Complete Hormones Sample Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Deficiency of 21 -Hydroxylation in Patients with Congenital Adrenal Hyperplasia 0
Arch Dis Child: first published as 10.1136/adc.43.230.410 on 1 August 1968. Downloaded from Arch. Dis. Childh., 1968, 43, 410. Evaluation of Deficiency of 21 -hydroxylation in Patients with Congenital Adrenal Hyperplasia 0. M. GALAL, B. T. RUDD, and N. M. DRAYER From the Institute of Child Health, University of Birmingham Congenital adrenal hyperplasia can manifest therapy in these 13 children started within the first 3 itself in a variety of clinical and biochemical weeks of life. abnormalities (Bongiovanni and Root, 1963). The In addition to the 18 patients with congenital adrenal salt-losing tendency in some of these patients can hyperplasia, 3 children with shortness of stature and 3 with early signs of puberty were given ACTH to be due to the absence of specific enzymes: dehydro- investigate their adrenal function. None of these genases or hydroxylases (Bongiovanni and Root, patients had received steroids and all had normal free 1963; Ulick et al., 1964; Visser and Cost, 1964). cortisol and 17-hydroxycorticosteroid urinary excretion In addition to the impaired production of certain rates. The age and sex of the patients in the 3 groups steroids, antagonism by steroids or other compounds and details of the steroid therapy are listed in Table I. could, theoretically, account for the salt-losing tendency (Neher, Meystre, and Wettstein, 1959; ACTH test. Twenty-four hour urine collections Jacobs et al., 1961). were obtained before and during ACTH stimulation. The purpose ofthis study was to discover whether, ACTH gel (Organon) was given intramuscularly at a copyright. despite the continuation of steroid therapy, stimula- dose of 20 I.U. -
Endocrinology Test List Endocrinology Test List
For Endocrinologists Endocrinology Test List Endocrinology Test List Extensive Capabilities Managing patients with endocrine disorders is complex. Having access to the right test for the right patient is key. With a legacy of expertise in endocrine laboratory diagnostics, Quest Diagnostics offers an extensive menu of laboratory tests across the spectrum of endocrine disorders. This test list highlights the extensive menu of laboratory diagnostic tests we offer, including highly specialized tests and those performed using highly specific and sensitive mass spectrometry detection. It is conveniently organized by glandular function or common endocrine disorder, making it easy for you to identify the tests you need to care for the patients you treat. Comprehensive Care Quest Diagnostics Nichols Institute has been pioneering state-of-the-art endocrine testing for over four decades. Our commitment to innovative diagnostics and our dedication to quality and service means we deliver solutions that enable you to make informed clinical decisions for comprehensive patient management. We strive to remain at the forefront of innovation in endocrine testing so you can deliver the highest level of patient care. Abbreviations and Footnotes NDM, neonatal diabetes mellitus; MODY, maturity-onset diabetes of the young; CH, congenital hyperinsulinism; MSUD, maple syrup urine disease; IHH, idiopathic hypogonadotropic hypogonadism; BBS, Bardet-Biedl syndrome; OI, osteogenesis imperfecta; PKD, polycystic kidney disease; OPPG, osteoporosis-pseudoglioma syndrome; CPHD, combined pituitary hormone deficiency; GHD, growth hormone deficiency. The tests highlighted in green are performed using highly specific and sensitive mass spectrometry detection. Panels that include a test(s) performed using mass spectrometry are highlighted in yellow. For tests highlighted in blue, refer to the Athena Diagnostics website (athenadiagnostics.com/content/test-catalog) for test information. -

Comprehensive Urinary Hormone Assessments
ENDOCRINOLOGY Complete Hormones – Analytes Comprehensive Urinary Hormone Assessments Urinary Pregesterones Urinary Glucocorticoids Urinary Androgens Urinary Estrogens Pregnanediol Cortisol, Free Testosterone Estrone Pregnanetriol Total 17-Hydroxy-corticosteroids Dehydroepiandrosterone (DHEA) Estradiol allo-Tetrahydrocortisol, a-THF Total 17-Ketosteroids Estriol Tetrahydrodeoxycortisol Androsterone 2-Hydroxyestrone Tetrahydrocortisol, THF Etiocholanolone 2-Methoxyestrone Tetrahydrocortisone, THE 11-Keto-androsterone 4-Hydroxyestrone 17-Hydroxysteriods, Total 11-Keto-etiocholanolone 4-Methoxyestrone Pregnanetriol 11-Hydroxy-androsterone 16α-Hydroxyestrone 11-Hydroxy-etiocholanolone 2-Hydroxy-estrone:16α-Hydroxyestrone ratio 2-Methoxyestrone:2-Hydroxyestrone ratio CLINICIAN INFORMATION 4-Methoxyestrone:4-Hydroxyestrone ratio ADVANCING THE CLINICAL UTILITY OF URINARY HORMONE ASSESSMENT Specimen Requirements Complete Hormones™ is Genova’s most comprehensive • 120 ml aliquot, refrigerated until shipped, urinary hormone profile, and is designed to assist with the from either First Morning Urine or 24-Hour clinical management of hormone-related symptoms. This profile Collection Why Use Complete Hormones? assesses parent hormones and their metabolites as well as key metabolic pathways, and provides insight into the contribution Hormone testing is an effective tool for assessing Related Profiles: that sex hormones may have in patients presenting with and managing patients with hormone- related symptoms. This profile supports: • Male Hormonal Health™ -

Endocrinology Assessments
2013 Edition Endocrinology Assessments PRODUCT LINE GUIDE THE GENOVA DIAGNOSTICS Advantage Our comprehensive line of assessments for personalized treatment & prevention of chronic disease: • Provides Fully Licensed and Certified Laboratory Services • Saves Practitioner Time with Easy-to-Read Test Results • Features Rapid Turnaround • Includes Support for Practitioner and Patient • Offers Patient and Practitioner Billing Options Visit us anytime on the web at www.GDX.net or call 800-522-4762 Monday through Friday, 8:30 am to 6:30 pm (Eastern Time) to order tests or more information about our services. ACCREDITATION Genova Diagnostics is fully licensed federally under Clinical Laboratory Improvement Amendments (CLIA) and certified by Medicare (all states), and by New York State. TABLE OF CONTENTS Endocrinology Product Line Guide for Genova Diagnostics 2-5 Steroidogenic Pathways Chart __________________________________18 Essence Hormone Tests ____________ First Morning Void vs. 24-Hour Collection __________________________19 Specimen Selection Salivary Assessments A Guide to Choosing Sample Types ________________________________2 Menopause Plus ______________________________________________20 Complete Testing Line Rhythm ____________________________________________________22 Individual Components Breakdown Chart __________________________4 Male Hormones Plus __________________________________________24 One Day Hormone Check ______________________________________26 Therapeutic Ranges for Menopause Profile ________________________28 Profiles -

Circadian Patterns of Plasma Cortisol, 17-Hydroxyprogesterone, and Testosterone in Congenital Adrenal Hyperplasia
Arch Dis Child: first published as 10.1136/adc.56.3.208 on 1 March 1981. Downloaded from Archives of Disease in Childhood, 1981, 56, 208-213 Circadian patterns of plasma cortisol, 17-hydroxyprogesterone, and testosterone in congenital adrenal hyperplasia H FRISCH, K PARTH, EDITH SCHOBER, AND W SWOBODA Department ofPaediatrics, University of Vienna School ofMedicine, andLudwig Boltzman Institutfuir klinische Endokrinologie und Nuklearmedizin, Vienna, Austria SUMMARY In 11 children aged between 2 and 17 years with (nonsalt-losing) congenital adrenal hyperplasia (21-hydroxylase deficiency) blood was drawn at 90-minute intervals during a 24-hour period and levels of 17-hydroxyprogesterone, testosterone, and cortisol were measured. Levels of 1 7-ketosteroids and pregnanetriol were measured too in 24-hour urine samples. These measurements were taken under different regimens of treatment and after interruption of treatment. Cortisol levels rose and fell rapidly after administered corticosteroid, and reached unphysiologically high levels. Testosterone levels showed pronounced variations but stayed in the normal range for most of the time even in untreated patients; thus testosterone provides a poor control parameter. Levels of 1 7-hydroxyprogesterone showed extreme fluctuations and very high peak levels in untreated patients; standard treatment with two or three daily doses of corticosteroids did not prevent a pronounced rise in its level after midnight. After the first morning dose of hydrocortisone a very steep fall was observed. The 24-hour pregnanetriol excretion correlated well with the corresponding total integrated copyright. 1 7-hydroxyprogesterone area. It is concluded that single 1 7-hydroxyprogesterone values are unlikely to give adequate information about the quality oftreatment. -
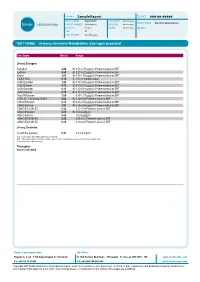
Sample Report
PATIENT: Sample Report TEST REF: ###-##-##### TEST NUMBER: ########## COLLECTED: dd/mm/yyyy PRACTITIONER: Nordic Laboratories PATIENT NUMBER: ########## RECEIVED: dd/mm/yyyy GENDER: Female TESTED: dd/mm/yyyy ADDRESS: AGE: 28 DATE OF BIRTH: dd-mm-yyyy TEST NAME: Urinary Hormone Metabolites Estrogen Essential Test Name Result Range Urinary Estrogens Estradiol 2.52 H 0.78-1.79 µg/g Cr Premeno-luteal or ERT Estrone 8.58 H 2.27-5.22 µg/g Cr Premeno-luteal or ERT Estriol 2.05 H 0.78-1.98 µg/g Cr Premeno-luteal or ERT E3/(E1+E2) 0.18 L >0.3 (> median value) 2-OH Estradiol 1.23 H 0.17-0.70 µg/g Cr Premeno-luteal or ERT 2-OH Estrone 4.79 H 0.70-2.54 µg/g Cr Premeno-luteal or ERT 4-OH Estradiol 0.35 H 0.10-0.18 µg/g Cr Premeno-luteal or ERT 4-OH Estrone 0.75 H 0.17-0.47 µg/g Cr Premeno-luteal or ERT 16α-OH Estrone 1.00 0.35-1.07 µg/g Cr Premeno-luteal or ERT 2-OH (E1 + E2)/16-α-OH E1 6.02 H 1.29-5.49 Premeno-luteal or ERT 2-MeO Estradiol 0.18 H 0.03-0.08 µg/g Cr Premeno-luteal or ERT 2-MeO Estrone 1.51 H 0.26-0.68 µg/g Cr Premeno-luteal or ERT 2-MeO E1/2-OH E1 0.32 0.21-0.38 Premeno-luteal or ERT 4-MeO Estradiol 0.05 H <0.04 µg/g Cr 4-MeO Estrone 0.04 <0.04 µg/g Cr 4-MeO E1/4-OH E1 0.05 0.05-0.13 Premeno-luteal or ERT 4-MeO E2/4-OH E2 0.14 0.10-0.29 Premeno-luteal or ERT Urinary Creatinine Creatinine (pooled) 0.32 0.3-2.0 mg/mL <dL = Less than the detectable limit of the lab. -

Non-Classic Disorder of Adrenal Steroidogenesis and Clinical Dilemmas in 21-Hydroxylase Deficiency Combined with Backdoor Androg
International Journal of Molecular Sciences Review Non-Classic Disorder of Adrenal Steroidogenesis and Clinical Dilemmas in 21-Hydroxylase Deficiency Combined with Backdoor Androgen Pathway. Mini-Review and Case Report Marta Sumi ´nska 1,* , Klaudia Bogusz-Górna 1, Dominika Wegner 1 and Marta Fichna 2 1 Department of Pediatric Diabetes and Obesity, Poznan University of Medical Sciences, 60-527 Poznan, Poland; [email protected] (K.B.-G.); [email protected] (D.W.) 2 Department of Endocrinology, Metabolism and Internal Medicine, Poznan University of Medical Sciences, 60-653 Poznan, Poland; mfi[email protected] * Correspondence: [email protected] Received: 3 June 2020; Accepted: 28 June 2020; Published: 29 June 2020 Abstract: Congenital adrenal hyperplasia (CAH) is the most common cause of primary adrenal insufficiency in children and adolescents. It comprises several clinical entities associated with mutations in genes, encoding enzymes involved in cortisol biosynthesis. The mutations lead to considerable (non-classic form) to almost complete (classic form) inhibition of enzymatic activity, reflected by different phenotypes and relevant biochemical alterations. Up to 95% cases of CAH are due to mutations in CYP21A2 gene and subsequent 21α-hydroxylase deficiency, characterized by impaired cortisol synthesis and adrenal androgen excess. In the past two decades an alternative (“backdoor”) pathway of androgens’ synthesis in which 5α-androstanediol, a precursor of the 5α-dihydrotestosterone, is produced from 17α-hydroxyprogesterone, with intermediate products 3α,5α-17OHP and androsterone, in the sequence and with roundabout of testosterone as an intermediate, was reported in some studies. This pathway is not always considered in the clinical assessment of patients with hyperandrogenism. -

Discover Essential Insights Oids Omatase TIC S ,20 Desmolase Ro with Specialized Hormone Testing
TM with specialized hormone testing Discover Essential Insights the GDX-7-144 Cholesterol Steroidogenic Pathways © 2018 Genova Diagnostics Pregnenolone 17-OH-Pregnenolone DHEAAndrostenediol Essence_trifold_030718 Pregnanediol Pregnanetriol Progesterone 17-OH-Progesterone Androstenedione Testosterone Etiocholanolone 11-Deoxycortisol DHT Corticosterone THS 11β-OH-Androstenedione Androsterone Androstanediol Mineralocorticoids Cortisol Cortisone 11-OH-Androsterone Estrone (E1) Estradiol (E2) Aldosterone* a-THFTHF THE 11-OH-Etiocholanolone Adrenosterone 2-OH (E1+E2) 2-MeO (E1+E2) 17-Hydroxysteroids 800.522.4762 • www.gdx.net 16a-OH(E1) Estriol (E3) ENZYMATIC STEPS: 11-Keto-Androsterone 11-Keto-Etiocholanolone 3βHSD = 3beta-Hydroxysteroid dehydrogenase 4-OH (E1+E2) 5α = 5alpha-Reductase 17-Ketosteroids 4-MeO (E1+E2) 5β = 5beta-Reductase CYP11b1 = 11beta-Hydroxylase Hormones measurable 11βHSD = 11beta-Hydroxysteroid dehydrogenase Estrogen Metabolites 17βHSD = 17beta-Hydroxysteroid dehydrogenase by Genova Diagnostics: 17,20 Lyase = 17,20 Desmolase CYPc17 = 17alpha-Hydroxylase Measurable in Urine CYP19 = Aromatase CYP21 = 21-Hydroxylase ESTROGEN METABOLISM: Measurable in Blood 1A1 = Cytochrome p450 1A1 (CYP1A1) 3A4 = Cytochrome p450 3A4 (CYP3A4) 1B1 = Cytochrome p450 1B1 (CYP1B1) Measurable in Saliva COMT = Catechol-O-Methyl-transferase © 2016 Genova Diagnostics • e,po,steropath,031016 *Serum Testosterone Melatonin (x3) Progesterone (x3) Estrogens (x3) (E1, E2, E3) Testosterone Progesterone Melatonin (x3) Peri/Menopausal Females Estrogens (E1, -

Metabolomic Biomarkers in Urine of Cushing's Syndrome Patients
Article Metabolomic Biomarkers in Urine of Cushing’s Syndrome Patients Alicja Kotłowska 1,*, Tomasz Puzyn 2, Krzysztof Sworczak 3, Piotr Stepnowski 4 and Piotr Szefer 1 1 Department of Food Sciences, Faculty of Pharmacy, Medical University of Gdańsk, Al. Gen. J. Hallera 107, 80-416 Gdańsk, Poland; [email protected] 2 Laboratory of Environmental Chemometrics, Faculty of Chemistry, University of Gdańsk, ul. Wita Stwosza 63, 80-308 Gdańsk, Poland; [email protected] 3 Department of Endocrinology and Internal Medicine, Medical University of Gdańsk, ul. Dębinki 7, 80-211 Gdańsk, Poland; [email protected] 4 Department of Environmental Analytics, Institute for Environmental and Human Health Protection, Faculty of Chemistry, University of Gdańsk, ul. Wita Stwosza 63, 80-308 Gdańsk, Poland; [email protected] * Correspondence: [email protected]; Tel./Fax: +48-58-349-3110 Academic Editors: Ting-Li (Morgan) Han Received: 5 December 2016; Accepted: 19 January 2017; Published: 29 January 2017 Abstract: Cushing’s syndrome (CS) is a disease which results from excessive levels of cortisol in the human body. The disorder is associated with various signs and symptoms which are also common for the general population not suffering from compound hypersecretion. Thus, more sensitive and selective methods are required for the diagnosis of CS. This follow-up study was conducted to determine which steroid metabolites could serve as potential indicators of CS and possible subclinical hypercortisolism in patients diagnosed with so called non-functioning adrenal incidentalomas (AIs). Urine samples from negative controls (n = 37), patients with CS characterized by hypercortisolism and excluding iatrogenic CS (n = 16), and patients with non-functioning AIs with possible subclinical Cushing’s syndrome (n = 25) were analyzed using gas chromatography-mass spectrometry (GC/MS) and gas chromatograph equipped with flame ionization detector (GC/FID). -

Adrenarche and Puberty in Children with Classic Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency
Original Paper HORMONE Horm Res Paediatr 2011;76:400–410 Received: July 4, 2011 RESEARCH IN DOI: 10.1159/000333696 Accepted: September 27, 2011 PÆDIATRIC S Published online: November 24, 2011 Adrenarche and Puberty in Children with Classic Congenital Adrenal Hyperplasia due to 21-Hydroxylase Deficiency a a a b Thomas M.K. Völkl Lisa Öhl Manfred Rauh Christof Schöfl a Helmuth G. Dörr a Division of Pediatric Endocrinology and Diabetology, Department of Pediatrics and Adolescent Medicine, and b Division of Endocrinology and Diabetology, First Department of Internal Medicine, Friedrich Alexander University of Erlangen-Nuremberg, Erlangen-Nuremberg , Germany Key Words was normal. Conclusions: Pubarche and adrenarche are dis- Congenital adrenal hyperplasia ؒ 21-Hydroxylase ؒ sociated in classic CAH: earlier pubarche, gonadarche and Adrenarche, puberty thelarche, respectively, in both sexes contrast with the ab- sence of typical adrenarche. Copyright © 2011 S. Karger AG, Basel Abstract There have been only a few studies on adrenarche in girls with classic congenital adrenal hyperplasia (CAH) showing Introduction that dehydroepiandrosterone sulfate (DHEAS) levels did not rise at the physiological age of adrenarche. Objective: Lon- Congenital adrenal hyperplasia (CAH) due to 21-hy- gitudinal analysis of serum DHEAS levels and Tanner stages droxylase deficiency is associated with abnormally low in CAH children. Design: We studied 98 CAH patients (52 fe- cortisol and low (salt wasting, SW-CAH) or normal aldo- males), aged between 1 month and 18.0 years. All patients sterone (simple virilizing, SV-CAH) production [1, 2] . had genetically proven classic CAH and received steroid sub- Due to an intact feedback system with activation of the stitution therapy. -

NON-INVASIVE MONITORING of REPRODUCTION in ASIAN ELEPHANTS (Eleohas Maximus) by URINARY ENDOCRINE ANALYSIS
NON-INVASIVE MONITORING OF REPRODUCTION IN ASIAN ELEPHANTS (Eleohas maximus) BY URINARY ENDOCRINE ANALYSIS A Thesis Presented to The Faculty of Graduate Studies of University College London by CHERYL NffiMULLER In partial fulfillment of requirements for the degree of Doctor of Philosphy January, 1994 ® Cheryl Niemuller, 1994 ProQuest Number: 10016751 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest 10016751 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 ABSTRACT NON-INVASIVE MONITORING OF REPRODUCTION IN ASIAN ELEPHANTS (Eleohas maximiis) BY URINARY ENDOCRINE ANALYSIS Cheryl Niemuller Supervisors: University College London Dr. H.J. Shaw 1994 Prof. J.K. Hodges The development of an enzymeimmunoassay for 5j8 pregnanetriol and its use for non-invasive monitoring of reproductive cycles and pregnancy in Asian elephants is described. Gas chromatography mass spectrometry (GCMS) and high performance liquid chromatography (HPLC) confirmed the presence of 5/3- pregnane-3a,17a,20a/i3 triols as the two most abundant urinary progesterone metabolites during pregnancy and the oestrous cycle. The assay developed utilized the antiserum anti-5)3-pregnane-17a,20a-diol-3a-yl glucuronide-carboxy- methyloxime-BSA and 4-pregnene-17a,20a-diol-3-one-HRP as the enzyme label. -

Plasma Progesterone and 17-Hydroxyprogesterone with Congenital Adrenal Hyperplasia
Plasma Progesterone and 17- Hydroxyprogesterone in Normal Men and Children with Congenital Adrenal Hyperplasia CHARLES A. STRoTr, TERUYA YOSHIMI, and MORTIMER B. LIPSETT From the Endocrinology Branch, National Cancer Institute, Bethesda, Maryland 20014 A B S T R A C T Plasma 17-hydroxyprogesterone (17- tively small amounts by normal subjects but may have OHP) concentrations in normal men averaged 0.094 high secretion rates when there are distal enzymatic ,ug/100 ml. Studies using suppressive doses of androgens blocks, such as in congenital adrenal hyperplasia (CAH). and glucocorticoids showed that 90% of the 17-OHP To study in greater detail the function of the steroid- originated from the Leydig cell. The 17-OHP production producing glands, we have examined the plasma con- rate was 1.8 mg/24 hr. Plasma 17-OHP has a marked centration and sources of plasma progesterone and 17- circadian variation, the 8 p.m. values being only 40% of OHP under varying conditions. We shall report here the 8 a.m. values. Plasma luteinizing hormone measured the utility of these measurements for investigating nor- in the same samples did not vary. mal Leydig cell function and adrenal cortical function in The adrenal cortex has the capacity to synthesize and CAH. secrete 17-OHP and progesterone since adrenocortico- trophic hormone (ACTH) caused a fourfold increase METHODS in these plasma steroids. In children with congenital Subjects. The normal men and women ranged in age adrenal hyperplasia, plasma 17-OHP levels were 50- from 20 to 47 yr. When circadian variation was examined, plasma samples were obtained after the subjects had been 200 times those of normal men and plasma progesterone in the recumbent position for at least 1 hr.