Medicaid Reform Legislation 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NBAF Final Environmental Impact Statement
NATIONAL BIO AND AGRO-DEFENSE FACILITY FINAL ENVIRONMENTAL IMPACT STATEMENT APPENDIX H COMMENT RESPONSE DOCUMENT DECEMBER 2008 U.S. DEPARTMENT OF HOMELAND SECURITY Chapter 1 – Comment Response Document NBAF Final Environmental Impact Statement Comment Response Document, Chapter 1 PUBLIC COMMENT PROCESS This chapter of the Comment Response Document describes the public comment process for the National Bio and Agro-Defense Facility (NBAF) Draft Environmental Impact Statement (EIS) and the procedures used in responding to those comments. Section 1.1 describes the various means through which comments were acquired. Section 1.2 discusses the public meeting format used to gather comments from the public. Section 1.3 describes the organization of this document and explains how the comments were categorized, addressed, and documented. Section 1.4 provides guidance to assist readers in locating comments and DHS responses. Section 1.5 presents the major issues raised in a majority of comments. In Section 1.6, the chapter concludes with a list of significant changes to the EIS resulting from public comments. 1.1 INTRODUCTION In June 2008, the U.S. Department of Homeland Security (DHS) published the National Bio and Agro-Defense Facility (NBAF) Draft Environmental Impact Statement (EIS), which analyzed six action alternatives as well as a No Action Alternative. The action alternatives include construction and operation of the proposed NBAF at one of the following site alternatives: (1) South Milledge Avenue Site, Athens, Georgia; (2) Manhattan Campus Site, Manhattan, Kansas; (3) Flora Industrial Park Site, Flora, Mississippi; (4) Plum Island Site, Plum Island, New York; (5) Umstead Research Farm Site, Butner, North Carolina; and (6) Texas Research Park Site, San Antonio, Texas. -
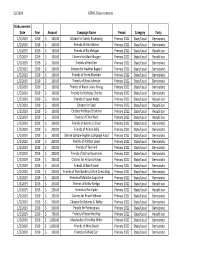
Astrazeneca's PAC Contributions Report: First
Q1 2019 AZPAC Disbursements Disbursement Date Year Amount Campaign Name Period Category Party 1/2/2019 2019$ 100.00 Citizens for Sandy Rosenberg Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Erek Barron Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Ric Metzgar Primary 2022 State/Local Republican 1/2/2019 2019$ 100.00 Citizens for Matt Morgan Primary 2022 State/Local Republican 1/2/2019 2019$ 100.00 Friends of Ken Kerr Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Citizens for Heather Bagnall Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Harry Bhandari Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Steve Johnson Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Karen Lewis Young Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends for Nicholas Charles Primary 2022 State/Local Democratic 1/2/2019 2019$ 100.00 Friends of Susan Krebs Primary 2022 State/Local Republican 1/2/2019 2019$ 100.00 Citizens for Saab Primary 2022 State/Local Republican 1/2/2019 2019$ 100.00 Citizens for Brian Chisholm Primary 2022 State/Local Republican 1/2/2019 2019$ 150.00 Friends of Chris West Primary 2022 State/Local Republican 1/2/2019 2019$ 200.00 Friends of Bonnie Cullison Primary 2022 State/Local Democratic 1/2/2019 2019$ 200.00 Friends of Ariana Kelly Primary 2022 State/Local Democratic 1/2/2019 2019$ 200.00 Sheree Sample‐Hughes Campaign Fund Primary 2022 State/Local Democratic 1/2/2019 2019$ 200.00 Friends of Robbyn Lewis -

2014 Political Corporate Contributions 2-19-2015.Xlsx
2014 POLITICAL CORPORATE CONTRIBUTIONS Last Name First Name Committee Name State Office District Party 2014 Total ($) Alabama 2014 PAC AL Republican 10,000 Free Enterprise PAC AL 10,000 Mainstream PAC AL 10,000 Collins Charles Charlie Collins Campaign Committee AR Representative AR084 Republican 750 Collins‐Smith Linda Linda Collins‐Smith Campaign Committee AR Senator AR019 Democratic 1,050 Davis Andy Andy Davis Campaign Committee AR Representative AR031 Republican 750 Dotson Jim Jim Dotson Campaign Committee AR Representative AR093 Republican 750 Griffin Tim Tim Griffin Campaign Committee AR Lt. Governor AR Republican 2,000 Rapert Jason Jason Rapert Campaign Committee AR Senator AR035 Republican 1,000 Rutledge Leslie Leslie Rutledge Campaign Committee AR Attorney General AR Republican 2,000 Sorvillo Jim Jim Sorvillo Campaign Committee AR Representative AR032 Republican 750 Williams Eddie Joe GoEddieJoePAC AR Senator AR029 Republican 5,000 Growing Arkansas AR Republican 5,000 Senate Victory PAC AZ Republican 2,500 Building Arizona's Future AZ Democratic 5,000 House Victory PAC AZ Republican 2,500 Allen Travis Re‐Elect Travis Allen for Assembly 2014 CA Representative CA072 Republican 1,500 Anderson Joel Tax Fighters for Joel Anderson, Senate 2014 CA Senator CA038 Republican 2,500 Berryhill Tom Tom Berryhill for Senate 2014 CA Senator CA008 Republican 2,500 Bigelow Frank Friends of Frank Bigelow for Assembly 2014 CA Representative CA005 Republican 2,500 Bonin Mike Mike Bonin for City Council 2013 Officeholder Account CA LA City Council -

Baltimore City Redistricting Reform Commission Meeting University of Baltimore Law School 1401 N
Baltimore City Redistricting Reform Commission Meeting University of Baltimore Law School 1401 N. Charles St., Baltimore, MD 21201 Judge Alex Williams - Calls meeting to order at 1:11pm Judge Alex Williams - Welcomes everyone to Baltimore. I am the co – chair, we are here to hear from the public and stakeholder organizations. We have been at this two years now. The Commission was appointed by Governor Hogan. Gerrymandering is an issue haunting Maryland. Both congressional and legislative districts are drawn in an unfair manner. We have members of the commission joining us here today. Governor Hogan appointed seven members to the Commission of whom three are Democrats, three are Republicans and one is not affiliated with a political party. The Governor selected Walter Olson, a Republican from Frederick County and Senior Fellow at the Cato Institute, and myself, a Democrat from Prince George’s County and former U.S. District Court Judge, to serve as co-chairmen of the Commission. Additional members appointed by the Governor include Tessa Hill-Aston, President of the Baltimore City branch of the NAACP, Michael Goff, who is the President of the Northeast-Midwest Institute and a board member at Common Cause Maryland. Christopher Summers, who is President of the Maryland Public Policy Institute. Carol Ramirez, a Bethesda resident and small business owner, and Ashley Oleson, Administrator for the League of Women Voters of Maryland were also added to the commission by Governor Hogan. President of the Maryland Senate Thomas V. Mike Miller, Jr. appointed Senator Joan Carter Conway who represents District 43 in Baltimore City and serves as Chair of the Education, Health and Environmental Affairs Committee. -

Legislative Guide Ejrodriquez/Adobe Stock
KENTUCKY ELECTRIC COOPERATIVES 2021 LEGISLATIVE GUIDE EJRODRIQUEZ/ADOBE STOCK Serving more than 1.5 million people in 117 of 120 Kentucky counties, Kentucky’s member-owned electric cooperatives are committed to improving the quality of life for their consumer-members. We encourage Kentuckians to engage with elected leaders and advocate for safe, reliable and affordable electricity. 1 TIM WEBB This 2021 Legislative Guide is provided as a public service by Co-ops work together to keep the power grid secure. Kentucky Electric Cooperatives, the statewide association When disasters strike, electric co-ops are always ready to that represents 26 co-ops that serve more than 1.5 million lend a hand. Kentuckians in 117 of the commonwealth’s 120 counties. We appreciate the service of elected leaders and other We work to educate elected leaders and advocate for government officials tasked with oversight of the energy policies that support our ability to provide safe, reliable and sector, and we are proud to be a trusted resource for any affordable electricity. questions about how public policy affects our ability to Each of Kentucky’s local electric cooperatives is locally effectively serve our members. owned and controlled by the consumer-members who are We encourage you to pull out this guide, save it and served by that local co-op. Each co-op was built by, belongs use it to contact elected leaders about issues that are to and is led by people in its own community. important to you. In that spirit, we encourage local co-op members to join our grassroots portal to stay up to date and communicate with legislators about issues important to co-ops. -

March 23, 2020 Via Email Governor Andy Beshear Lt. Governor
March 23, 2020 Via email Governor Andy Beshear Lt. Governor Jacqueline Coleman The Honorable Robert Stivers The Honorable Morgan McGarvey The Honorable David Osborne The Honorable Joni Jenkins Dear Governor Beshear, Lt. Governor Coleman and Legislative Leaders: This letter is intended to provide additional recommendations urgently requested by Kentucky’s nonprofit sector as a follow up to the letter originally submitted via email on March 17 (see below). The original recommendations and these additions are critical to the nonprofit sector’s ability to weather this storm and continue to serve Kentucky’s most vulnerable during this crisis. Disruptions in state grants and contracts could trigger massive layoffs or even permanently shut down organizations providing health services, food assistance, emergency shelter, senior care, emergency child-care, mental health, substance use disorder treatment and other essential services in the Commonwealth. In addition to the original recommendations (see below), we recommend: • Special attention and funding are needed for the homeless population in Kentucky. Homeless individuals are not able to safely practice social distancing, wash their hands or take other recommended precautions to stay safe. They are also more likely to have underlying health conditions and a high volume of infection among this population will seriously stress our health system. Emergency funding to agencies that provide housing, healthcare and other services to homeless populations are needed, as well as creative responses to relieve existing shelters that do not have enough distance between beds to keep the virus from spreading. • We urge the Commonwealth to maintain customary payments to nonprofits that have current grants and contracts. -
Scorecard 2011-2014 2
Report on th e MARYLAND GENERAL ASSEMBLY SCORECARD 2011-2014 2 2012 2014 2011-2014 Maryland Legislation SB 317 & HB 131 – Retail Pet Stores SB 827 & HB 1124 – Roadside Zoos Requires retail pet stores to disclose information Establishes basic animal welfare and public safety SCORED BY about the puppies they sell and establishes requirements for facilities keeping big cats, bears Humane Society Legislative Fund remedies for consumers who purchase sick puppies and primates. from pet stores. Signed into Law. Sponsored by Senator Catherine & Maryland Votes For Animals Signed into Law. Sponsored by Senator Catherine Pugh and Delegate Eric Luedtke Pugh and Delegate Nic Kipke SB 659 & HB 665 – Surgical Procedures on Dogs SB 465 & HB 393 – Shark Fins 2011 Prohibits ear cropping, tail docking, dewclaw Bans the possession, distribution and sale of shark fins. removal and surgical births of dogs, unless done by SB 115 & HB 227 – Animal Cruelty Passed the Senate. Sponsored by Senator Brian a veterinarian under anesthesia. Authorizes a court to prohibit someone convicted Frosh and Delegate Eric Luedtke Signed into Law. Sponsored by Senator Lisa of animal cruelty from owning an animal as a Gladden and Delegate Ben Kramer condition of probation. SB 203 & HB 484 – Cost of Care SB 660 & HB 667 – Devocalization Signed into law. Sponsored by Senator Jim Robey Authorizes a court to require someone convicted of and Delegate Jeff Waldstreicher animal cruelty to pay for the costs of caring for the Prohibits devocalization of dogs and cats unless animals during the course of the trial. medically necessary. SB 747 & HB 407 – Pet Protective Orders Passed the Senate. -

February 10, 2020 Via Electronic Communication David W. Osborne
February 10, 2020 Via Electronic Communication David W. Osborne David Meade Chair, Committee on Committees Vice-Chair, Committee on Committees Kentucky House of Representatives Kentucky House of Representatives [email protected] [email protected] Re: Letter in Support of HB114 Dear Representatives Osborne and Meade: Aimed Alliance is a 501(c)(3) non-profit health policy organization that seeks to protect and enhance the rights of health care consumers and providers. We are writing in support of HB114, and we ask that you approve the bill, with a few changes, for a full vote before the legislature. Historically, privately insured individuals who cannot afford their copayments or coinsurance have been able to obtain aid from copayment assistance programs –programs in which a pharmaceutical manufacturer may offer cost-sharing assistance, typically in the form of a coupon card, to an individual to ease the burden of high out-of-pocket costs. Traditionally, the coupon card contributes also toward the patient’s deductible and maximum out-of-pocket limit. These programs have been especially helpful for individuals enrolled in high deductible health plans (HDHPs) in which the patient is responsible for high out-of-pocket costs until the deductible is reached. Increasingly, HDHPs are the only option for many Americans; many employers and marketplace exchanges only offer HDHPs.1 Health plans are increasingly implementing copay accumulator programs, which prevent the value of a drug manufacturer’s coupon from counting toward a patient’s deductible and maximum out-of-pocket limit.2 Under such programs, once copayment assistance runs out, the plan enrollee is again faced with an inability to afford his or her medication. -

2014 Report of Political Financial Support
2014 2014 Lilly Political Contributions As a biopharmaceutical company that treats serious diseases, Lilly plays an important role in public health and its related policy debates. It is important that our company shapes global public policy debates on issues specific to the people we serve and to our other key stakeholders including shareholders and employees. Our engagement in the political arena helps address the most pressing issues related to ensuring that patients have access to needed medications—leading to improved patient outcomes. Through public policy engagement, we provide a way for all of our locations globally to shape the public policy environment in a manner that supports access to innovative medicines. We engage on issues specific to local business environments (corporate tax, for example). Based on our company’s strategy and the most recent trends in the policy environment, our company has decided to focus on three key areas: innovation, health care delivery, and pricing and reimbursement. More detailed information on key issues can be found in our 2014 Corporate Responsibility Update. Through our policy research, development, and stakeholder dialogue activities, Lilly develops positions and advocates on these issues. Government actions such as price controls, pharmaceutical manufacturer rebates, and access to Lilly medicines affect our ability to invest in innovation. Lilly has a comprehen- sive government relations operation to have a voice in the public policymaking process at the federal, state, and local levels. Lilly is committed to participating in the political process as a responsible corporate citizen to help inform the U.S. debate over health care and pharmaceutical innovation. -

East Stand (A)
EAST STAND (A) ACHIE ATWELL • GEORGE BOGGIS • JOHN ELLIOTT • DAVID BREWSTER • GILLIAN ROBINS • DESMOND DESHAUT • PETER CWIECZEK • JAMES BALLARD • PETER TAYLOR • JOHN CLEARY • MARK LIGHTERNESS • TERENCE KERRISON • ANTHONY TROCIAN • GEORGE BURT • JESSICA RICHARDSON • STEVE WICK • BETHAN MAYNARD • MICHAEL SAMMONS • DAN MAUGHAN • EMILY CRANE • STEFANO SALUSTRI • MARTIN CHIDWICK • SOPHIA THURSTON • RICHARD HACK • PHILIP PITT • ROBERT SAMBIDGE • DEREK VOLLER • DAVID PARKINSON • LEONARD COONEY • KAREN PARISH • KIRSTY NORFOLK • SAMUEL MONAGHAN • TONY CLARKE • RAY MCCRINDLE • MIKKEL RUDE • FREDERIC HALLER • JAMIE JAXON • SCOTT JASON • JACQUELINE DUTTON • RICHARD GRAHAM • MATTHEW SHEEHAN • EMILY CONSTABLE • TERRY MARABLE • DANNY SMALLDRIDGE • PAULA GRACE • JOHN ASHCROFT • BARNABY BLACKMAN • JESSICA REYNOLDS • DENNIS DODD • GRAHAM HAWKES • SHAUN MCCABE • STEPHEN RUGGIERO • ALAN DUFFY • BEN PETERS • PAUL SHEPPARD • SIMON WISE • IAN SCOTT • MARK FINSTER • CONNOR MCCLYMONT • JOSEPH O’DRISCOLL • FALCON GREEN • LEAH FINCHAM • ROSS TAYLOR • YONI ADLER • SAMUEL LENNON • IAN PARSONS • GEORGE REILLY • BRIAN WINTER • JOSEPH BROWN • CHARLIE HENNEY • PAUL PRYOR • ROBERT BOURKE • DAREN HALL • DANIEL HANBURY • JOHN PRYOR • BOBBY O’DONOGHUE • ROBERT KNIGHT • BILLY GREEN • MAISIE-JAE JOYCE • LEONARD GAYLE • KEITH JONES • PETER MOODY • ANDY ATWELL DANIEL SEDDON • ROBBIE WRIGHT • PAUL BOWKER • KELLY CLARK • DUNCAN LEVERETT • BILL SINGH • RODNEY CASSAR • ASHER BRILL • MARTIN WILLIAMS • KEVIN BANE • TERRY PORTER • GARETH DUGGAN • DARREN SHEPHERD • KEN CAMPBELL • PHYLLIS -

DRAFT ---APTA Maryland – Key Legislators
2020 PAC Contribution Budget: $4,000 DRAFT ---- APTA Maryland – Key Legislators Current Donations: $3,600 (As of October 15, 2020) Given Suggested Current Cycle Title First Name Last Name District Committee Amount (1/1/2019 Upcoming Event(s): Campaign Info 2020 thru 12/31/2022) Color Code Key: Influential Leaders: highlighted yellow; FIN Health Subcommittee members: green; EHEA Health Subcommittee members: orange ; HGO Health Occupations Subcommittee members: red; HGO Insurance Subcommittee members: blue; Senate and House Leaders: pink Citizens for Bill Ferguson C/o Martin Lauer Associates 1215 E. Fort Avenue, Suite 106 Senate Pres Bill Ferguson D Baltimore, MD 21230 President 410-547-8884 [email protected] billforbaltimore.com/november7 District 3 Friends of Ron Young Sen. Ron Young D Frederick Senate $200 P.O. Box 724 County Frederick, MD 21705 Citizens for Delores Kelley FIN – Chair District 10 c/o Rice Consulting Subcom Sen. Delores Kelley D Baltimore $100 17 W. Courtland Street Chair, County Suite 210 Health Bel Air, MD 21014 Citizens for Brian Feldman District 15 FIN - Vice PO Box 34408 Sen. Brian Feldman D Montgomery $100 Ch Bethesda, MD 20827, MD 20827 County 301-517-5719 November 10, 2020; Friends of Malcolm Augustine District 47 7:00pm-8:00pm PO Box 272 Sen. Malcolm Augustine D Prince George's FIN Virtual Fundraiser Bladensburg, MD 20710 County $47, $100, $250, $500, 301-383-8011 $1,000, $2,500 www.malcolmaugustine.com Page 1 of 11 2020 PAC Contribution Budget: $4,000 Current Donations: $3,600 Given Suggested Current Cycle Title First Name Last Name District Committee Amount (1/1/2019 Upcoming Event(s): Campaign Info 2020 thru 12/31/2022) Color Code Key: Influential Leaders: highlighted yellow; FIN Health Subcommittee members: green; EHEA Health Subcommittee members: orange ; HGO Health Occupations Subcommittee members: red; HGO Insurance Subcommittee members: blue; Senate and House Leaders: pink www.malcolmaugusti ne.com/augustine11_ 10 Friends of Pam Beidle c/o Rice Consulting, 17 W Courtland District 32 St., Suite 210 Sen. -

February 16, 2020 the Honorable Maggie Mcintosh, Chairman House
February 16, 2020 The Honorable Maggie McIntosh, Chairman House Appropriations Committee 6 Bladen Street, Suite 121 Annapolis, Maryland 21401 The Honorable Anne Kaiser, Chairman House Ways and Means Committee 6 Bladen Street, Suite 131 Annapolis, Maryland 21401 Dear Madame Chairs, As you are aware, at Noon tomorrow, February 7, 2012, four committees in the General Assembly will hold a joint hearing on HB 1300/SB 1000 – Blueprint for Maryland’s Future – Implementation. This is one of the most significant pieces of legislation the Maryland General Assembly has considered in a generation; not only because of the fundamental changes it is said to make in our education system but also for the tremendous price tag that it carries. For better or for worse, this legislation will have a staggering impact on Maryland for years to come. It is our duty, as the elected representatives who will consider and ultimately vote on this monumental piece of legislation, to do so thoughtfully and carefully. It is critical that this legislation is thoroughly vetted and analyzed, and that we hear from all parties who will be impacted by this legislation. It is just as critical that we, and the public, have access to all of the information and analysis available. It is with an abundance of concern that, at this juncture, this legislation appears to be moving forward at a rushed pace, that we write to you today. As we write this letter, the hearing for this bill is less than 24 hours away. And yet, after more than three years of meetings, decisions, and recommendations from the Kirwan Commission and months of planning and analysis by the Department of Legislative Services, there is no Fiscal Note available; neither to the members sitting on the Committees nor to the public.