5Th Common Review Mission- Chhattisgarh
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
English Lotlist 2021-I Dated 07.11.2020 (954 Lot) 2
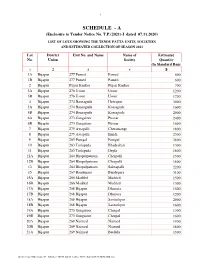
1 SCHEDULE - A (Enclosure to Tender Notice No. T.P.(2021)-I dated 07.11.2020) LIST OF LOTS SHOWING THE TENDU PATTA UNITS, SOCIETIES AND ESTIMATED COLLECTION OF SEASON 2021 Lot District Unit No. and Name Name of Estimated No. Union Society Quantity (In Standard Bags) 1 2 3 4 5 1A Bijapur 277 Pamed Pamed 600 1B Bijapur 277 Pamed Pamed 600 2 Bijapur Pujari Kanker Pujari Kanker 700 3A Bijapur 276 Usoor Usoor 1200 3B Bijapur 276 Usoor Usoor 1200 4 Bijapur 274 Bansaguda Heerapur 3000 5A Bijapur 274 Bansaguda Korsaguda 1600 5B Bijapur 274 Bansaguda Korsaguda 2000 6A Bijapur 273 Gangaloor Pusnar 2400 6B Bijapur 273 Gangaloor Pusnar 1600 7 Bijapur 275 Awapalli Cheramangi 1800 8 Bijapur 275 Awapalli Ilmidi 2300 9 Bijapur 265 Pamgal Pamgal 2800 10 Bijapur 263 Tarlaguda Bhadrakali 1300 11 Bijapur 263 Tarlaguda Depla 1800 12A Bijapur 264 Bhopalpatnam Cherpalli 1500 12B Bijapur 264 Bhopalpatnam Cherpalli 1800 13 Bijapur 264 Bhopalpatnam Saknapalli 2200 15 Bijapur 267 Bandepara Bandepara 3100 16A Bijapur 266 Madded Madded 1500 16B Bijapur 266 Madded Madded 1300 17A Bijapur 268 Bijapur Dhanora 1500 17B Bijapur 268 Bijapur Dhanora 1200 18A Bijapur 268 Bijapur Santoshpur 2000 18B Bijapur 268 Bijapur Santoshpur 1600 19A Bijapur 273 Gangaloor Cherpal 1300 19B Bijapur 273 Gangaloor Cherpal 1600 20A Bijapur 269 Naimed Naimed 1900 20B Bijapur 269 Naimed Naimed 1800 21A Bijapur 269 Naimed Berdela 1500 C:\Users\user\Desktop\T.P. Advance 2021\English_Lotlist_2021-I dated 07.11.2020 (954 Lot) 2 1 2 3 4 5 21B Bijapur 269 Naimed Berdela 1700 22A Bijapur 269 Naimed -

Pre-Feasibility Report of Granite
PRE-FEASIBILITY REPORT OF GRANITE (MINOR MINERAL) MINE Village – Kanhanpuri, Tehsil – Narharpur Dist. – Kanker, Chhattisgarh Area - 1.87 Hectare INTRODUCTION The commercial use of the term Black Granite is considerably broader than the geological use. In industry the term refer to true granite, granite gneiss and the intermediate member of the granite – gabbro series, gabbro, diabase, anorthosite , pyroxinite and dolerite called black granite, when used for polished dimension stone. Kanker is one of the large districts of Chhattisgarh and known to be densely forested and thinly populated by the tribes. The district is endowed with large number of economic rocks and minerals. There is a growing demand for Black Granite ( dolerite dyke ) and other basic rocks known as Black Granite in Kanker district. The applicant Vimal Lunia granted quarry lease for Black Granite in village – Kanhanpuri of District – Uttar Bastar ( Kanker.) The proposed area for which 1st Scheme of Mining is being prepared is located in the Jurisdiction of village – Kanhanpuri, Tahsil – Narharpur of District – Uttar Bastar ( Kanker ) , State – Chhattisgarh. There is a small but good deposit of “Black Granite” available in this village . The leased area was granted to the applicant Mr. Vimal Lunia 1st time on 2nd November 1998 for 10 years under the Madhya Pradesh Minor Mineral Rules 1996. As per the rule 18 (2) GDCR 1999 1st scheme of mining due for the period of 2014-15 to 2018-19, for this reason lessee Shri. Vimal Lunia of Jagdalpur, District – Bastar, State – Chhattisgarh submitting the 1st scheme of mining for their existing Kanhanpuri Black Granite Mine by utilizing the services of an Indian Bureau of Mines Nagpur , approved Recognized Qualified Person Mr. -

Brief Industrial Profile of Kanker District
lR;eso t;rs Government of India Ministry of MSME Brief Industrial Profile of Kanker District Carried out by MSME-Development Institute, Raipur (Ministry of MSME, Govt. of India,) Phone :- 0771- 2427719 /2422312 Fax: 0771 - 2422312 e-mail: [email protected] Web- www.msmediraipur.gov.in Contents S. No. Topic Page No. 1. General Characteristics of the District 1 1.1 Location & Geographical Area 1 1.2 Topography 1 1.3 Availability of Minerals. 1 1.4 Forest 2 1.5 Administrative set up 2 2. District at a glance 3 2.1 Existing Status of Industrial Area in the District Kanker 6 3. Industrial Scenario Of Kanker 6 3.1 Industry at a Glance 6 3.2 Year Wise Trend Of Units Registered 7 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The 8 District 3.4 Large Scale Industries / Public Sector undertakings 8 3.5 Major Exportable Item 8 3.6 Growth Trend 8 3.7 Vendorisation / Ancillarisation of the Industry 8 3.8 Medium Scale Enterprises 9 3.8.1 List of the units in Kanker & near by Area 9 3.8.2 Major Exportable Item 9 3.9 Service Enterprises 9 3.9.1 Potentials areas for service industry 9 3.10 Potential for new MSMEs 9 4. Existing Clusters of Micro & Small Enterprise 10 4.1 Detail Of Major Clusters 10 4.1.1 Manufacturing Sector 10 4.1.2 Service Sector 10 4.2 Details of Identified cluster 10 5. General issues raised by industry association during the course of 10 meeting 6 Steps to set up MSMEs 13 Brief Industrial Profile of Kanker District 1. -

Mahanadi River Basin
The Forum and Its Work The Forum (Forum for Policy Dialogue on Water Conflicts in India) is a dynamic initiative of individuals and institutions that has been in existence for the last ten years. Initiated by a handful of organisations that had come together to document conflicts and supported by World Wide Fund for Nature (WWF), it has now more than 250 individuals and organisations attached to it. The Forum has completed two phases of its work, the first centring on documentation, which also saw the publication of ‘Water Conflicts in MAHANADI RIVER BASIN India: A Million Revolts in the Making’, and a second phase where conflict documentation, conflict resolution and prevention were the core activities. Presently, the Forum is in its third phase where the emphasis of on backstopping conflict resolution. Apart from the core activities like documentation, capacity building, dissemination and outreach, the Forum would be intensively involved in A Situation Analysis right to water and sanitation, agriculture and industrial water use, environmental flows in the context of river basin management and groundwater as part of its thematic work. The Right to water and sanitation component is funded by WaterAid India. Arghyam Trust, Bangalore, which also funded the second phase, continues its funding for the Forums work in its third phase. The Forum’s Vision The Forum believes that it is important to safeguard ecology and environment in general and water resources in particular while ensuring that the poor and the disadvantaged population in our country is assured of the water it needs for its basic living and livelihood needs. -

Pre-Feasibility Report
PRE-FEASIBILITY REPORT OF GRANITE (MINOR MINERAL) MINE Village – Kanhanpuri, Tehsil – Narharpur Dist. – Kanker, Chhattisgarh Area - 1.87 Hectare INTRODUCTION The commercial use of the term Black Granite is considerably broader than the geological use. In industry the term refer to true granite, granite gneiss and the intermediate member of the granite – gabbro series, gabbro, diabase, anorthosite , pyroxinite and dolerite called black granite, when used for polished dimension stone. Kanker is one of the large districts of Chhattisgarh and known to be densely forested and thinly populated by the tribes. The district is endowed with large number of economic rocks and minerals. There is a growing demand for Black Granite ( dolerite dyke ) and other basic rocks known as Black Granite in Kanker district. The applicant Vimal Lunia granted quarry lease for Black Granite in village – Kanhanpuri of District – Uttar Bastar ( Kanker.) The proposed area for which 1st Scheme of Mining is being prepared is located in the Jurisdiction of village – Kanhanpuri, Tahsil – Narharpur of District – Uttar Bastar ( Kanker ) , State – Chhattisgarh. There is a small but good deposit of “Black Granite” available in this village . The leased area was granted to the applicant Mr. Vimal Lunia 1st time on 2nd November 1998 for 10 years under the Madhya Pradesh Minor Mineral Rules 1996. As per the rule 18 (2) GDCR 1999 1st scheme of mining due for the period of 2014-15 to 2018-19, for this reason lessee Shri. Vimal Lunia of Jagdalpur, District – Bastar, State – Chhattisgarh submitting the 1st scheme of mining for their existing Kanhanpuri Black Granite Mine by utilizing the services of an Indian Bureau of Mines Nagpur , approved Recognized Qualified Person Mr. -

Notice Final Voter List Election2
Page 1 V O T E R L I S T - E L E C T I O N 2017 Rgn.N Father's/ Husband's Qualifin. S.No. Name Address District o. Name for Reg. 1 2 3 4 5 6 7 1 1 Kamlesh Chandra Shil Shri Kartik Chandra Shil P.V. No.-7, Po. Kapsi Kanker D.Pharma 2 2 Kunj Ram Shri Chamru Q.No. 29/7, Banki Mongra Korba D.Pharma 3 3 Tufail Ahmed Mohd. Israil Artision Block, Chirmiri (w) Korea D.Pharma 4 5 Pradeep Kumar Jain Shri Rambilash Jain Vill.- Keshgwan Korea D.Pharma Steel Nagar, Camp-I, Road No.- 5 6 Manish Kumar Agrawal Shri Khanjanchi Lal Durg D.Pharma 8, Post - Bhilai c/o. Prashant Medicose, Post - 6 7 Pratap Narayan Singh Shri Jag Narayan Singh Surguja D.Pharma Jarahi Morh, M/409 Near Bus Stand, Post - 7 8 Sawan Kumar Shri Surendra Kumar Bastar D.Pharma Kondagaon Q.No. - M/108, Rajgamar 8 9 Arun Kumar Mishra Shri Shiv Narayan Korba D.Pharma Colony, Post - Ompur Katainar, Q.No. CH/142, Post - 9 10 Ganga Prasad Shri Sukhi Ram Korba D.Pharma Banki Mongra Shri Birendra Kumar H.No. 31/551, Azad Chowk, 10 11 Vikas Shukla Raipur D.Pharma Shukla Brahaman Para, Raipur 11 12 Vinod Kumar Agrawal Shri Ratan Lal Hospital Colony. Post - Surajpur Surguja D.Pharma Sapna Garments, Sanjay 12 13 Smt. Shailja Gupta Shri Saran Gupta Korea D.Pharma Chowk, Post - Baikunthpur C.H.C. Kartala, Post - Bhaishma 13 15 Sushma Singh Shri Dhyan Singh Korba D.Pharma 495674 Qtr. -

Country Technical Note on Indigenous Peoples' Issues
Country Technical Note on Indigenous Peoples’ Issues Republic of India Country Technical Notes on Indigenous Peoples’ Issues REPUBLIC OF INDIA Submitted by: C.R Bijoy and Tiplut Nongbri Last updated: January 2013 Disclaimer The opinions expressed in this publication are those of the authors and do not necessarily represent those of the International Fund for Agricultural Development (IFAD). The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of IFAD concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The designations ‗developed‘ and ‗developing‘ countries are intended for statistical convenience and do not necessarily express a judgment about the stage reached by a particular country or area in the development process. All rights reserved Table of Contents Country Technical Note on Indigenous Peoples‘ Issues – Republic of India ......................... 1 1.1 Definition .......................................................................................................... 1 1.2 The Scheduled Tribes ......................................................................................... 4 2. Status of scheduled tribes ...................................................................................... 9 2.1 Occupation ........................................................................................................ 9 2.2 Poverty .......................................................................................................... -

11 06 Chhattisgarh (10.02.2016)
STATE REVIEWS Indian Minerals Yearbook 2014 (Part- I) 53rd Edition STATE REVIEWS (Chhattisgarh) (ADVANCE RELEASE) GOVERNMENT OF INDIA MINISTRY OF MINES INDIAN BUREAU OF MINES Indira Bhavan, Civil Lines, NAGPUR – 440 001 PHONE/FAX NO. (0712) 2565471 PBX : (0712) 2562649, 2560544, 2560648 E-MAIL : [email protected] Website: www.ibm.gov.in March, 2016 11-1 STATE REVIEWS CHHATTISGARH fields in India. Limestone occurs in Bastar, Bilaspur, Durg, Janjgir-Champa, Kawardha Mineral Resources (Kabirdham), Raigarh, Raipur & Rajnandgaon Chhattisgarh is the sole producer of tin districts; quartzite in Durg, Raipur, Rajnandgaon concentrates and is one of the leading producers & Raigarh districts; and talc/soapstone/steatite of coal, dolomite, bauxite and iron ore. The State in Durg & Kanker districts. accounts for about 36% tin ore, 18% iron ore Other minerals found in the State are (hematite), 17% coal and 11% dolomite resources corundum in Dantewada district; diamond and other of the country. Important mineral occurrences of gemstones in Raipur, Mahasamund and Dhamtari the State are bauxite in Bastar, Bilaspur, districts; fire clay in Bilaspur, Raigarh and Dantewada, Jashpur, Kanker, Kawardha Rajnandgaon districts; fluorite in Rajnandgaon (Kabirdham), Korba, Raigarh & Sarguja districts; district; garnet & marble in Bastar district; emerald china clay in Durg & Rajnandgaon districts; coal and gold in Raipur district; granite in Bastar, Kanker in Koria, Korba, Raigarh & Sarguja districts; & Raipur districts; quartz/silica sand in Durg, dolomite in Bastar, Bilaspur, Durg, Janjgir-Champa, Jashpur, Raigarh, Raipur & Rajnandgaon districts; Raigarh & Raipur districts; and iron ore and tin in Bastar & Dantewada districts (Table - 1 ). (hematite) in Bastar district, Bailadila deposit in The reserves/resources of coal are given in Table - 2. -

Basic Information of Urban Local Bodies – Chhattisgarh
BASIC INFORMATION OF URBAN LOCAL BODIES – CHHATTISGARH Name of As per As per 2001 Census 2009 Election S. Corporation/Municipality (As per Deptt. of Urban Growth No. of No. Class Area House- Total Sex No. of Administration & Development SC ST (SC+ ST) Rate Density Women (Sq. km.) hold Population Ratio Wards Govt. of Chhattisgarh) (1991-2001) Member 1 2 3 4 5 8 9 10 11 12 13 14 15 1 Raipur District 1 Raipur (NN) I 108.66 127242 670042 82113 26936 109049 44.81 6166 923 70 23 2 Bhatapara (NPP) II 7.61 9026 50118 8338 3172 11510 10.23 6586 965 27 8 3 Gobra Nayapara (NPP) III 7.83 4584 25591 3078 807 3885 21.84 3268 987 18 6 4 Tilda Nevra (NPP) III 34.55 4864 26909 4180 955 5135 30.77 779 975 18 7 5 Balodabazar (NPP) III 7.56 4227 22853 3851 1015 4866 31.54 3023 954 18 6 6 Birgaon (NPP) III Created after 2001 26703 -- -- -- -- -- -- 30 NA 7 Aarang (NP) IV 23.49 2873 16629 1255 317 1572 16.64 708 973 15 6 8 Simga (NP) IV 14.32 2181 13143 1152 135 1287 -3.01 918 982 15 5 9 Rajim (NP) IV Created after 2001 11823 -- -- -- -- -- -- 15 5 10 Kasdol (NP) IV Created after 2001 11405 -- -- -- -- -- -- 15 5 11 Bhatgaon (NP) V 15.24 1565 8228 1956 687 2643 -4.76 540 992 15 5 12 Abhanpur (NP) V Created after 2001 7774 -- -- -- -- -- -- 15 5 13 Kharora (NP) V Created after 2001 7647 -- -- -- -- -- -- 15 5 14 Lavan (NP) V Created after 2001 7092 -- -- -- -- -- -- 15 5 15 Palari (NP) V Created after 2001 6258 -- -- -- -- -- -- 15 5 16 Mana-kemp (NP) V Created in 2008-09 8347 -- -- -- -- -- -- 15 5 17 Fingeshwar (NP) V Created in 2008-09 7526 -- -- -- -- -- -- 15 5 18 Kura (NP) V Created in 2008-09 6732 -- -- -- -- -- -- 15 5 19 Tudara (NP) V Created in 2008-09 6761 -- -- -- -- -- -- 15 5 20 Gariyaband (NP) V Created in 2008-09 9762 -- -- -- -- -- -- 15 5 21 Chura (NP) VI Created in 2008-09 4869 -- -- -- -- -- -- 15 5 22 BiIlaigarh (NP) VI Created in 2008-09 4896 -- -- -- -- -- -- 15 5 2 Dhamtari District 23 Dhamtari (NPP) II 23.40 15149 82111 7849 7521 15370 18.39 3509 991 36 12 18 RCUES, Lucknow Name of As per As per 2001 Census 2009 Election S. -
Common Service Center List
CSC Profile Details Report as on 15-07-2015 SNo CSC ID District Name Block Name Village/CSC name Pincode Location VLE Name Address Line 1 Address Line 2 Address Line 3 E-mail Id Contact No 1 CG010100101 Durg Balod Karahibhadar 491227 Karahibhadar LALIT KUMAR SAHU vill post Karahibhadar block dist balod chhattisgarh [email protected] 8827309989 VILL & POST : NIPANI ,TAH : 2 CG010100102 Durg Balod Nipani 491227 Nipani MURLIDHAR C/O RAHUL COMUNICATION BALOD DISTRICT BALOD [email protected] 9424137413 3 CG010100103 Durg Balod Baghmara 491226 Baghmara KESHAL KUMAR SAHU Baghmara BLOCK-BALOD DURG C.G. [email protected] 9406116499 VILL & POST : JAGANNATHPUR ,TAH : 4 CG010100105 Durg Balod JAGANNATHPUR 491226 JAGANNATHPUR HEMANT KUMAR THAKUR JAGANNATHPUR C/O NIKHIL COMPUTER BALOD [email protected] 9479051538 5 CG010100106 Durg Balod Jhalmala 491226 Jhalmala SMT PRITI DESHMUKH VILL & POST : JHALMALA TAH : BALOD DIST:BALOD [email protected] 9406208255 6 CG010100107 Durg Balod LATABOD LATABOD DEKESHWAR PRASAD SAHU LATABOD [email protected] 9301172853 7 CG010100108 Durg Balod Piparchhedi 491226 PIPERCHEDI REKHA SAO Piparchhedi Block: Balod District:Balod [email protected] 9907125793 VILL & POST : JAGANNATHPUR JAGANNATHPUR.CSC@AISEC 8 CG010100109 Durg Balod SANKARAJ 491226 SANKARAJ HEMANT KUMAR THAKUR C/O NIKHIL COMPUTER ,TAH : BALOD DIST: BALOD TCSC.COM 9893483408 9 CG010100110 Durg Balod Bhediya Nawagaon 491226 Bhediya Nawagaon HULSI SAHU VILL & POST : BHEDIYA NAWAGAON BLOCK : BALOD DIST:BALOD [email protected] 9179037807 10 CG010100111 -

About Chhattisgarh
About Chhattisgarh Map Chhatisgarh state and districts (Stand 2007) At the time of separation from Madhya Pradesh, Chhattisgarh originally had 16 districts. Two new districts: Bijapur and Narayanpur were carved out on May 11, 2007[1] and nine new districts on Jan 1, 2012. The new districts have been created by carving out the existing districts to facilitate more targeted, focused and closer administration. These districts have been named Sukma, Kondagaon, Balod, Bemetara, Baloda Bazar, Gariaband, Mungeli, Surajpur and Balrampur[2] Contents [hide] 1 Background 2 Administrative history 3 Districts of Chhattisgarh 4 References 5 External links Background[edit] A district of an Indian state is an administrative geographical unit, headed by a district magistrate or a deputy commissioner, an officer belonging to the Indian Administrative Service. The district magistrate or the deputy commissioner is assisted by a number of officials belonging to different wings of the administrative services of the state. A superintendent of Police, an officer belonging to Indian Police Service is entrusted with the responsibility of maintaining law and order and related issues. Administrative history Before Indian independence, present-day Chhattisgarh state was divided between the Central Provinces and Berar, a province of British India, and a number of princely states in the north, south, and east, which were part of the Eastern States Agency. The British province encompassed the central portion of the state, and was made up of three districts, Raipur, Bilaspur, and Durg, which made up the Chhattisgarh Division of the Central Provinces. Durg District was created in 1906 out of the eastern portion of Raipur District. -

Publication No. 109 EDUCATIONAL STATISTICS INDIAN STATES 1946
Ministry of Education BUREAU OF EDUCATION, INDIA Publication No. 109 EDUCATIONAL STATISTICS INDIAN STATES 1946-47 PART II PrBUBBlD BT TBI MAHAQIH OF I'l'BUOlTlOSH, DlLHI PBIHTH' IB IWDU BY THB MANAOKB, GOTBBBMWIT OF IBTU PBBSS StML4, ]9fil PREFACE The present publication constitutes Part II of an earlier publication entitled " Educational Statistics, Indian States, 1946-47, Part I ". It rontains information on education for I94G-47 in renpijut of 45 former Indian States. The form in which information has been presented in this volumi' has been somewhat modified and improved as compared to Part I. It is hoped that it will be found useful by educationists and the public. I take this opportunity to express my gratitude to the State authori• ties who have supplied the inlornvition on which this account is based. TARA CHAND, NEW DELHI : Educational Adviser to the The 12th June, 1951. Government of India. TABLE OF CONTENTS Explanatioiu , (iii) Educational Statistics Name of the State-*- Athsgarh 1-2 Athmalik 2-3 Bamra 3-5 Banaras 6-7 Banairara 7-8 Baramba 8-10 Baudh 10-12 12-la •BhopJil 10-16 Booai 16-17 Cbbuikhadan 17-20 Cooob-Behor 20-22 Datia 22-23 Dh«okanal 23-26 Dholpor 25-20 HJndol 20-28 J^pur Jbalawar 28-29 Jodbpur 30-31 Kanker 31 EeoDJhar 32-34 Khandpara 34-35 Korea 35-37 Kotah 37-38 Katch Lob am 41-4S Hakrai 4M3 Mysore 43-45 Nagod 45-40 40^7 Naningpor 47-48 NaT«g»rh 48 . NOgiri . (ii) Name of the State—contd, PAGES Pallahara .