The Practice of Medicine II Academic Year 2011-2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -
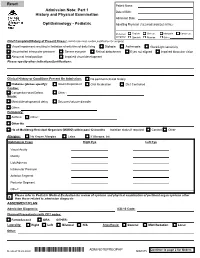
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Prevalence of Diastasis of the Rectus Abdominis Muscles Immediately Postpartum: Comparison Between Primiparae and Multiparae
ISSN 1413-3555 Rev Bras Fisioter, São Carlos, v. 13, n. 4, p. 275-80, jul./ago. 2009 ARTIGO ORIGIN A L ©Revista Brasileira de Fisioterapia Prevalência de diástase dos músculos retoabdominais no puerpério imediato: comparação entre primíparas e multíparas Prevalence of diastasis of the rectus abdominis muscles immediately postpartum: comparison between primiparae and multiparae Rett MT1,2, Braga MD2, Bernardes NO1,2, Andrade SC2 Resumo Objetivos: Verificar a prevalência da diástase dos músculos retoabdominais (DMRA) em primíparas e multíparas no pós-parto vaginal imediato, comparar a DMRA supraumbilical e infraumbilical e correlacioná-las com a idade materna, o índice de massa corporal (IMC), a idade gestacional (IG) e o tempo de trabalho de parto (TTP). Métodos: Foi realizado um estudo transversal, sendo registradas informações pessoais, antecedentes obstétricos e a DMRA supra e infraumbilical. Os pontos de medida foram 4,5 cm acima e abaixo da cicatriz umbilical, sendo graduada pelo número de dedos entre as bordas mediais dessa musculatura. Para cada dedo, foi estimado 1,5 cm. A DMRA foi considerada presente e relevante quando houvesse um afastamento >2 cm na região supra e/ou infraumbilical. Resultados: Foram analisadas 467 fichas de dados, sendo a prevalência da DMRA supraumbilical >2 cm de 68% e infraumbilical de 32%. A prevalência supraumbilical entre as primíparas e multíparas foi idêntica (68%) e infraumbilical maior nas multíparas (19,8% e 29,2%). As médias da DMRA foram 2,8 (±1,2) cm supraumbilical e 1,5 (±1,1) cm infraumbilical, apresentando diferença significativa (p=0,0001) e fraca correlação (r=0,461). A média da DMRA infraumbilical foi significativamente maior nas multíparas (p<0,018). -

Physical Therapy Assessment
Physical Therapy Assessment Patient Name __________________________________________ Sex M F Date _________________ First MI Last MM / DD / YYYY DOB______________ What are your goals? _____________________________________________________ MM / DD / YYYY Medical History Have you been admitted to the Emergency Room in the past year? Yes No When? __________________________________________________________________________________ Have you been admitted to the Hospital in the past year?Yes No When? __________________________________________________________________________________ History or broken bones, fractures?Yes No When and Where?________________________________________________________________________ Do you experience Headaches?Yes No How long do they last? ____________________ How often do you have them? ____________________ What makes them worse? __________________________ What helps? __________________________ Have you had any surgical procedure(s) performed? Yes No When? __________________________________________________________________________________ Describe the surgery: _____________________________________________________________________ Have you experienced head trauma including concussion, traumatic brain injury, whiplash? Yes No When? __________________________________________________________________________________ Describe what happened: _________________________________________________________________ Have you ever been in a car accident? Yes No When? __________________________________________________________________________________ -

Abdominoplasty Sur716.002 ______Coverage
ABDOMINOPLASTY SUR716.002 ______________________________________________________________________ COVERAGE: Abdominoplasty and/or removal of the overhanging lower abdominal panniculus are considered cosmetic procedures. Abdominoplasty is sometimes described as a wide internal oblique transverse abdominous plication (a wide rectus plication). No coverage is available for these procedures or for repair of a diastasis recti in the absence of a true midline hernia (ventral or umbilical). On rare occasions, abdominoplasty may be considered for coverage with determination of medical necessity for indications such as the following: · in an older individual who has such a significantly large panniculus as to interfere with the ability to walk normally or in a patient with documented pressure sores, rash, or intertriginous maceration that has not responded to all manners of conservative treatment, or · in an individual who has had multiple operations with spreading of the scar associated with diastasis recti and a true incisional hernia defect. NOTE: The presence of back pain alone without one of the preceding indications will not constitute medical necessity for abdominoplasty. ______________________________________________________________________ DESCRIPTION: Abdominoplasty is a plastic repair of the anterolateral abdominal wall, which is largely muscular and aponeurotic (a white flattened or ribbon-like tendonous expansion serving mainly to connect a muscle with the parts that it moves), with overlying subcutaneous tissue and skin. Abdominal wall pathophysiology concerns weakness or laxity of the abdominal wall musculature. This prevents maximum force generation with contraction and weakens the support of the lumber dorsal fascia with resultant back pain. An excess of ten pounds of adipose tissue in the abdominal wall adds 100 pounds of strain on the discs of the lower back by exaggeration of the normal S curve of the spine. -

F110 Genetics Physical Exam, Part II
Bench to Bassinet Pediatric Cardiac Genomics Consortium: CHD GENES Form 110: Genetics Physical Exam - Part II Version: C - 06/22/2011 SECTION A: ADMINISTRATIVE INFORMATION F1 Skin A1. Study Identification Number: F2 Chest F3 Inter A2. Study Visit: Proband Subject Baseline Visit F4 Nippl A3. Date Form Completed: MM/DD/YYYY F5 Chest F6 Abdo SECTION F: SKIN, CHEST, ABDOMEN, AND BACK F7 Back Normal Abnormal Unknown Source G1 Genit Pending H1 Hand F1. Skin: I1 Feet a. Ashleaf spots J1 Neuro b. Café-au-lait spots c. Cutis marmata d. Hemangioma e. Hyperkeratosis f. Hyperpigmented lesions g. Hypopigmented lesions h. Lipoma i. Port wine spots j. Skin tag k. Telangiectasia l. Other i. If Other, specify: F2. Chest circumference: cm F3. Inter-Nipple Distance (IND): cm Normal Wide Closely Unknown Source Spaced Spaced Pending Nipples Nipples F4. Nipples: Normal Abnormal Unknown Source Pending F5. Chest: a. Barrel b. Absent/ hypoplastic clavicles c. Narrow d. Supernumerary Nipples e. Absent pectoralis muscle f. Pectus Carinatum g. Pectus Excavatum h. Absent Ribs i. Supernumerary Ribs j. Short k. Other i. If Other, specify: Normal Abnormal Unknown Source Pending F6. Abdomen: a. Abdominal Mass b. Diastasis recti c. Gastroschisis d. Inguinal Hernia e. Umbilical Hernia f. Left-sided Liver g. Midline Liver h. Omphalocele i. Splenomegaly j. Other i. If Other, specify: Normal Abnormal Unknown Source Pending F7. Back: a. Kyphosis b. Meningomyelocele c. Sacral Dimple d. Scoliosis e. Winged Scapula Unilateral Bilateral No f. Other i. If Other, specify: SECTION G: GENITOURINARY (HISTORY OF OR PRESENT) Normal Abnormal Unknown Source Pending G1. -

Diastasis Recti
In This Chapter Benefits and Risks of Exercise During Pregnancy Maternal Fitness Gestational Diabetes Preeclampsia Maternal Obesity Maternal Exercise and the Fetal Response Contraindications and Risk Factors Physiological Changes During Pregnancy Musculoskeletal System Cardiovascular System Respiratory System Thermoregulatory System Programming Guidelines and Considerations for Prenatal Exercise Biomechanical Considerations for the Pregnant Mother Low-back and Posterior Pelvic Pain Pubic Pain Carpal Tunnel Syndrome Diastasis Recti About The Author Stress Urinary Incontinence Sabrena Merrill, M.S., has been actively involved in the fitness Nutritional Considerations industry since 1987. An ACE-certified Group Fitness Instructor Psychological Considerations and Personal Trainer, Merrill teaches group exercise, owns and Benefits and Risks of Exercise Following Pregnancy operates her own personal training business, has managed Physiological Changes Following fitness departments in commercial facilities, and lectured to Pregnancy university students and established fitness professionals. She Programming Guidelines and Considerations for Postnatal has a bachelor’s degree in exercise science as well as a master’s Exercise degree in physical education from the University of Kansas, and Biomechanical Considerations for the Lactating Mother has numerous certifications in exercise instruction. Merrill acts Case Study as a spokesperson for the American Council on Exercise (ACE) Summary and is involved in curriculum development for ACE continuing education programs. Additionally, Merrill presents lectures and workshops to fitness professionals nationwide. CHAPTER 23 Pre- and Postnatal Exercise Sabrena Merrill n increasing amount of research on exercise in pregnancy has led to a waning debate over the maternal and fetal risks of regular physical activity during pregnancy. There is a growing trend of women entering pregnancy with regu- Alar aerobic and strength-conditioning activities as a part of their daily routines. -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -

Phase 4 Medicine Intended Learning Outcomes (Ilos)
Phase 4 Medicine Intended Learning Outcomes (ILOs) This Phase 4 document outlines the listed ILOs for Medicine. This will be examined in the Year 4 and Year 5 summative written examinations. It is important that we impress upon you the limitation of any ILOs in their application to a vocational professional course such as medicine. ILOs may be useful in providing a ‘shopping list’ of conditions that you will be expected to describe and anticipate. The depth and extent of your knowledge of each condition will be a joint function of the condition’s frequency and its gravity. Please use the ILOs to make sure you are familiar with the common and important presentations and conditions. The list does not comprise of the entire coda for successful medical practice but will provide you with a solid platform from which to build upon. More detailed explanations and outlines will be available in the standard textbooks. Any elucidation or expansion can be obtained there. Even more important is the point that ILOs will point you in the correct direction to pass our written exam, but that this is only part of the story. ILOs will point you in the correct direction to pass our written exam, but that this is only part of the story. Final exams function as ‘objective proof’ for the general public that you have enough knowledge to function as a doctor. As you will see during your time on the wards, however, being a doctor requires much more than knowledge; as well as being able to imitate and build on the activities you witness in your clinical placements, it is imperative that you acquire skills, behaviours, specific attitudes, and commitment to your patients’ well being. -

Alpha Thalassemia
Alpha Thalassemia Alpha thalassemia is a genetic disorder called a hemoglobinopathy, or an inherited type of anemia. People who have alpha thalassemia make red blood cells that are not able to carry oxygen as well throughout the body, which can lead to anemia. This chronic anemia can include pale skin, fatigue, and weakness. In more severe cases, people with alpha thalassemia can also develop jaundice (yellowing of the eyes and skin), heart defects, and an enlarged liver and spleen (called hepatosplenomegaly). Alpha thalassemia is more common in people of African, Southeast Asian, Chinese, Middle Eastern, and Mediterranean ancestries. Causes We have over 20,000 different genes in the body. These genes are like instruction manuals for how to build a protein, and each protein has an important function that helps to keep our body working how it should. The HBA1 and HBA2 genes make a protein called alpha-globin. Two of the alpha-globin proteins combine with two other proteins called beta-globins (which are made by the HBB gene) to make a normal red blood cell. Most people have four copies of the genes that make the alpha-globin protein: two copies of the HBA1 gene (one from each parent), and two copies of the HBA2 gene (one from each parent). Having all four copies of these genes is symbolized by writing αα/αα. Whether or not someone has alpha thalassemia depends on how many working copies of the alpha- globin gene they have (if someone has a missing or nonworking alpha-globin gene, it is most frequently caused by a deletion): Silent alpha thalassemia carrier (also referred to as -α/αα): When there is one missing alpha-globin gene. -

Hypersphere Anonymous
Hypersphere Anonymous This work is licensed under a Creative Commons Attribution 4.0 International License. ISBN 978-1-329-78152-8 First edition: December 2015 Fourth edition Part 1 Slice of Life Adventures in The Hypersphere 2 The Hypersphere is a big fucking place, kid. Imagine the biggest pile of dung you can take and then double-- no, triple that shit and you s t i l l h a v e n ’ t c o m e c l o s e t o o n e octingentillionth of a Hypersphere cornerstone. Hell, you probably don’t even know what the Hypersphere is, you goddamn fucking idiot kid. I bet you don’t know the first goddamn thing about the Hypersphere. If you were paying attention, you would have gathered that it’s a big fucking 3 place, but one thing I bet you didn’t know about the Hypersphere is that it is filled with fucked up freaks. There are normal people too, but they just aren’t as interesting as the freaks. Are you a freak, kid? Some sort of fucking Hypersphere psycho? What the fuck are you even doing here? Get the fuck out of my face you fucking deviant. So there I was, chilling out in the Hypersphere. I’d spent the vast majority of my life there, in fact. It did contain everything in my observable universe, so it was pretty hard to leave, honestly. At the time, I was stressing the fuck out about a fight I had gotten in earlier. I’d been shooting some hoops when some no-good shithouses had waltzed up to me and tried to make a scene. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement.