EMA/86941/2018 Committee for Medicinal Products for Human Use (CHMP) Assessment report Steglujan International non-proprietary name: ertugliflozin / sitagliptin Procedure No. EMEA/H/C/004313/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 7 1.1. Submission of the dossier ...................................................................................... 7 1.2. Steps taken for the assessment of the product ......................................................... 8 2. Scientific discussion ................................................................................ 9 2.1. Problem statement ............................................................................................... 9 2.1.1. Disease or condition ........................................................................................... 9 2.1.2. Epidemiology .................................................................................................... 9 2.1.3. Clinical presentation .......................................................................................... -

Role of Apple Phytochemicals, Phloretin and Phloridzin, in Modulating Processes Related to Intestinal Inflammation
nutrients Article Role of Apple Phytochemicals, Phloretin and Phloridzin, in Modulating Processes Related to Intestinal Inflammation Danuta Zielinska 1, José Moisés Laparra-Llopis 2, Henryk Zielinski 3, Dorota Szawara-Nowak 3 and Juan Antonio Giménez-Bastida 3,4,* 1 Department of Chemistry, University of Warmia and Mazury, 10-727 Olsztyn, Poland; [email protected] 2 Group of Molecular Immunonutrition in Cancer, Madrid Institute for Advanced Studies in Food (IMDEA-Food), 28049 Madrid, Spain; [email protected] 3 Institute of Animal Reproduction and Food Research, Department of Chemistry and Biodynamics of Food, Polish Academy of Science, 10-748 Olsztyn, Poland; [email protected] (H.Z.); [email protected] (D.S.-N.) 4 Group on Quality, Safety and Bioactivity of Plant Foods, Centro de Edafología y Biología Aplicada del Segura (CSIC), 30100 Murcia, Spain * Correspondence: [email protected] Received: 25 April 2019; Accepted: 23 May 2019; Published: 25 May 2019 Abstract: Plant-derived food consumption has gained attention as potential intervention for the improvement of intestinal inflammatory diseases. Apple consumption has been shown to be effective at ameliorating intestinal inflammation symptoms. These beneficial effects have been related to (poly)phenols, including phloretin (Phlor) and its glycoside named phloridzin (Phldz). To deepen the modulatory effects of these molecules we studied: i) their influence on the synthesis of proinflammatory molecules (PGE2, IL-8, IL-6, MCP-1, and ICAM-1) in IL-1β-treated myofibroblasts of the colon CCD-18Co cell line, and ii) the inhibitory potential of the formation of advanced glycation end products (AGEs). -

IHS PROVIDER September 2017
September 2017 Volume 42 Number 9 Indian Health Service National Pharmacy and Therapeutics Committee SGLT-2 inhibitors (Update) NPTC Formulary Brief August Meeting 2017 Background: The FDA has currently approved three SGLT-2 inhibitors, two of which have completed FDA-mandated cardiovascular outcomes trials. Last year, in the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG), empagliflozin not only reduced cardiovascular events, but also mortality.1 This year, the Canagliflozin Cardiovascular Assessment Study (CANVAS) demonstrated equivocal cardiovascular benefits, no mortality benefit, and significant harms in those receiving canagliflozin.2 The DECLARE-TIMI 58 cardiovascular study of dapagliflozin will be completed in April 2019 (ClinicalTrials.gov Identifier: NCT01730534). Uncertainty remains regarding the current data, long- term benefits and harms, and differentiation among SGLT-2 inhibitors. Following a review of SGLT2 inhibitors at the August 2017 NPTC meeting on their cardiovascular outcomes, net benefit and place in therapy, no modifications were made to the National Core Formulary (NCF). Discussion: EMPA-REG enrolled 7,020 patients with Type 2 diabetes mellitus (T2DM) and HgbA1c values between 7.0-10.0%. All patients had established cardiovascular disease (CVD) and were observed for a median duration of 3.1 years. Empagliflozin reduced the primary outcome of cardiovascular (CV) death, nonfatal myocardial infarction (MI), or nonfatal cardiovascular accident (CVA) by 6.5 events per 1000 patient-years (pt-yrs). Mortality decreased by 9.2 events per 1000 pt-yrs, primarily driven by a reduction in CV mortality of 7.8 events per 1000 pt-yrs. Heart failure hospitalization decreased by 5.1 events per 1000 pt-yrs. -

Natural Products As Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors
Reviews Natural Products as Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors Author ABSTRACT Wolfgang Blaschek Glucose homeostasis is maintained by antagonistic hormones such as insulin and glucagon as well as by regulation of glu- Affiliation cose absorption, gluconeogenesis, biosynthesis and mobiliza- Formerly: Institute of Pharmacy, Department of Pharmaceu- tion of glycogen, glucose consumption in all tissues and glo- tical Biology, Christian-Albrechts-University of Kiel, Kiel, merular filtration, and reabsorption of glucose in the kidneys. Germany Glucose enters or leaves cells mainly with the help of two membrane integrated transporters belonging either to the Key words family of facilitative glucose transporters (GLUTs) or to the Malus domestica, Rosaceae, Phlorizin, flavonoids, family of sodium glucose cotransporters (SGLTs). The intesti- ‑ SGLT inhibitors, gliflozins, diabetes nal glucose absorption by endothelial cells is managed by SGLT1, the transfer from them to the blood by GLUT2. In the received February 9, 2017 kidney SGLT2 and SGLT1 are responsible for reabsorption of revised March 3, 2017 filtered glucose from the primary urine, and GLUT2 and accepted March 6, 2017 GLUT1 enable the transport of glucose from epithelial cells Bibliography back into the blood stream. DOI http://dx.doi.org/10.1055/s-0043-106050 The flavonoid phlorizin was isolated from the bark of apple Published online April 10, 2017 | Planta Med 2017; 83: 985– trees and shown to cause glucosuria. Phlorizin is an inhibitor 993 © Georg Thieme Verlag KG Stuttgart · New York | of SGLT1 and SGLT2. With phlorizin as lead compound, specif- ISSN 0032‑0943 ic inhibitors of SGLT2 were developed in the last decade and some of them have been approved for treatment mainly of Correspondence type 2 diabetes. -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -
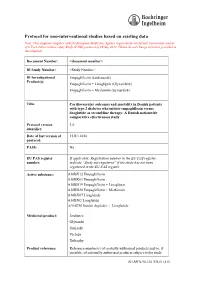
Protocol for Non-Interventional Studies Based on Existing Data
ABCD TITLE PAGE Protocol for non-interventional studies based on existing data TITLE PAGE Note: This template complies with the European Medicines Agency requirements on format, layout and content of a Post Authorisation safety Study (PASS) protocol of 26 Sep 2012. Please do not change structure provided in this template. Document Number: <document number> BI Study Number: <Study Number> BI Investigational Empagliflozin (Jardiance®) Product(s): Empagliflozin + Linagliptin (Glyxambi®) Empagliflozin + Metformin (Synjardy®) Title: Cardiovascular outcomes and mortality in Danish patients with type 2 diabetes who initiate empagliflozin versus liraglutide as second-line therapy: A Danish nationwide comparative effectiveness study Protocol version 1.0 identifier: Date of last version of 15JUL2018 protocol: PASS: No EU PAS register If applicable: Registration number in the EU PAS register; number: indicate “Study not registered” if the study has not been registered in the EU PAS register Active substance: A10BX12 Empagliflozin A10BK03 Empagliflozin A10BD19 Empagliflozin + Linagliptin A10BD20 Empagliflozin + Metformin A10BX07 Liraglutide A10BJ02 Liraglutide A10AE56 Insulin degludec + Liraglutide Medicinal product: Jardiance Glyxambi Synjardy Victoza Xultophy Product reference: Reference number(s) of centrally authorised products and/or, if possible, of nationally authorised products subject to the study 001-MCS-90-124_RD-01 (4.0) Boehringer Ingelheim Page 2 of 55 Protocol for non-interventional studies based on existing data BI Study Number <Study Number> <document number> Proprietary confidential information © 2019 Boehringer Ingelheim International GmbH or one or more of its affiliated companies Procedure number: If applicable, Agency or national procedure number(s), e.g. EMA/X/X/XXX Joint PASS: No Research question and To compare, among patients with type 2 diabetes in Denmark, objectives: clinical outcomes among new users (initiators) of empagliflozin versus liraglutide. -

Steglujan (Ertugliflozin/Sitagliptin), Segluromet
Steglatro™ (ertugliflozin), Steglujan™ (ertugliflozin/sitagliptin), Segluromet™ (ertugliflozin/metformin) – New drug approval • On December 19, 2017, the FDA approved Merck’s Steglatro (ertugliflozin), Steglujan (ertugliflozin/sitagliptin), and Segluromet (ertugliflozin/metformin) as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). — Steglujan is indicated when treatment with both ertugliflozin and sitagliptin is appropriate. — Segluromet is indicated when patients are not adequately controlled on a regimen containing ertugliflozin or metformin, or in patients who are already treated with both ertugliflozin and metformin. — These drugs are not recommended in patients with type 1 diabetes mellitus (T1DM) or for the treatment of diabetic ketoacidosis. — Steglujan has not been studied in patients with a history of pancreatitis. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using Steglujan. • Ertugliflozin is the fourth sodium-glucose co-transoporter-2 (SGLT2) inhibitor approved by the FDA. Other marketed SGLT2 inhibitors include Jardiance® (empagliflozin), Farxiga® (dapagliflozin), and Invokana® (canagliflozin). • The efficacy and safety of ertugliflozin were evaluated in multiple clinical studies involving patients with T2DM. Ertugliflozin was studied as monotherapy and in combination with metformin and/or a dipeptidyl peptidase 4 (DPP-4) inhibitor. Ertugliflozin was also studied in combination with other antidiabetic medications, including insulin and a sulfonylurea, and in T2DM patients with moderate renal impairment. — In patients with T2DM, treatment with ertugliflozin, ertugliflozin + sitagliptin, and ertugliflozin + metformin reduced hemoglobin A1c (HbA1c) vs. placebo or the active comparator. — In patients with T2DM and moderate renal impairment, treatment with ertugliflozin did not result in a reduction in HbA1c vs. -

Qtern (Dapagliflozin/Saxagliptin) – New Drug Approval
Qtern® (dapagliflozin/saxagliptin) – New drug approval • On February 28, 2017, AstraZeneca announced the FDA approval of Qtern (dapagliflozin/saxagliptin) as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM) who have inadequate control with Farxiga® (dapagliflozin) or who are already treated with dapagliflozin and Onglyza® (saxagliptin). • Qtern is not indicated for the treatment of type 1 diabetes mellitus or diabetic ketoacidosis, and it should only be used in patients who tolerate 10 mg of dapagliflozin. • Qtern combines two anti-hyperglycemic agents, dapagliflozin, a sodium-glucose co-transporter 2 (SGLT-2) inhibitor, and saxagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor. • The efficacy of Qtern was evaluated in a study of 315 T2DM patients. Patients were randomized to saxagliptin or placebo, in combination with dapagliflozin and metformin. — Patients treated with add-on saxagliptin therapy had significantly greater reductions in HbA1c from baseline vs. the placebo group (-0.5% vs. -0.2%, respectively; difference between groups in HbA1c: -0.4%, p < 0.0001). — The proportion of patients achieving HbA1c < 7% at week 24 was 35.3% in the saxagliptin group vs. 23.1% in the placebo group. • Qtern is contraindicated in patients with a history of a serious hypersensitivity reaction to dapagliflozin or to saxagliptin (eg, anaphylaxis, angioedema or exfoliative skin conditions), and in patients with moderate to severe renal impairment (eGFR < 45 mL/min/1.73 m2), end-stage renal disease, or on dialysis. • Warnings and precautions of Qtern include pancreatitis, heart failure, hypotension, ketoacidosis, acute kidney injury and impairment in renal function, urosepsis and pyelonephritis, hypoglycemia with concomitant use of insulin or insulin secretagogues, genital mycotic infections, increases in low- density lipoprotein cholesterol, bladder cancer, severe and disabling arthralgia, and bullous pemphigoid.