Shoulder Dystocia Shoulder Dystocia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
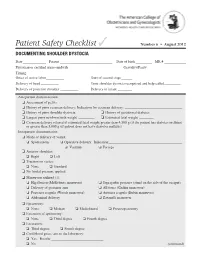
Documenting Shoulder Dystocia
Patient Safety Checklist ✓ Number 6 • August 2012 DOCUMENTING SHOULDER DYSTOCIA Date _____________ Patient _____________________________ Date of birth _________ MR # ____________ Physician or certified nurse–midwife _____________________________ Gravidity/Parity______________________ Timing: Onset of active labor __________ Start of second stage ______ Delivery of head __________ Time shoulder dystocia recognized and help called _________ Delivery of posterior shoulder __________ Delivery of infant ________ Antepartum documentation: ❏ Assessment of pelvis ❏ History of prior cesarean delivery: Indication for cesarean delivery: ________________________________ ❏ History of prior shoulder dystocia ❏ History of gestational diabetes ❏ Largest prior newborn birth weight _________ ❏ Estimated fetal weight ________ ❏ Cesarean delivery offered if estimated fetal weight greater than 4,500 g (if the patient has diabetes mellitus) or greater than 5,000 g (if patient does not have diabetes mellitus) Intrapartum documentation: ❏ Mode of delivery of vertex: ❏ Spontaneous ❏ Operative delivery: Indication: _________________________________________ ❏ Vacuum ❏ Forceps ❏ Anterior shoulder: ❏ Right ❏ Left ❏ Traction on vertex: ❏ None ❏ Standard ❏ No fundal pressure applied ❏ Maneuvers utilized (1): ❏ Hip flexion (McRoberts maneuver) ❏ Suprapubic pressure (stand on the side of the occiput) ❏ Delivery of posterior arm ❏ All fours (Gaskin maneuver) ❏ Posterior scapula (Woods maneuver) ❏ Anterior scapula (Rubin maneuver) ❏ Abdominal delivery ❏ Zavanelli maneuver -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Shoulder Dystocia Abnormal Placentation Umbilical Cord
Obstetric Emergencies Shoulder Dystocia Abnormal Placentation Umbilical Cord Prolapse Uterine Rupture TOLAC Diabetic Ketoacidosis Valerie Huwe, RNC-OB, MS, CNS & Meghan Duck RNC-OB, MS, CNS UCSF Benioff Children’s Hospital Outreach Services, Mission Bay Objectives .Highlight abnormal conditions that contribute to the severity of obstetric emergencies .Describe how nurses can implement recommended protocols, procedures, and guidelines during an OB emergency aimed to reduce patient harm .Identify safe-guards within hospital systems aimed to provide safe obstetric care .Identify triggers during childbirth that increase a women’s risk for Post Traumatic Stress Disorder and Postpartum Depression . Incorporate a multidisciplinary plan of care to optimize care for women with postpartum emergencies Obstetric Emergencies • Shoulder Dystocia • Abnormal Placentation • Umbilical Cord Prolapse • Uterine Rupture • TOLAC • Diabetic Ketoacidosis Risk-benefit analysis Balancing 2 Principles 1. Maternal ‒ Benefit should outweigh risk 2. Fetal ‒ Optimal outcome Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3 Prior vaginal births: 7.12, 8.1, 8.5 (NCB) .Late to care – EDC ~ 40-41 weeks .GDM Type A2 – somewhat uncontrolled .4’11’’ .Hx of Lupus .BMI 40 .Gained ~ 40 lbs during pregnancy Question: What complication is she a risk for? a) Placental abruption b) Thyroid Storm c) Preeclampsia with severe features d) Shoulder dystocia e) Uterine prolapse Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3 -

OBGYN-Study-Guide-1.Pdf
OBSTETRICS PREGNANCY Physiology of Pregnancy: • CO input increases 30-50% (max 20-24 weeks) (mostly due to increase in stroke volume) • SVR anD arterial bp Decreases (likely due to increase in progesterone) o decrease in systolic blood pressure of 5 to 10 mm Hg and in diastolic blood pressure of 10 to 15 mm Hg that nadirs at week 24. • Increase tiDal volume 30-40% and total lung capacity decrease by 5% due to diaphragm • IncreaseD reD blooD cell mass • GI: nausea – due to elevations in estrogen, progesterone, hCG (resolve by 14-16 weeks) • Stomach – prolonged gastric emptying times and decreased GE sphincter tone à reflux • Kidneys increase in size anD ureters dilate during pregnancy à increaseD pyelonephritis • GFR increases by 50% in early pregnancy anD is maintaineD, RAAS increases = increase alDosterone, but no increaseD soDium bc GFR is also increaseD • RBC volume increases by 20-30%, plasma volume increases by 50% à decreased crit (dilutional anemia) • Labor can cause WBC to rise over 20 million • Pregnancy = hypercoagulable state (increase in fibrinogen anD factors VII-X); clotting and bleeding times do not change • Pregnancy = hyperestrogenic state • hCG double 48 hours during early pregnancy and reach peak at 10-12 weeks, decline to reach stead stage after week 15 • placenta produces hCG which maintains corpus luteum in early pregnancy • corpus luteum produces progesterone which maintains enDometrium • increaseD prolactin during pregnancy • elevation in T3 and T4, slight Decrease in TSH early on, but overall euthyroiD state • linea nigra, perineum, anD face skin (melasma) changes • increase carpal tunnel (median nerve compression) • increased caloric need 300cal/day during pregnancy and 500 during breastfeeding • shoulD gain 20-30 lb • increaseD caloric requirements: protein, iron, folate, calcium, other vitamins anD minerals Testing: In a patient with irregular menstrual cycles or unknown date of last menstruation, the last Date of intercourse shoulD be useD as the marker for repeating a urine pregnancy test. -

Pretest Obstetrics and Gynecology
Obstetrics and Gynecology PreTestTM Self-Assessment and Review Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the prod- uct information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. Obstetrics and Gynecology PreTestTM Self-Assessment and Review Twelfth Edition Karen M. Schneider, MD Associate Professor Department of Obstetrics, Gynecology, and Reproductive Sciences University of Texas Houston Medical School Houston, Texas Stephen K. Patrick, MD Residency Program Director Obstetrics and Gynecology The Methodist Health System Dallas Dallas, Texas New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2009 by The McGraw-Hill Companies, Inc. -

Obstetrics 2002
OBSTETRICS Dr. P. Bernstein Laura Loijens and Colleen McDermott, chapter editors Tracy Chin, associate editor NORMAL OBSTETRICS . 2 ABNORMAL LABOUR . .34 Definitions Induction of Labour Diagnosis of Pregnancy Induction Methods Investigations Augmentation of Labour Maternal Physiology Abnormal Progress of Labour Umbilical Cord Prolapse PRENATAL CARE . 5 Shoulder Dystocia Preconception Counseling Breech Presentation Initial Visit Vaginal Birth After Cesarean (VBAC) Subsequent Visits Uterine Rupture Gestation-Dependent Management Amniotic Fluid Embolus Prenatal Diagnosis OPERATIVE OBSTETRICS . .39 FETAL MONITORING. 8 Indications for Operative Vaginal Delivery Antenatal Monitoring Forceps Intra-Partum Monitoring Vacuum Extraction Lacerations MULTIPLE GESTATION . .12 Episiotomy Background Cesarean Delivery Management Twin-Twin Transfusion Syndrome OBSTETRICAL ANESTHESIA . .40 Pain Pathways During Labour MEDICAL CONDITIONS IN PREGNANCY . .13 Analgesia Urinary Tract Infection (UTI) Anesthesia Iron Deficiency Anemia Folate Deficiency Anemia NORMAL PUERPERIUM . .42 Diabetes Mellitus (DM) Definition Gestational Diabetes Mellitus (GDM) Post-Delivery Examination Hypertensive Disorders of Pregnancy Breast Hyperemesis Gravidarum Uterus Isoimmunization Lochia Infections During Pregnancy Postpartum Care ANTENATAL HEMORRHAGE . .22 PUERPERAL COMPLICATIONS . .42 First and Second Trimester Bleeding Retained Placenta Therapeutic Abortions Uterine Inversion Third Trimester Bleeding Postpartum Pyrexia Placenta Previa Postpartum Hemorrhage (PPH) Abruptio Placentae -

Intractable Shoulder Dystocia: a Posterior Axilla Maneuver May Save the Day
Intractable shoulder dystocia: A posterior axilla maneuver may save the day My preferred posterior axilla maneuver is the Menticoglou maneuver. Here, a look at your options and steps to delivery. Robert L. Barbieri, MD houlder dystocia is an unpredictable 7. delivering the posterior arm obstetric emergency that challenges 8. considering the Gaskin all-four maneuver. S all obstetricians and midwives. In response to a shoulder dystocia emergency, When initial management most clinicians implement a sequence of steps are not enough IN THIS well-practiced steps that begin with early If this sequence of steps does not result in ARTICLE recognition of the problem, clear communi- successful vaginal delivery, additional op- cation of the emergency with delivery room tions include: clavicle fracture, cephalic re- staff, and a call for help to available clinicians. placement followed by cesarean delivery Menticoglou Management steps may include: (Zavanelli maneuver), symphysiotomy, or maneuver 1. instructing the mother to stop pushing and fundal pressure combined with a rotational page 18 moving the mother’s buttocks to the edge maneuver. Another simple intervention that of the bed is not discussed widely in medical textbooks Importance of 2. ensuring there is not a tight nuchal cord or taught during training is the posterior simulation 3. committing to avoiding the use of excessive axilla maneuver. page 20 force on the fetal head and neck 4. considering performing an episiotomy 5. performing the McRoberts maneuver com- Posterior axilla maneuvers bined with suprapubic pressure Varying posterior axilla maneuvers have 6. using a rotational maneuver, such as the been described by many expert obstetri- Woods maneuver or the Rubin maneuver cians, including Willughby (17th Cen- tury),1 Holman (1963),2 Schramm (1983),3 4 Dr. -

Medicalverdicts
Medical Verdicts Notable judgmeNts aNd settlemeNts gravida in septic shock; partners during her pregnancy. were signs missed? } physician’s DEFENSE Negative results of a Herpes Select Test 6 months wiTh sEVERE ABDOMINAL PAIN AND VOMITING at 14 before birth made follow-up testing weeks’ gestation, a 30-year-old woman was brought unnecessary. She must have contracted by ambulance to the hospital. After initial evalua- the disease after testing had been per- tion did not reveal a cause of her symptoms, she was formed. She had no symptoms that transferred to the antepartum unit for observation. made the viral disease diagnosable at The mother developed hypotension and a diagnosis of septic shock delivery. The child’s symptoms sug- was made. Fetal cardiac activity ceased and the woman developed intesti- gested transplacental transmission of nal ischemia. She underwent an intestinal transplant several months later. herpes; a cesarean delivery would not have changed the outcome. } paTiEnT’s cLAIM Both treating physicians and the nursing staff failed to } VERDICT A Nevada defense react to her intermittently low blood pressure, and failed to diagnose or verdict was returned. treat septic shock in a timely manner. } defenDanTs’ DEFENSE The patient was properly monitored and treated. } VERDICT A $11,500,000 Illinois verdict was returned against the hospital. home birth A defense verdict was returned for both physicians. emergency DuRing a homE birth managed by severe abdominal pain after surgery. a midwife, the baby was born after Lethal outcome of } defenDanTs’ DEFENSE Bowel perfo- the mother pushed for 2 hours and ovarian cystectomy ration is a known complication of the 47 minutes. -

Rupture of the Symphysis Pubis During Vaginal Delivery Followed
REFERENCES Present status and future role of the Zavanelli maneuver. 1. Sandberg EC. The Zavanelli maneuver: A potentially rev- Obstet Gynecol 1993;82:847–50. olutionary method for the resolution of shoulder dystocia. 5. Gherman RB, Ouzounian JG, Goodwin TM. Brachial Am J Obstet Gynecol 1985;152:479–84. plexus palsy: An in utero injury? Am J Obstet Gynecol 2. Gherman RB, Ouzounian JG, Goodwin TM. Obstetric 1999;180:1303–7. maneuvers for shoulder dystocia and associated fetal mor- 6. Sandmire HF, DeMott RK. Erb’s palsy: Concepts of causa- bidity. Am J Obstet Gynecol 1998;178:1126–30. tion. Obstet Gynecol 2000;95:940–2. 3. Sandberg EC. The Zavanelli maneuver: 12 years of recorded experience. Obstet Gynecol 1999;93:312–7. Received March 6, 2002. Received in revised form April 25, 2002. 4. O’Leary JA. Cephalic replacement for shoulder dystocia: Accepted May 13, 2002. Rupture of the Symphysis Pubis pregnancies. We present a case of a woman with a 5-cm symphyseal separation with vaginal delivery followed by During Vaginal Delivery two subsequent normal pregnancies. Followed by Two Subsequent Uneventful Pregnancies CASE A young, healthy primigravida experienced spontane- Patrick Culligan, MD, Stephanie Hill, and ous rupture of membranes followed by spontaneous Michael Heit, MD, MSPH labor at 37 weeks’ gestation. Her pregnancy had been Division of Urogynecology and Reconstructive Pelvic Surgery, Department of uneventful. Cervical dilatation progressed to 4 cm 2 Obstetrics and Gynecology, University of Louisville Health Sciences Center, Lou- hours after her membranes ruptured and she was given isville, Kentucky epidural anesthesia. She progressed through the active phase of labor without oxytocin augmentation, and was BACKGROUND: Rupture of the symphysis pubis during vag- fully dilated 6 hours after the placement of her epidural inal delivery is a rare but debilitating complication. -
Abnormalities of Labor and Delivery
Abnormalities of labour and delivery Artúr Beke MD PhD Semmelweis University Department of Obstetrics and Gynecology Department of Obstetrics and Gynecology Baross Street Abnormalities of labor and delivery • 1. Fetal malpositions and malpresentations • 2. Uterine dystocia • 3. Shoulder dystocia • 4. Premature rupture of the membranes • 5. Fetal distress • 6. Preterm delivery • 7. Twin delivery Artur Beke - Abnormalities of Labour and Delivery - 2019 1. Fetal malposition and malpresentations Artur Beke - Abnormalities of Labour and Delivery - 2019 Fetal malposition and malpresentations • A./ Abnormal presentation – Breech presentation – Transverse or oblique lie (shoulder presentation) • B./ Abnormal position – High sagittal position – Obliquity • C./ Abnormalities of flexion – Deflexion of the head • D./ Abnormalities of rotation Artur Beke - Abnormalities of Labour and Delivery - 2019 A./ ABNORMAL PRESENTATION • Cephalic presentation 96.5% • Breech presentation 3.0% • Transverse or oblique lie 0.5% Artur Beke - Abnormalities of Labour and Delivery - 2019 Breech presentation • Fetal buttocks or lower extremities present • 3% of all deliveries • At the 30th week 25% of fetuses • After 36th week no change in position Artur Beke - Abnormalities of Labour and Delivery - 2019 Types of breech presentation • Frank breech - Extended legs (Simple) (65%) • Complete breech - Flexed legs (25%) • Incomplete breech - Footling or knee presentation (10%) Artur Beke - Abnormalities of Labour and Delivery - 2019 Diagnosis of breech presentation • Leopold -

Abdominal Access for Shoulder Dystocia As a Last Resort – a Case Report Abdominaler Zugang Bei Schulterdystokie Als Ultima Ratio – Ein Fallbericht
634 GebFra Science Abdominal Access for Shoulder Dystocia as a Last Resort – a Case Report Abdominaler Zugang bei Schulterdystokie als Ultima Ratio – ein Fallbericht Authors A. Enekwe1, R. Rothmund2, B. Uhl1 Affiliations 1 Gynaecology Deparment, St-Vinzenz-Hospital Dinslaken, Dinslaken, Germany 2 University Hospital of Obstetrics and Gynaecology, Tübingen, Germany Key words Abstract Zusammenfassung l" shoulder dystocia ! ! l" abdominal rescue Shoulder dystocia is the term used to describe Die Schulterdystokie beschreibt einen Geburts- l" ʼ Erb s palsy failure to progress in labour after the head has stillstand nach Geburt des Kopfes aufgrund unzu- Schlüsselwörter been delivered due to insufficient rotation of the reichender Schulterdrehung. Das Ereignis trifft l" Schulterdystokie shoulders. It is unpredictable and cannot be pre- die geburtshilflich tätige Person in der Regel völ- l" abdominaler vented by the midwife or the obstetrician. We lig unerwartet. Es wird hier über einen Fall einer Rettungsversuch report here on a severe case of shoulder dystocia, schweren Schulterdystokie berichtet, bei dem die l" Armplexusparese where delivery of the shoulder was finally Schulterlösung durch direkten Druck auf die vor- achieved through direct pressure on the anterior dere Schulter nach Laparotomie und Uterotomie shoulder after laparotomy and uterotomy with bei gleichzeitigem Woods-Screw-Manöver von concurrent vaginal Woods screw manoeuvre and vaginal mit anschließender vaginaler Entbindung was followed by vaginal delivery. The patient pre- gelang. Die Patientin wies eine Adipositas und die sented risk factors like maternal obesity and ad- Gabe von wehenfördernden Mitteln als Risikofak- ministration of labour-inducing drugs. After dif- toren auf. Nach erfolgloser Ausführung des McRo- ferent manoeuvres like McRoberts manoeuvre berts-Manövers und diverser Manöver zur inne- and several manoeuvres for internal rotation ren Rotation wurde eine Notlaparotomie durch- were carried out unsuccessfully, an emergency geführt. -
Predictive Factors for the Success Of
Lok et al. BMC Pregnancy and Childbirth (2016) 16:334 DOI 10.1186/s12884-016-1125-3 RESEARCH ARTICLE Open Access Predictive factors for the success of McRoberts’ manoeuvre and suprapubic pressure in relieving shoulder dystocia: a cross-sectional study Zara Lin Zau Lok, Yvonne Kwun Yue Cheng and Tak Yeung Leung* Abstract Background: McRoberts’ and suprapubic pressure are often recommended as the initial choices of manoeuvres to manage shoulder dystocia, as they are believed to be less invasive compared to other manoeuvres. However, their success rates range from 23 to 40 %. This study aims to investigate the predictive factors for the success of McRoberts’ manoeuvre with or without suprapubic pressure (M+/−S). Methods: All cases of shoulder dystocia in a tertiary hospital in South East Asia were recruited from 1995 to 2009. Subjects were analysed according to either ‘success’ or ‘failure’ of M+/−S. Maternal and fetal antenatal and intrapartum factors were compared by univariate and multivariate analysis. Results: Among 198 cases of shoulder dystocia, M+/−S as the primary manoeuvre was successful in 25.8 %. The other 74.2 % needed either rotational or posterior arm manoeuvres or combination of manoeuvres. Instrumental delivery was the single most significant factor associated with an increased risk of failed M+/−S on logistic regression (p < 0.001, OR 4.88, 95 % CI 2.05–11.60). The success rate of M+/−S was only 15.0 % if shoulder dystocia occurred after instrumental delivery but was 47.7 % after spontaneous vaginal delivery. Conclusions: When shoulder dystocia occurs after instrumental vaginal delivery, the chance of failure of M+/−Sis 85 %, which is 4.7 times higher than that after spontaneous vaginal delivery.