Elucidating the Roles of Il-15 in the Tumor Microenvironment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Research and Exchanges Board Records
International Research and Exchanges Board Records A Finding Aid to the Collection in the Library of Congress Prepared by Karen Linn Femia, Michael McElderry, and Karen Stuart with the assistance of Jeffery Bryson, Brian McGuire, Jewel McPherson, and Chanté Wilson-Flowers Manuscript Division Library of Congress Washington, D.C. 2011 International Research and Exchanges Board Records Page ii Collection Summary Title: International Research and Exchanges Board Records Span Dates: 1947-1991 (bulk 1956-1983) ID No: MSS80702 Creator: International Research and Exchanges Board Creator: Inter-University Committee on Travel Grants Extent: 331,000 items; 331 cartons; 397.2 linear feet Language: Collection material in English and Russian Repository: Manuscript Division, Library of Congress, Washington, D.C. Abstract: American service organization sponsoring scholarly exchange programs with the Soviet Union and Eastern Europe in the Cold War era. Correspondence, case files, subject files, reports, financial records, printed matter, and other records documenting participants’ personal experiences and research projects as well as the administrative operations, selection process, and collaborative projects of one of America’s principal academic exchange programs. International Research and Exchanges Board Records Page iii Contents Collection Summary .......................................................... ii Administrative Information ......................................................1 Organizational History..........................................................2 -

High-Impact Grantmaking: the Power of Collaboration
High-Impact Grantmaking: The Power of Collaboration Each year, NW Children’s Fund Board associated with increased poverty, Strengthening Fragile Families: Grants Members explore the latest research homelessness and mental health issues in this category seek to prevent child surrounding child welfare and prepare are key risk factors for child abuse and abuse and neglect in at-risk families, and for the upcoming grant-review cycle. This neglect. support healing and stability for families year, the Board invited 10 child welfare affected by domestic violence. experts to lend new research and In this grantmaking area, NWCF insights to the discussion. Several of prioritizes programs that provide In order to support families at greatest these experts also participated as counseling and therapy, foster care risk of child maltreatment, NWCF panelists at our annual fall retreat. The programming, adoption services, and prioritizes programs aimed at building result was an invigorating exchange of comprehensive support services. We will families’ “protective factors” (see ideas that confirmed NWCF’s strategic focus on comprehensive services aimed box on page two) – parent education approach, and sparked ideas for fine- at long-term benefits--programs that not and training, support groups for tuning our grant-making processes to fit only treat, but prevent victims of abuse caregivers, family centers, supportive the ever-evolving needs of fragile from growing up to become another housing programs, emergency shelters, children and families in our area. generation of abusers. counseling, and other support services. Here are highlights in our three grantmaking areas: Healing Abused Children: The goal of these grants is to help young victims of abuse and neglect heal from early childhood traumatic experiences and find permanency and stability in their lives. -

Aes Corporation
THE AES CORPORATION THE AES CORPORATION The global power company A Passion to Serve A Passion A PASSION to SERVE 2000 ANNUAL REPORT ANNUAL REPORT THE AES CORPORATION 1001 North 19th Street 2000 Arlington, Virginia 22209 USA (703) 522-1315 CONTENTS OFFICES 1 AES at a Glance AES CORPORATION AES HORIZONS THINK AES (CORPORATE OFFICE) Richmond, United Kingdom Arlington, Virginia 2 Note from the Chairman 1001 North 19th Street AES OASIS AES TRANSPOWER Arlington, Virginia 22209 Suite 802, 8th Floor #16-05 Six Battery Road 5 Our Annual Letter USA City Tower 2 049909 Singapore Phone: (703) 522-1315 Sheikh Zayed Road Phone: 65-533-0515 17 AES Worldwide Overview Fax: (703) 528-4510 P.O. Box 62843 Fax: 65-535-7287 AES AMERICAS Dubai, United Arab Emirates 33 AES People Arlington, Virginia Phone: 97-14-332-9699 REGISTRAR AND Fax: 97-14-332-6787 TRANSFER AGENT: 83 2000 AES Financial Review AES ANDES FIRST CHICAGO TRUST AES ORIENT Avenida del Libertador COMPANY OF NEW YORK, 26/F. Entertainment Building 602 13th Floor A DIVISION OF EQUISERVE 30 Queen’s Road Central 1001 Capital Federal P.O. Box 2500 Hong Kong Buenos Aires, Argentina Jersey City, New Jersey 07303 Phone: 852-2842-5111 Phone: 54-11-4816-1502 USA Fax: 852-2530-1673 Fax: 54-11-4816-6605 Shareholder Relations AES AURORA AES PACIFIC Phone: (800) 519-3111 100 Pine Street Arlington, Virginia STOCK LISTING: Suite 3300 NYSE Symbol: AES AES ENTERPRISE San Francisco, California 94111 Investor Relations Contact: Arlington, Virginia USA $217 $31 Kenneth R. Woodcock 93% 92% AES ELECTRIC Phone: (415) 395-7899 $1.46* 91% Senior Vice President 89% Burleigh House Fax: (415) 395-7891 88% 1001 North 19th Street $.96* 18 Parkshot $.84* AES SÃO PAULO Arlington, Virginia 22209 Richmond TW9 2RG $21 Av. -

Diplomatic List – Fall 2018
United States Department of State Diplomatic List Fall 2018 Preface This publication contains the names of the members of the diplomatic staffs of all bilateral missions and delegations (herein after “missions”) and their spouses. Members of the diplomatic staff are the members of the staff of the mission having diplomatic rank. These persons, with the exception of those identified by asterisks, enjoy full immunity under provisions of the Vienna Convention on Diplomatic Relations. Pertinent provisions of the Convention include the following: Article 29 The person of a diplomatic agent shall be inviolable. He shall not be liable to any form of arrest or detention. The receiving State shall treat him with due respect and shall take all appropriate steps to prevent any attack on his person, freedom, or dignity. Article 31 A diplomatic agent shall enjoy immunity from the criminal jurisdiction of the receiving State. He shall also enjoy immunity from its civil and administrative jurisdiction, except in the case of: (a) a real action relating to private immovable property situated in the territory of the receiving State, unless he holds it on behalf of the sending State for the purposes of the mission; (b) an action relating to succession in which the diplomatic agent is involved as an executor, administrator, heir or legatee as a private person and not on behalf of the sending State; (c) an action relating to any professional or commercial activity exercised by the diplomatic agent in the receiving State outside of his official functions. -- A diplomatic agent’s family members are entitled to the same immunities unless they are United States Nationals. -

30 Years of Turning Hope Into Action
30 Years of Turning Hope into Action NW Children’s Fund is turning 30! In fact, NWCF has provided grants to expand at key junctures in their own more than 300 agencies in Western growth. Says Mimi Siegel, Executive The dictionary defines a “generation” in Washington since its inception in 1985. Director of Kindering: human terms as 30 years. So NW Some of our 1,250+ grants have helped Children’s Fund is amazed and proud to fledgling organizations to get off the Kindering received its first NWCF grant be able to say that literally a generation ground, others have provided much- 20 years ago. … [A]s our Eastside of children, adolescents and their needed funding to expand programs and community has evolved, we have families have been touched by the services, and yet others have ensured recognized the increasing needs of programs that we have funded. These that effective established programs infants and children at risk of neglect or children and their families have grown continue to offer life-changing services abuse. NWCF has been right alongside up safer, healthier and more resilient, to children in need. Kindering and our families, enabling us thanks to the unflagging (and often to pilot several highly effective projects under-recognized) work of the When asked, NW Children’s Fund grant to address feeding issues, parent organizations we support. recipients often say that they wouldn’t education, and foster care… Each and be able to deliver critical services to every success began with a start-up their clients without our support. NWCF grant from NWCF. -
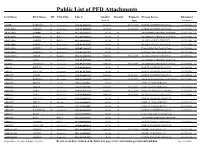
Public List of PFD Attachments
Public List of PFD Attachments Last Name First Name MI Court Site Case # Amount Reason* Payment Process Server Document Seized Date Locator # ABAIR BARBARA J Anchorage 3AN-15-07567CI $880.00 09/23/2017 NORTH COUNTRY PROCESS 2017042963 2 ABALAMA AMBER R Anchorage 3AN-10-00200SC $819.50 09/23/2017 NORTH COUNTRY PROCESS 2017011036 4 ABALAMA AMBER R Palmer 3PA-10-02623CI $0.00 B ATTORNEYS PROCESS SERVICE 2017011036 4 ABALAMA AMBER R Palmer 3PA-10-02623CI $0.00 B ATTORNEYS PROCESS SERVICE 2017011036 4 ABALAMA AMBER R Palmer 3PA-10-00783SC $0.00 B ALASKA COURT SERVICES 2017011036 4 ABALAMA SHIRELL F Anchorage 3AN-02-02749SC $0.00 B ALASKA COURT SERVICES 2017058060 0 ABALAMA SHIRELL F Anchorage 3AN-05-11010CI $0.00 B Certified Mail By Clerk Of Court 2017058060 0 ABALAMA SHIRELL F Anchorage 3AN-01-06487CI $0.00 B INQUEST PROCESS SERVICE 2017058060 0 ABALANZA JOMER T Kodiak 3KO-15-00018SC $880.00 09/23/2017 ALASKA COURT SERVICES 2017054462 8 ABANG TERA Anchorage 3AN-05-01894SC $0.00 A ATTORNEYS PROCESS SERVICE ABARO CHANELLE M Anchorage 3AN-09-02177SC $880.00 09/23/2017 ATTORNEYS PROCESS SERVICE 2017049038 9 ABBAS PHYLLIS A Anchorage 3AN-08-05753CI $0.00 B NORTH COUNTRY PROCESS 2017066584 3 ABBAS PHYLLIS A Anchorage 3AN-06-03730SC $0.00 B NORTH COUNTRY PROCESS 2017066584 3 ABBOTT ANGEL Anchorage 3AN-17-00537SC $506.04 09/23/2017 NORTH COUNTRY PROCESS 2017047984 4 ABBOTT BRENNA N Ketchikan 1KE-13-00007SC $880.00 10/20/2017 SEAK PROFESSIONAL SERVICES LLC2017012534 2 ABBOTT BRIAN L Juneau 1JU-12-00027SC $0.00 A CIVIL CLAIMS SERVICE ABBOTT CHLOE Juneau -
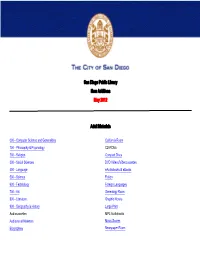
San Diego Public Library New Additions May 2012
San Diego Public Library New Additions May 2012 Adult Materials 000 - Computer Science and Generalities California Room 100 - Philosophy & Psychology CD-ROMs 200 - Religion Compact Discs 300 - Social Sciences DVD Videos/Videocassettes 400 - Language eAudiobooks & eBooks 500 - Science Fiction 600 - Technology Foreign Languages 700 - Art Genealogy Room 800 - Literature Graphic Novels 900 - Geography & History Large Print Audiocassettes MP3 Audiobooks Audiovisual Materials Music Scores Biographies Newspaper Room Fiction Call # Author Title [MYST] FIC/ADAMS Adams, Jane Night vision : a Naomi Blake novel [MYST] FIC/ALLAN Allan, Barbara. Antiques disposal [MYST] FIC/ALLINGHAM Allingham, Margery Cargo of eagles [MYST] FIC/ALLINGHAM Allingham, Margery The mind readers [MYST] FIC/ATHERTON Atherton, Nancy. Aunt Dimity and the village witch [MYST] FIC/ATKINS Atkins, Ace. Robert B. Parker's lullaby : a Spenser novel [MYST] FIC/BASS Bass, Jefferson. The inquisitor's key [MYST] FIC/BRADBURY Bradbury, Ray Death is a lonely business [MYST] FIC/CAVENDER Cavender, Chris. Rest in pizza [MYST] FIC/CLARK Clark, Marcia. Guilt by degrees : a novel [MYST] FIC/DOHERTY Doherty, P. C. The Mysterium : a Hugh Corbett medieval mystery [MYST] FIC/DRYDEN Dryden, Alex. The blind spy : a novel [MYST] FIC/EDWARDSON Edwardson, Åke Sail of stone [MYST] FIC/GOLDENBAUM Goldenbaum, Sally. A fatal fleece : a seaside knitters mystery [MYST] FIC/GRABENSTEIN Grabenstein, Chris. Fun house [MYST] FIC/GRAVES Graves, Sarah. Dead level : a home repair is homicide mystery [MYST] FIC/GREAVES Greaves, Chuck. Hush money [MYST] FIC/HARRIS Harris, Charlaine. Deadlocked [MYST] FIC/HAYS Hays, Tony. The stolen bride [MYST] FIC/JOHNSON Johnson, Craig As the crow flies [MYST] FIC/KEILLOR Keillor, Garrison. -

Tekovská Knižnica V Leviciach
Tekovská knižnica v Leviciach Prírastkové Hlavný názov Hlavný autor Cena Jazyk číslo K199595 10 malých zajačikov Edith Jentner leporelo 1.63 slo K182174 10 malých zajačikov Edith Jentner leporelo 1.63 slo H26094 100 čarodejných spôsobov, ako objaviť svoj pôvab brož. 5.61 slo K162250 1000 dobrých rad zahrádkářům Radoslav Šrot viaz. 3.98 cze H2817 101 dalmatínov Walt Disney viaz. 3.95 slo K187094 101 dalmatínov Walt Disney viaz. 2.95 slo K253156 12 obľúbených rozprávok Dvanásť viaz. 8.27 slo K142996 13 éves lány vagyok Mischa de Vreede viaz. 0.58 hun K142995 13 éves lány vagyok Mischa de Vreede viaz. 0.58 hun K9960 15 egyfelvonásos viaz. 0.48 hun K99474 222 új magyar vers viaz. 0.93 hun K187656 3. príručka mladých svišťov Walt Disney viaz. 2.29 slo H21144 365 more bedtime stories John Gatehouse viaz. 3.32 eng K170231 365 príbehov viaz. 2.95 slo K192402 366 príbehov z prírody a ešte čosi navyše Anne-Marie Dalmais viaz. 4.28 slo K171217 3x Egon Bondy Egon Bondy viaz. 0.83 cze H18274 3x Randôt Noel (vl.m.Randonski, Wigiliusz) Randonviaz. 1.99 slo K200498 4 1/2 priateľa na horúcej stope Joachim Friedrich viaz. 2.95 slo K200497 4 1/2 priateľa na horúcej stope Joachim Friedrich viaz. 2.95 slo K192447 4. príručka mladých svišťov Walt Disney viaz. 2.29 slo K180544 444 najzaujímavejších rekordov Nikolaus Lenz viaz. 2.32 slo K194819 5. príručka mladých svišťov Walt Disney viaz. 2.29 slo H6882 5000 zaujímavostí o svete okolo nás Ercole Patti viaz. 13.24 slo K199925 7. -
Bodleian Library Publishing Sprint 2021
Bodleian Library Publishing SPRING 2021 Bodleian Library Publishing SPRING 2021 Founded in 1602, the Bodleian Library is one of the oldest libraries in Britain and the largest university library in Europe. Since 1610, it has been entitled to receive a copy of every book published in the British Isles. The Bodleian collections, built up through benefaction, purchase and legal deposit, are exceptionally diverse, spanning every corner of the globe and embracing almost every form of written work and the book arts. With over thirteen million items and outstanding special collections, the Bodleian draws readers from every continent and continues to inspire generations of researchers as well as the wider public who enjoy its exhibitions, displays, public lectures and other events. Increasingly, its unique collections are available to all digitally. Bodleian Library Publishing helps to bring some of the riches of Oxford’s libraries to readers around the world through a range of beautiful and authoritative books. We publish approximately twenty-five new books a year on a wide range of subjects, including titles related to our exhibitions, illustrated and non-illustrated books, facsimiles, children’s books and stationery. We have a current backlist of over 250 titles. Cover image Illustrations from Johann Wilhelm All of our profits are returned to the Bodleian Phytanthoza Iconographia Weinmann’s , 1737–1745. and help support the Library’s work in curating, Bodleian Library, Arch.Nat. hist. G 5-12. Taken from A Cornucopia of Fruit & Vegetables, page 2. conserving and expanding its rich archives, helping to maintain the Bodleian’s position as one of the Image opposite Gallery, Upper Reading Room, Radcliffe Camera © Featherstonhaugh pre-eminent libraries in the world. -
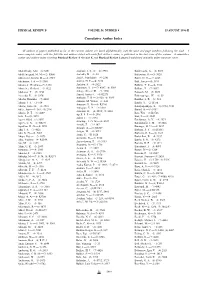
Author Index (Print)
PHYSICAL REVIEW B VOLUME 54, NUMBER 8 15 AUGUST 1996-II Cumulative Author Index All authors of papers published so far in the current volume are listed alphabetically with the issue and page numbers following the dash. A more complete index, with the full title and authors listed with each ®rst author's name, is published in the last issue of the volume. A cumulative author and subject index covering Physical Review A through E and Physical Review Letters is published annually under separate cover. Abdel-Hady, Afaf—͑6͒ 3851 Andrade, J. S., Jr.—͑6͒ 3910 Baldereschi, A.—͑8͒ 5691 Abd-Elmeguid, M. M.—͑2͒ R800 Andraka, B.—͑1͒ 48 Balestrino, G.—͑5͒ 3628 Abkemeier, Kristin M.—͑4͒ 2723 Andre´, Jean-Marie—͑4͒ 2381 Balev, O. G.—͑7͒ 4863 Abrikosov, I. A.—͑5͒ 3380 Andres, H. P.—͑6͒ 3830 Ball, James—͑5͒ 3499 Abromeit, Christian—͑5͒ 3142 Andrieu, S.—͑4͒ 2822 Ballabh, T. K.—͑6͒ 3926 Abstreiter, Gerhard—͑3͒ 1922 Anisimov, V. I.—͑7͒ 4387; ͑8͒ 5309 Ballone, P.—͑7͒ 5097 Abukawa, T.—͑7͒ 4456 Anlage, Steven M.—͑5͒ 3508 Balooch, M.—͑7͒ 5029 Acevedo, R.—͑6͒ 3976 Annett, James F.—͑4͒ R2271 Baltensperger, W.—͑1͒ 59 Anthony, T. R.—͑2͒ 920; ͑6͒ 3989 Adachi, Hirohiko—͑7͒ 4604 Bandler, S. R.—͑1͒ 534 Antisari, M. Vittori—͑1͒ 441 Adams, J. S.—͑1͒ 534 Bando, Y.—͑2͒ R756 Antonov, V. N.—͑6͒ R3706 Adams, James B.—͑4͒ 2910 Bandyopadhyay, S.—͑8͒ 5712, 5721 Antropov, V. P.—͑2͒ 1019 Adler, Joan—͑1͒ 364; ͑5͒ 2996 Bansil, A.—͑8͒ 5453 Anwand, W.—͑4͒ 2512; ͑5͒ 3084 Adroja, D. -
Program Update
We are excited to present the following program of 281 virtual sessions for this year’s Virtual 96th Annual Conference! To search for a specific name or for keywords in the program, type Ctrl-F to open a search bar. All sessions are listed in Pacific Daylight Time. Participating Allied Societies AEAMP .............. AEA Mentoring Program AEDSB ............... Association for Economic and Development Studies of Bangladesh AERE .................. Association of Environmental and Resource Economists ASHE .................. American Society of Hispanic Economists Clio .................... Cliometric Society CSMGEP ............ AEA Committee on the Status of Minority Groups in the Economics Profession CSWEP ............... AEA Committee on the Status of Women in the Economics Profession EHA ................... Economic History Association ENSA ................. Economics of National Security Association ESA .................... Economic Science Association KAEA.................. Korea-America Economic Association MEEA................. Middle East Economic Association NAFE ................. National Association of Forensic Economics SABE .................. Society for the Advancement of Behavioral Economics TPUG ................. Transportation and Public Utilities Group Featured Sessions Monday, June 28 @ 10:00 AM–11:45 AM — Presidential Address by John B. Shoven, Stanford University [079] 2020 PRESIDENTIAL ADDRESS: IS AUTOMATIC ENROLLMENT CONSISTENT WITH A LIFE CYCLE MODEL? Monday, June 28 @ 12:00 PM–1:45 PM — Professional Development [080] -

Recent References: October 1, 2005 to December 31, 2005
BNL-77290-2006-IR Recent References: October 1, 2005 to December 31, 2005 David F. Winchell National Nuclear Data Center, Brookhaven National Laboratory November 2006 Energy Sciences & Technology Department National Nuclear Data Center Brookhaven National Laboratory P.O. Box 5000 Upton, NY 11973-5000 www.bnl.gov Notice: This manuscript has been authored by employees of Brookhaven Science Associates, LLC under Contract No. DE-AC02-98CH10886 with the U.S. Department of Energy. The publisher by accepting the manuscript for publication acknowledges that the United States Government retains a non-exclusive, paid-up, irrevocable, world-wide license to publish or reproduce the published form of this manuscript, or allow others to do so, for United States Government purposes. DISCLAIMER This report was prepared as an account of work sponsored by an agency of the United States Government. Neither the United States Government nor any agency thereof, nor any of their employees, nor any of their contractors, subcontractors, or their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or any third party’s use or the results of such use of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof or its contractors or subcontractors. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government or any agency thereof.