Natural Genetic Variation Affecting Calcium Homeostasis Rebecca Anna Replogle Purdue University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
In Vivo Studies Using the Classical Mouse Diversity Panel
The Mouse Diversity Panel Predicts Clinical Drug Toxicity Risk Where Classical Models Fail Alison Harrill, Ph.D The Hamner-UNC Institute for Drug Safety Sciences 0 The Importance of Predicting Clinical Adverse Drug Reactions (ADR) Figure: Cath O’Driscoll Nature Publishing 2004 Risk ID PGx Testing 1 People Respond Differently to Drugs Pharmacogenetic Markers Identified by Genome-Wide Association Drug Adverse Drug Risk Allele Reaction (ADR) Abacavir Hypersensitivity HLA-B*5701 Flucloxacillin Hepatotoxicity Allopurinol Cutaneous ADR HLA-B*5801 Carbamazepine Stevens-Johnson HLA-B*1502 Syndrome Augmentin Hepatotoxicity DRB1*1501 Ximelagatran Hepatotoxicity DRB1*0701 Ticlopidine Hepatotoxicity HLA-A*3303 Average preclinical populations and human hepatocytes lack the diversity to detect incidence of adverse events that occur only in 1/10,000 people. Current Rodent Models of Risk Assessment The Challenge “At a time of extraordinary scientific progress, methods have hardly changed in several decades ([FDA] 2004)… Toxicologists face a major challenge in the twenty-first century. They need to embrace the new “omics” techniques and ensure that they are using the most appropriate animals if their discipline is to become a more effective tool in drug development.” -Dr. Michael Festing Quantitative geneticist Toxicol Pathol. 2010;38(5):681-90 Rodent Models as a Strategy for Hazard Characterization and Pharmacogenetics Genetically defined rodent models may provide ability to: 1. Improve preclinical prediction of drugs that carry a human safety risk 2. -

Age-Dependent Myocardial Transcriptomic Changes in the Rat
Revista Română de Medicină de Laborator Vol. 22, Nr. 1, Martie, 2014 9 Research article DOI: 10.2478/rrlm-2014-0001 Age-dependent myocardial transcriptomic changes in the rat. Novel insights into atrial and ventricular arrhythmias pathogenesis Modificări transcriptomice dependente de vârstă în miocardul de șobolan. Noi aspecte referitoare la patogeneza aritmiilor atriale și ventriculare Alina Scridon1,2, Emmanuelle Fouilloux-Meugnier3, Emmanuelle Loizon3, Marcel Perian1, Sophie Rome3, Claude Julien2, Christian Barrès2, Philippe Chevalier2,4 1.Physiology Department, University of Medicine and Pharmacy of Tîrgu Mureș, 540139, Tîrgu Mureș, Romania 2. Unité de Neurocardiologie, EA4612, Université Lyon 1, F-69008, Lyon, France 3. Unité 1060 INSERM CarMen, Université Lyon 1, F-69008, Lyon, France 4. Hospices Civils de Lyon, Hôpital Louis Pradel, Service de Rythmologie, 69500, Bron, France Abstract Background: Aging is associated with significantly increased prevalence of cardiac arrhythmias, but tran- scriptional events that underlie this process remain to be established. To gain deeper insight into molecular mech- anisms of aging-related cardiac arrhythmias, we performed mRNA expression analysis comparing atrial and ven- tricular myocardium from Wistar-Kyoto (WKY) rats of different ages. Methods: Atrial and ventricular sampling was performed in 3 groups (n=4 each) of young (14-week-old), adult (25-week-old), and aging (47-week-old) WKY rats. mRNA expressions of 89 genes involved in cardiac arrhythmogenicity were investigated using TaqMan Low Density Array analysis. Results: Of the 89 studied genes, 40 and 64 genes presented steady atrial and ventricu- lar expressions, respectively. All genes differentially expressed within the atria of WKY rats were up-regulated with advancing age, mainly the genes encoding for various K+, Ca2+, Na+ channels, and type 6 collagen. -

The Mineralocorticoid Receptor Leads to Increased Expression of EGFR
www.nature.com/scientificreports OPEN The mineralocorticoid receptor leads to increased expression of EGFR and T‑type calcium channels that support HL‑1 cell hypertrophy Katharina Stroedecke1,2, Sandra Meinel1,2, Fritz Markwardt1, Udo Kloeckner1, Nicole Straetz1, Katja Quarch1, Barbara Schreier1, Michael Kopf1, Michael Gekle1 & Claudia Grossmann1* The EGF receptor (EGFR) has been extensively studied in tumor biology and recently a role in cardiovascular pathophysiology was suggested. The mineralocorticoid receptor (MR) is an important efector of the renin–angiotensin–aldosterone‑system and elicits pathophysiological efects in the cardiovascular system; however, the underlying molecular mechanisms are unclear. Our aim was to investigate the importance of EGFR for MR‑mediated cardiovascular pathophysiology because MR is known to induce EGFR expression. We identifed a SNP within the EGFR promoter that modulates MR‑induced EGFR expression. In RNA‑sequencing and qPCR experiments in heart tissue of EGFR KO and WT mice, changes in EGFR abundance led to diferential expression of cardiac ion channels, especially of the T‑type calcium channel CACNA1H. Accordingly, CACNA1H expression was increased in WT mice after in vivo MR activation by aldosterone but not in respective EGFR KO mice. Aldosterone‑ and EGF‑responsiveness of CACNA1H expression was confrmed in HL‑1 cells by Western blot and by measuring peak current density of T‑type calcium channels. Aldosterone‑induced CACNA1H protein expression could be abrogated by the EGFR inhibitor AG1478. Furthermore, inhibition of T‑type calcium channels with mibefradil or ML218 reduced diameter, volume and BNP levels in HL‑1 cells. In conclusion the MR regulates EGFR and CACNA1H expression, which has an efect on HL‑1 cell diameter, and the extent of this regulation seems to depend on the SNP‑216 (G/T) genotype. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

To Study Mutant P53 Gain of Function, Various Tumor-Derived P53 Mutants
Differential effects of mutant TAp63γ on transactivation of p53 and/or p63 responsive genes and their effects on global gene expression. A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science By Shama K Khokhar M.Sc., Bilaspur University, 2004 B.Sc., Bhopal University, 2002 2007 1 COPYRIGHT SHAMA K KHOKHAR 2007 2 WRIGHT STATE UNIVERSITY SCHOOL OF GRADUATE STUDIES Date of Defense: 12-03-07 I HEREBY RECOMMEND THAT THE THESIS PREPARED UNDER MY SUPERVISION BY SHAMA KHAN KHOKHAR ENTITLED Differential effects of mutant TAp63γ on transactivation of p53 and/or p63 responsive genes and their effects on global gene expression BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF Master of Science Madhavi P. Kadakia, Ph.D. Thesis Director Daniel Organisciak , Ph.D. Department Chair Committee on Final Examination Madhavi P. Kadakia, Ph.D. Steven J. Berberich, Ph.D. Michael Leffak, Ph.D. Joseph F. Thomas, Jr., Ph.D. Dean, School of Graduate Studies 3 Abstract Khokhar, Shama K. M.S., Department of Biochemistry and Molecular Biology, Wright State University, 2007 Differential effect of TAp63γ mutants on transactivation of p53 and/or p63 responsive genes and their effects on global gene expression. p63, a member of the p53 gene family, known to play a role in development, has more recently also been implicated in cancer progression. Mice lacking p63 exhibit severe developmental defects such as limb truncations, abnormal skin, and absence of hair follicles, teeth, and mammary glands. Germline missense mutations of p63 have been shown to be responsible for several human developmental syndromes including SHFM, EEC and ADULT syndromes and are associated with anomalies in the development of organs of epithelial origin. -

Prox1regulates the Subtype-Specific Development of Caudal Ganglionic
The Journal of Neuroscience, September 16, 2015 • 35(37):12869–12889 • 12869 Development/Plasticity/Repair Prox1 Regulates the Subtype-Specific Development of Caudal Ganglionic Eminence-Derived GABAergic Cortical Interneurons X Goichi Miyoshi,1 Allison Young,1 Timothy Petros,1 Theofanis Karayannis,1 Melissa McKenzie Chang,1 Alfonso Lavado,2 Tomohiko Iwano,3 Miho Nakajima,4 Hiroki Taniguchi,5 Z. Josh Huang,5 XNathaniel Heintz,4 Guillermo Oliver,2 Fumio Matsuzaki,3 Robert P. Machold,1 and Gord Fishell1 1Department of Neuroscience and Physiology, NYU Neuroscience Institute, Smilow Research Center, New York University School of Medicine, New York, New York 10016, 2Department of Genetics & Tumor Cell Biology, St. Jude Children’s Research Hospital, Memphis, Tennessee 38105, 3Laboratory for Cell Asymmetry, RIKEN Center for Developmental Biology, Kobe 650-0047, Japan, 4Laboratory of Molecular Biology, Howard Hughes Medical Institute, GENSAT Project, The Rockefeller University, New York, New York 10065, and 5Cold Spring Harbor Laboratory, Cold Spring Harbor, New York 11724 Neurogliaform (RELNϩ) and bipolar (VIPϩ) GABAergic interneurons of the mammalian cerebral cortex provide critical inhibition locally within the superficial layers. While these subtypes are known to originate from the embryonic caudal ganglionic eminence (CGE), the specific genetic programs that direct their positioning, maturation, and integration into the cortical network have not been eluci- dated. Here, we report that in mice expression of the transcription factor Prox1 is selectively maintained in postmitotic CGE-derived cortical interneuron precursors and that loss of Prox1 impairs the integration of these cells into superficial layers. Moreover, Prox1 differentially regulates the postnatal maturation of each specific subtype originating from the CGE (RELN, Calb2/VIP, and VIP). -

Genome-Wide DNA Methylation Analysis of KRAS Mutant Cell Lines Ben Yi Tew1,5, Joel K
www.nature.com/scientificreports OPEN Genome-wide DNA methylation analysis of KRAS mutant cell lines Ben Yi Tew1,5, Joel K. Durand2,5, Kirsten L. Bryant2, Tikvah K. Hayes2, Sen Peng3, Nhan L. Tran4, Gerald C. Gooden1, David N. Buckley1, Channing J. Der2, Albert S. Baldwin2 ✉ & Bodour Salhia1 ✉ Oncogenic RAS mutations are associated with DNA methylation changes that alter gene expression to drive cancer. Recent studies suggest that DNA methylation changes may be stochastic in nature, while other groups propose distinct signaling pathways responsible for aberrant methylation. Better understanding of DNA methylation events associated with oncogenic KRAS expression could enhance therapeutic approaches. Here we analyzed the basal CpG methylation of 11 KRAS-mutant and dependent pancreatic cancer cell lines and observed strikingly similar methylation patterns. KRAS knockdown resulted in unique methylation changes with limited overlap between each cell line. In KRAS-mutant Pa16C pancreatic cancer cells, while KRAS knockdown resulted in over 8,000 diferentially methylated (DM) CpGs, treatment with the ERK1/2-selective inhibitor SCH772984 showed less than 40 DM CpGs, suggesting that ERK is not a broadly active driver of KRAS-associated DNA methylation. KRAS G12V overexpression in an isogenic lung model reveals >50,600 DM CpGs compared to non-transformed controls. In lung and pancreatic cells, gene ontology analyses of DM promoters show an enrichment for genes involved in diferentiation and development. Taken all together, KRAS-mediated DNA methylation are stochastic and independent of canonical downstream efector signaling. These epigenetically altered genes associated with KRAS expression could represent potential therapeutic targets in KRAS-driven cancer. Activating KRAS mutations can be found in nearly 25 percent of all cancers1. -

Isolation and Characterisation of Lymphatic Endothelial Cells From
www.nature.com/scientificreports OPEN Isolation and characterisation of lymphatic endothelial cells from lung tissues afected by lymphangioleiomyomatosis Koichi Nishino1,2*, Yasuhiro Yoshimatsu3,4, Tomoki Muramatsu5, Yasuhito Sekimoto1,2, Keiko Mitani1,2, Etsuko Kobayashi1,2, Shouichi Okamoto1,2, Hiroki Ebana1,2,6,7, Yoshinori Okada8, Masatoshi Kurihara2,6, Kenji Suzuki9, Johji Inazawa5, Kazuhisa Takahashi1, Tetsuro Watabe3 & Kuniaki Seyama1,2 Lymphangioleiomyomatosis (LAM) is a rare pulmonary disease characterised by the proliferation of smooth muscle-like cells (LAM cells), and an abundance of lymphatic vessels in LAM lesions. Studies reported that vascular endothelial growth factor-D (VEGF-D) secreted by LAM cells contributes to LAM-associated lymphangiogenesis, however, the precise mechanisms of lymphangiogenesis and characteristics of lymphatic endothelial cells (LECs) in LAM lesions have not yet been elucidated. In this study, human primary-cultured LECs were obtained both from LAM-afected lung tissues (LAM-LECs) and normal lung tissues (control LECs) using fuorescence-activated cell sorting (FACS). We found that LAM-LECs had signifcantly higher ability of proliferation and migration compared to control LECs. VEGF-D signifcantly promoted migration of LECs but not proliferation of LECs in vitro. cDNA microarray and FACS analysis revealed the expression of vascular endothelial growth factor receptor (VEGFR)-3 and integrin α9 were elevated in LAM-LECs. Inhibition of VEGFR-3 suppressed proliferation and migration of LECs, and blockade of integrin α9 reduced VEGF-D-induced migration of LECs. Our data uncovered the distinct features of LAM-associated LECs, increased proliferation and migration, which may be due to higher expression of VEGFR-3 and integrin α9. Furthermore, we also found VEGF-D/VEGFR-3 and VEGF-D/ integrin α9 signaling play an important role in LAM-associated lymphangiogenesis. -
New PDF Document
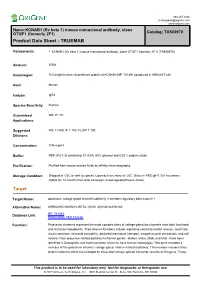
888.267.4436 [email protected] www.origene.com Name:KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) Catalog: TA503970 Product Data Sheet - TRUEMAB Components: • KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) (TA503970) Amount: 100ul Immunogen: Full length human recombinant protein of KCNAB1(NP_751891) produced in HEK293T cell. Host: Mouse Isotype: IgG1 Species Reactivity: Human Guaranteed WB, IF, FC Applications: Suggested WB 1:1000, IF 1:100, FLOW 1:100, Dilutions: Concentration: 0.96 mg/ml Buffer: PBS (PH 7.3) containing 1% BSA, 50% glycerol and 0.02% sodium azide. Purification: Purified from mouse ascites fluids by affinity chromatography Storage Condition: Shipped at -20C or with ice packs. Upon delivery store at -20C. Dilute in PBS (pH7.3) if necessary. Stable for 12 months from date of receipt. Avoid repeated freeze-thaws. Target Target Name: potassium voltage-gated channel subfamily A member regulatory beta subunit 1 Alternative Name: AKR6A3|KCNA1B|KV-BETA-1|Kvb1.3|hKvBeta3|hKvb3 Database Link: NP_751891 Entrez Gene 7881 Human Function: Potassium channels represent the most complex class of voltage-gated ion channels from both functional and structural standpoints. Their diverse functions include regulating neurotransmitter release, heart rate, insulin secretion, neuronal excitability, epithelial electrolyte transport, smooth muscle contraction, and cell volume. Four sequence-related potassium channel genes - shaker, shaw, shab, and shal - have been identified in Drosophila, and each has been shown to have human homolog(s). This gene encodes a member of the potassium channel, voltage-gated, shaker-related subfamily. This member includes three distinct isoforms which are encoded by three alternatively spliced transcript variants of this gene. -

The Chondrocyte Channelome: a Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities
Old Dominion University ODU Digital Commons Biological Sciences Theses & Dissertations Biological Sciences Summer 2017 The Chondrocyte Channelome: A Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities Anthony J. Asmar Old Dominion University, [email protected] Follow this and additional works at: https://digitalcommons.odu.edu/biology_etds Part of the Biology Commons, Molecular Biology Commons, and the Physiology Commons Recommended Citation Asmar, Anthony J.. "The Chondrocyte Channelome: A Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities" (2017). Doctor of Philosophy (PhD), Dissertation, Biological Sciences, Old Dominion University, DOI: 10.25777/pyha-7838 https://digitalcommons.odu.edu/biology_etds/19 This Dissertation is brought to you for free and open access by the Biological Sciences at ODU Digital Commons. It has been accepted for inclusion in Biological Sciences Theses & Dissertations by an authorized administrator of ODU Digital Commons. For more information, please contact [email protected]. THE CHONDROCYTE CHANNELOME: A NOVEL ION CHANNEL CANDIDATE IN THE PATHOGENESIS OF PECTUS DEFORMITIES by Anthony J. Asmar B.S. Biology May 2010, Virginia Polytechnic Institute M.S. Biology May 2013, Old Dominion University A Dissertation Submitted to the Faculty of Old Dominion University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY BIOMEDICAL SCIENCES OLD DOMINION UNIVERSITY August 2017 Approved by: Christopher Osgood (Co-Director) Michael Stacey (Co-Director) Lesley Greene (Member) Andrei Pakhomov (Member) Jing He (Member) ABSTRACT THE CHONDROCYTE CHANNELOME: A NOVEL ION CHANNEL CANDIDATE IN THE PATHOGENESIS OF PECTUS DEFORMITIES Anthony J. Asmar Old Dominion University, 2017 Co-Directors: Dr. Christopher Osgood Dr. Michael Stacey Costal cartilage is a type of rod-like hyaline cartilage connecting the ribs to the sternum. -

The First Genome-Wide View of Vitamin D Receptor Locations and Their Mechanistic Implications
ANTICANCER RESEARCH 32: 271-282 (2012) Review The First Genome-wide View of Vitamin D Receptor Locations and Their Mechanistic Implications CARSTEN CARLBERG1, SABINE SEUTER2 and SAMI HEIKKINEN1 1Department of Biosciences, University of Eastern Finland, Kuopio, Finland; 2Life Sciences Research Unit, University of Luxembourg, Luxembourg, Luxembourg Abstract. The transcription factor vitamin D receptor Physiological Impact of Vitamin D (VDR) is the nuclear sensor for the biologically most active in the Immune System metabolite of vitamin D, 1α,25-dihydroxyvitamin D3 (1α,25(OH)2D3). The physiological actions of the VDR and Vitamin D is a micronutrient which under ultraviolet (UV) its ligand are not only the well-known regulation of calcium radiation can also be produced in the skin (1). The most and phosphorus uptake and transport controlling bone abundant form of vitamin D is its liver hydroxylation product formation, but also their significant involvement in the 25-hydroxyvitamin D3 (25(OH)D3), serum concentrations of control of immune functions and of cellular growth and which indicate the vitamin D status of the human individual differentiation. For a general understanding of the (2). The biologically most active vitamin D metabolite is mechanisms of 1α,25(OH)2D3 signaling, it is essential to obtained from further hydroxylation of 25(OH)D3 in the monitor the genome-wide location of VDR in relation to kidney to 1α,25(OH)2D3 (3). Interestingly, the hydroxylation primary 1α,25(OH)2D3 target genes. Within the last months, of vitamin D can also take place in other tissues and a few of two chromatin immunoprecipitation sequencing (ChIP-Seq) them, such as keratinocytes and macrophages, have the studies using cells of the hematopoietic system, capacity for the full conversion of vitamin D to lymphoblastoids and monocytes, were published. -

Functional Regions in the 5' External Transcribed Spacer of Yeast Pre-Rrna
Downloaded from rnajournal.cshlp.org on October 3, 2021 - Published by Cold Spring Harbor Laboratory Press Functional regions in the 5' external transcribed spacer of yeast pre-rRNA Jing Chen1,2,3, Liman Zhang2, Keqiong Ye3,4* 1PTN Joint Graduate Program, School of Life Sciences, Tsinghua University, Beijing 100084, China 2National Institute of Biological Sciences, Beijing 102206, China 3Key Laboratory of RNA Biology, CAS Center for Excellence in Biomacromolecules, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China 4University of Chinese Academy of Sciences, Beijing 100049, China *Corresponding author: [email protected], Tel: +86 10 64887672 1 Downloaded from rnajournal.cshlp.org on October 3, 2021 - Published by Cold Spring Harbor Laboratory Press ABSTRACT Ribosomal subunits are assembled on a precursor rRNA that includes four spacers in addition to the mature rRNA sequences. The 5’ external transcribed spacer (5' ETS) is the most prominent one that recruits U3 snoRNA and a plethora of proteins during the early assembly of 90S small subunit pre-ribosomes. Here, we have conducted a comprehensive mutational analysis of 5' ETS by monitoring the processing and assembly of a plasmid-expressed pre-18S RNA. Remarkably, nearly half of the 5' ETS sequences, when depleted individually, are dispensable for 18S rRNA processing. The dispensable elements largely bind at the surface of 90S structure. Defective assembly of 5' ETS completely blocks the last stage of 90S formation, yet has little effect on the early assembly of 5' and central domain of 18S rRNA. Our study reveals the functional regions of 5' ETS and provides new insight into the assembly hierarchy of 90S pre-ribosomes.