Attenuation of Nrf2/Keap1/ARE in Alzheimer's Disease By
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intestinal Anti-Inflammatory Activity of Terpenes in Experimental Models
molecules Review Intestinal Anti-Inflammatory Activity of Terpenes in Experimental Models (2010–2020): A Review Maria Elaine Araruna 1, Catarina Serafim 1, Edvaldo Alves Júnior 1, Clelia Hiruma-Lima 2, Margareth Diniz 1,3 and Leônia Batista 1,3,* 1 Postgraduate Program in Natural Products and Bioactive Synthetic, Health Sciences Center, Federal University of Paraiba, João Pessoa 58051-900, PB, Brazil; [email protected] (M.E.A.); [email protected] (C.S.); [email protected] (E.A.J.); [email protected] (M.D.) 2 Department of Structural and Functional Biology (Physiology), Institute of Biosciences, São Paulo State University, Botucatu 18618-970, SP, Brazil; [email protected] 3 Department of Pharmacy, Health Sciences Center, Federal University of Paraíba, João Pessoa 58051-900, PB, Brazil * Correspondence: [email protected]; Tel.: +55-83-32167003; Fax: +55-83-32167502 Academic Editors: Maurizio Battino, Jesus Simal-Gandara and Esra Capanoglu Received: 8 September 2020; Accepted: 28 September 2020; Published: 20 November 2020 Abstract: Inflammatory bowel diseases (IBDs) refer to a group of disorders characterized by inflammation in the mucosa of the gastrointestinal tract, which mainly comprises Crohn’s disease (CD) and ulcerative colitis (UC). IBDs are characterized by inflammation of the intestinal mucosa, are highly debilitating, and are without a definitive cure. Their pathogenesis has not yet been fully elucidated; however, it is assumed that genetic, immunological, and environmental factors are involved. People affected by IBDs have relapses, and therapeutic regimens are not always able to keep symptoms in remission over the long term. Natural products emerge as an alternative for the development of new drugs; bioactive compounds are promising in the treatment of several disorders, among them those that affect the gastrointestinal tract, due to their wide structural diversity and biological activities. -
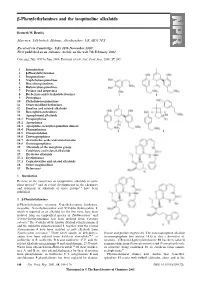
Β-Phenylethylamines and the Isoquinoline Alkaloids
-Phenylethylamines and the isoquinoline alkaloids Kenneth W. Bentley Marrview, Tillybirloch, Midmar, Aberdeenshire, UK AB51 7PS Received (in Cambridge, UK) 28th November 2000 First published as an Advance Article on the web 7th February 2001 Covering: July 1999 to June 2000. Previous review: Nat. Prod. Rep., 2000, 17, 247. 1 Introduction 2 -Phenylethylamines 3 Isoquinolines 4 Naphthylisoquinolines 5 Benzylisoquinolines 6 Bisbenzylisoquinolines 7 Pavines and isopavines 8 Berberines and tetrahydoberberines 9 Protopines 10 Phthalide-isoquinolines 11 Other modified berberines 12 Emetine and related alkaloids 13 Benzophenanthridines 14 Aporphinoid alkaloids 14.1 Proaporphines 14.2 Aporphines 14.3 Aporphine–benzylisoquinoline dimers 14.4 Phenanthrenes 14.5 Oxoaporphines 14.6 Dioxoaporphines 14.7 Aristolochic acids and aristolactams 14.8 Oxoisoaporphines 15 Alkaloids of the morphine group 16 Colchicine and related alkaloids 17 Erythrina alkaloids 17.1 Erythrinanes 17.2 Cephalotaxine and related alkaloids 18 Other isoquinolines 19 References 1 Introduction Reviews of the occurrence of isoquinoline alkaloids in some plant species 1,2 and of recent developments in the chemistry and synthesis of alkaloids of these groups 3–6 have been published. 2 -Phenylethylamines β-Phenylethylamine, tyramine, N-methyltyramine, hordenine, mescaline, N-methylmescaline and N,N-dimethylmescaline 1, which is reported as an alkaloid for the first time, have been isolated from an unspecified species of Turbinocarpus 7 and N-trans-feruloyltyramine has been isolated from Cananga odorata.8 The N-oxides of the known alkaloid culantraramine 2 and the unknown culantraraminol 3, together with the related avicennamine 4 have been isolated as new alkaloids from Zanthoxylum avicennae.9 Three novel amides of dehydrotyr- leucine and proline respectively. -

Subject Index
52_1107_1136_SI 16.11.2005 9:35 Uhr Seite 1107 Subject Index A – tape 264, 368, 940 α-adjustment 154 AAS, see atomic absorption spectrophotometry adrenocorticotrophic hormone (ACTH) 21 abietic acid 909, 943 adverse drug reaction 401 abrasion 174, 283 aeroallergen 391 absorption through appendage 169 – atopic eczema 391 α-acaridial 329 – avoidance 391 accident 889 aerospace 726 acebutolol hydrochloride 909 African aceclofenac 909 –ebony783 acetaldehyde 943 – mahagony 783 acetone 118, 666 – red padauk wood 783 acetylacetone 697 Agave acetylsalicylic acid 84, 909 – americana 354 Achillea millefolium (yarrow extract) 909 – tequilana 225 aciclovir 909 age 279 acid 110 agent orange 806 – black 48 (CI 65005) 909 AGEP 404 – dye 689 Agfa TSS 355 – halogenated 259 aggravation 204 –hydrochloric261 agricultural worker 272 –nitric261 agriculture 725 –red AICD, see activation-induced cell death – – 14 (azorubine) 909 airborne – – 118 (CI 26410) 909 – allergic contact dermatitis 218, 228, 315, 467, 477, 484, 598, ––359909 627, 654, 788 – violet 17 (CI 42650) 909 – contact urticaria 753, 758 – yellow – irritant contact dermatitis 625 – – 36 (CI 13065, metanil yellow) 909 aircraft manufacture 560 – – 61 (CI 18968) 909 airway symptom 520 acitretin 341 alachlor 953 acneiform alantolactone 55, 789, 909, 954 – folliculitis 229 alclometasone-17,21-dipropionate 909 –lesion265 alclometasone-17-propionate 58 acrodermatitis enteropathica 241 alcohol, see also ethyl 909 acrovesicular dermatitis 401 aldehyde 110, 607, 886 acrylamide 592, 944 algicide 562 acrylate -

Anti-Inflammatory Activity of Compounds from Kaempferia Marginata Rhizomes
Songklanakarin J. Sci. Technol. 39 (1), 91-99, Jan. - Feb. 2017 http://www.sjst.psu.ac.th Original Article Anti-inflammatory activity of compounds from Kaempferia marginata rhizomes Kanidta Kaewkroek1, Chatchai Wattanapiromsakul1, 2, Hisashi Matsuda3, Seikou Nakamura3, and Supinya Tewtrakul1, 2* 1 Department of Pharmacognosy and Pharmaceutical Botany, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Songkhla, 90112 Thailand 2 Excellent Research Laboratory, Phytomedicine and Phamaceutical Biotechnology Excellence Center, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Songkhla, 90112 Thailand 3 Kyoto Pharmaceutical University, Misasagi, Yamashina-ku, Kyoto, 607-8412 Japan Received: 12 January 2016; Revised: 12 April 2016; Accepted: 19 April 2016 Abstract Two new pimarane diterpenes were obtained from Kaempferia marginata rhizomes, which are 1-acetoxysandara- copimaradien-2-one (1) and 1-acetoxysandaracopimaradiene (4), along with seven known compounds from the hexane and chloroform fractions including two pimarane-type diterpenes [marginatol (5), sandaracopimaradiene (8)], one kavalactone [desmethoxyyangonin (3)], three steroids [sitosterol--D-glucoside (2), the mixture of stigmasterol and -sitosterol (6 + 7)] and one diarylheptanoid [bisdemethoxycurcumin (9)]. Compounds 3 and 9 exhibited potent effect against NO production with IC50 of 10.1 and 6.8 µM, respectively. Compound 3 inhibited iNOS mRNA expression in a dose-dependent manner, while 9 suppressed both of iNOS and COX-2 genes. Moreover, compounds 2, 3, 6 + 7 and 9 were isolated for the first time from K. marginata. These results revealed that diterpenes, diarylheptanoid and kavalactone are components of K. marginata that afford anti-inflammatory effect through a mechanism involving a decrease in inflammatory mediators. Keywords: Kaempferia marginata, diterpenes, diarylheptanoid, kavalactone, anti-inflammatory activity 1. -

Herbal Insomnia Medications That Target Gabaergic Systems: a Review of the Psychopharmacological Evidence
Send Orders for Reprints to [email protected] Current Neuropharmacology, 2014, 12, 000-000 1 Herbal Insomnia Medications that Target GABAergic Systems: A Review of the Psychopharmacological Evidence Yuan Shia, Jing-Wen Donga, Jiang-He Zhaob, Li-Na Tanga and Jian-Jun Zhanga,* aState Key Laboratory of Bioactive Substance and Function of Natural Medicines, Institute of Materia Medica, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, P.R. China; bDepartment of Pharmacology, School of Marine, Shandong University, Weihai, P.R. China Abstract: Insomnia is a common sleep disorder which is prevalent in women and the elderly. Current insomnia drugs mainly target the -aminobutyric acid (GABA) receptor, melatonin receptor, histamine receptor, orexin, and serotonin receptor. GABAA receptor modulators are ordinarily used to manage insomnia, but they are known to affect sleep maintenance, including residual effects, tolerance, and dependence. In an effort to discover new drugs that relieve insomnia symptoms while avoiding side effects, numerous studies focusing on the neurotransmitter GABA and herbal medicines have been conducted. Traditional herbal medicines, such as Piper methysticum and the seed of Zizyphus jujuba Mill var. spinosa, have been widely reported to improve sleep and other mental disorders. These herbal medicines have been applied for many years in folk medicine, and extracts of these medicines have been used to study their pharmacological actions and mechanisms. Although effective and relatively safe, natural plant products have some side effects, such as hepatotoxicity and skin reactions effects of Piper methysticum. In addition, there are insufficient evidences to certify the safety of most traditional herbal medicine. In this review, we provide an overview of the current state of knowledge regarding a variety of natural plant products that are commonly used to treat insomnia to facilitate future studies. -

Premenstrual Syndrome: a Natural Approach to Management
CNI506 8/99 Vol. 5, No. 6 APPLIED NUTRITIONAL SCIENCE REPORTS Copyright © 1997 Advanced Nutrition Publications, Inc. rev. 1999 Premenstrual Syndrome: A Natural Approach to Management BY JOSEPH L. MAYO, MD, FACOG ABSTRACT: Premenstrual syndrome (PMS) is a disorder that imbalances, nutritional insufficiencies, and psychologic factors. occurs during the luteal phase of the menstrual cycle, producing A nutritional approach to PMS that takes into account the complex a diverse number of physical and emotional changes. The most interactions of all bodily systems that influence hormonal balance common symptoms of PMS include bloating, backache, breast and neuroendocrine function, with an emphasis on the liver, is tenderness, food cravings, fatigue, irritability, and depression. recommended. The nutritional factors that have been studied The timing of the appearance and disappearance of symptoms, include vitamin B6, magnesium, zinc, choline, vitamin E, and rather than the presence of specific symptoms, is of more essential fatty acids, in addition to weight management and importance in the diagnosis of PMS. The direct cause of PMS is stress reduction. Herbal therapies have also proven beneficial in unknown, although there are numerous theories relating to hormonal the management of PMS. PREMENSTRUAL SYNDROME symptoms such as bloating, breast tenderness, and headache (Table 1).3-5 These diverse symptoms may range from mild Cyclic symptoms in women of reproductive age have been to incapacitating. In some women a single symptom, such recognized for thousands of years. First appearing in the medical as depression, may predominate, whereas others may have literature in 1931 and originally termed “premenstrual tension,” several symptoms.1 this condition has been renamed “premenstrual syndrome” (PMS) in an effort to take into account the different clinical Table. -

(12) Patent Application Publication (10) Pub. No.: US 2010/0311593 A1 Fischer Et Al
US 20100311593A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0311593 A1 Fischer et al. (43) Pub. Date: Dec. 9, 2010 (54) HALOALKYLMETHYLENEOXYPHENYL- AOIPI3/00 (2006.01) SUBSTITUTED KETOENOLS C07D 207/00 (2006.01) C07D 305/12 (2006.01) (75) Inventors: Reiner Fischer, Monheim (DE): CD7C 49/00 (2006.01) Thomas Bretschneider, Lohmar C07D 23/00 (2006.01) (DE); Stefan Lehr, Liederbach C07C 229/00 (2006.01) (DE); Eva-Maria Franken, Lyon C07C 69/76 (2006.01) (FR): Olga Malsam, Rosrath (DE); CD7C 24I/00 (2006.01) Arnd Voerste, Koln (DE); Ulrich CD7C 63/04 (2006.01) Görgens, Ratingen (DE); Jan (52) U.S. Cl. ......... 504/219;564/170; 514/622:504/336; Dittgen, Frankfurt (DE); Dieter Feucht, Eschborn (DE); Isolde 504/236; 514/248; 544/235; 540/545; 514/211.08; Hauser-Hahn, Leverkusen (DE); 548/544; 549/319; 568/379: 548/366.4; 560/37; Christopher Hugh Rosinger, 560/76; 560/105:564/149; 562/493 Hofheim (DE); Alfred Angermann, Kriftel (DE) (57) ABSTRACT The invention relates to novel compounds of the formula (I), Correspondence Address: STERNE, KESSLER, GOLDSTEIN & FOX P.L. L.C. (I) 1100 NEW YORKAVENUE, N.W. WASHINGTON, DC 20005 (US) (73) Assignee: Bayer Cropscience AG, Monheim (DE) (21) Appl. No.: 12/639,536 (22) Filed: Mar. 11, 2010 in which W, X, Y, Z and CKE are each as defined above, to several methods and intermediates for preparation thereof (30) Foreign Application Priority Data and to the use thereofas pesticides and/or herbicides. The invention also relates to selective herbicidal composi Mar. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

Redox Signaling and Alzheimer's Disease
Chen et al. Biomarker Research (2020) 8:42 https://doi.org/10.1186/s40364-020-00218-z REVIEW Open Access Redox signaling and Alzheimer’s disease: from pathomechanism insights to biomarker discovery and therapy strategy Yuan-Yuan Chen1†, Min-Chang Wang2†, Yan-Ni Wang1, He-He Hu1, Qing-Quan Liu3*, Hai-Jing Liu4* and Ying-Yong Zhao1* Abstract Aging and average life expectancy have been increasing at a rapid rate, while there is an exponential risk to suffer from brain-related frailties and neurodegenerative diseases as the population ages. Alzheimer’s disease (AD) is the most common neurodegenerative disease worldwide with a projected expectation to blossom into the major challenge in elders and the cases are forecasted to increase about 3-fold in the next 40 years. Considering the etiological factors of AD are too complex to be completely understood, there is almost no effective cure to date, suggesting deeper pathomechanism insights are urgently needed. Metabolites are able to reflect the dynamic processes that are in progress or have happened, and metabolomic may therefore provide a more cost-effective and productive route to disease intervention, especially in the arena for pathomechanism exploration and new biomarker identification. In this review, we primarily focused on how redox signaling was involved in AD-related pathologies and the association between redox signaling and altered metabolic pathways. Moreover, we also expatiated the main redox signaling-associated mechanisms and their cross-talk that may be amenable to mechanism-based therapies. Five natural products with promising efficacy on AD inhibition and the benefit of AD intervention on its complications were highlighted as well. -
Kava - the Unfolding Story: Report on a Work-In-Progress
Article Kava - the unfolding story: Report on a work-in-progress. Denham, Alison, McIntyre, Michael and Whitehouse, Jule Available at http://clok.uclan.ac.uk/9455/ Denham, Alison, McIntyre, Michael and Whitehouse, Jule Kava - the unfolding story: Report on a work-in-progress. Journal of Alternative and Complementary Medicine, 8 (3). pp. 237-263. It is advisable to refer to the publisher’s version if you intend to cite from the work. For more information about UCLan’s research in this area go to http://www.uclan.ac.uk/researchgroups/ and search for <name of research Group>. For information about Research generally at UCLan please go to http://www.uclan.ac.uk/research/ All outputs in CLoK are protected by Intellectual Property Rights law, including Copyright law. Copyright, IPR and Moral Rights for the works on this site are retained by the individual authors and/or other copyright owners. Terms and conditions for use of this material are defined in the policies page. CLoK Central Lancashire online Knowledge www.clok.uclan.ac.uk THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE Volume 8, Number 3, 2002, pp. 237–263 © Mary Ann Liebert, Inc. SPECIAL REPORT Kava—the Unfolding Story: Report on a Work-in-Progress ALISON DENHAM, B.A. (Soc.), M.N.I.M.H., 1 MICHAEL McINTYRE, M.A., F.N.I.M.H., F.R.C.H.M., M.B.Ac.C., 2 and JULIE WHITEHOUSE, Ph.D., M.N.I.M.H. 3 ABSTRACT This paper, originated as a submission (now updated) to the U.K. Medicines Control Agency and Committee of Safety of Medicines (CSM) on January 11, 2002, in response to a report circu- lated by the German Federal Institute for Drugs and Medical Products (German initials are BfArM), a compilation of which is summarized in Appendix 2. -

Antiparasitic Effects of Medicinal Plants (Part 1)- a Review
IOSR Journal Of Pharmacy www.iosrphr.org (e)-ISSN: 2250-3013, (p)-ISSN: 2319-4219 Volume 6, Issue 10 Version. 3 (October 2016), PP. 51-66 Antiparasitic effects of medicinal plants (part 1)- A review Prof Dr Ali Esmail Al-Snafi Department of Pharmacology, College of Medicine, Thi qar University, Nasiriyah, Iraq . Cell: +9647801397994. Email: [email protected] Abstract: Many previous researches showed that many plants exerted antiparasitic, antiprotozoal, molluscicidal and insecticidal. These plants included: Achillea santolina, Ailanthus altissima, Allium cepa, Allium sativum, Ammi majus, Anagyris foetida, Antirrhinum majus, Apium graveolens, Arachis hypogaea, Artemisia campestris, Arundo donax, Asclepias curassavica, Ballota nigra, Bauhinia variegate, Betula alba, Bidens tripartite, Brassica nigra, Bryophyllum calycinum, Caccinia crassifolia, Caesalpinia crista,Calendula officinalis, Calotropis procera, Canna indica, Capparis spinosa, Carum carvi, Cassia occidentalis, Celosia cristata, Chenopodium album, Chorchorus capsularis, Chrysanthemum cinerariaefolium, Cichorium intybus, Citrullus colocynthis, Citrus limetta, Citrus medica, Citrus sinensis, Citrus limonum, Citrus aurantifolia, Citrus reticulate, Citrus vitis, Clerodendron inerme, Clitoria ternatea, Corchorus capsularis, Cordia myxa, Coriandrum sativum, Coronilla scorpioides, Coronilla varia, Crocus sativus, Cupressus sempervirens, Cymbopogon schoenanthus, Cyminum cuminum, Cynodon dactylon, Dalbergia sissoo, Datura metel, Datura stramonium, Dianthus caryophyllum, Digitalis purpurea, -

Healthy Aging: Antioxidants, Adaptogens & Cognition
Healthy Aging: Antioxidants, Adaptogens & Cognition Karen Butler Michael Altman, CN, RH (AHG) Kieron Edwards, Ph.D. Senior Editor Herbalist Nutritionist Chief Scientific Officer Informa Markets Anthocyanins International LLC Sibelius Natural Products (SeattleCancerCareAlternatives.com) David Heber, M.D., Ph.D., FACP, FASN Katie Stage, N.D., RH (AHG) Professor Emeritus and Founding Director, Therapeutics Division Director UCLA Center for Associate Professor, Southwest Human Nutrition College of Naturopathic Medicine (SCNM) Booth #5310 Towards healthy aging Kieron Edwards PhD MBA www.sibeliusnaturalproducts.com OCTOBER 2019 1 Talk outline Booth #5310 . The trends and challenges of aging . What occurs during aging? . Theories, effects, and pathways of aging . Supporting healthy aging 2 Aging: The monster at the end of the Booth #5310 book 3 The trends and challenges of aging Booth #5310 4 What is aging? Booth #5310 . Ageing results from the impact of the accumulation of a wide variety of molecular and cellular damage over time. This leads to a gradual decrease in physical and mental capacity, a growing risk of disease, and ultimately, death. But these changes are neither linear nor consistent, and they are only loosely associated with a person’s age in years (WHO) 5 Age-related changes to health Booth #5310 . Physical aging . Sensory loss, body composition changes, osteoarthritis . Cognitive aging . Immune aging . Immunosenecence, inflammation . Cardiovascular health . CVD is still the leading cause of death in older adults . Metabolic health . Cancer . Second leading cause of death in older adults 6 Living longer and better? Booth #5310 . Human lifespan is increasing . Almost 2 years increase per decade . Age is a major risk-factor in many human diseases and conditions .