Cardiac Cardiac
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cardiac Symptoms and Physical Signs 11
CHAPTER 1 1 Cardiac Symptoms and Physical Signs 1.1 Common Cardiac Symptoms Angina Typical angina presents as a chest tightness or heaviness brought on by effort and relieved by rest. The sensation starts in the retrosternal region and radi- ates across the chest. Frequently it is associated with a leaden feeling in the arms. Occasionally it may present in more unusual sites, e.g. pain in the jaw or teeth on effort, without pain in the chest. It may be confused with oesopha- geal pain, or may present as epigastric or even hypochondrial pain. The most important feature is its relationship to effort. Unilateral chest pain (sub- mammary) is not usually cardiac pain, which is generally symmetrical in distribution. Angina is typically exacerbated by heavy meals, cold weather (just breath- ing in cold air is enough) and emotional disturbances. Arguments with col- leagues or family and watching exciting television are typical precipitating factors. Stable Angina This is angina induced by effort and relieved by rest. It does not increase in frequency or severity, and is predictable in nature. It is associated with ST- segment depression on ECG. Decubitus Angina This is angina induced by lying down at night or during sleep. It may be caused by an increase in LVEDV (and hence wall stress) on lying fl at, associ- ated with dreaming or getting between cold sheets. Coronary spasm may occur in REM sleep. It may respond to a diuretic, calcium antagonist or nitrate taken in the evening. Swanton’s Cardiology, sixth edition. By R. H. Swanton and S. -

4.17-Kronzon-M-Mode-Echo.Pdf
M-Mode Echocardiography Is it still Alive? Itzhak Kronzon, MD,FASE Honoraria: Philips Classical M-mode Echocardiography M-Mode offers better time and image resolution. Sampling Rate M-Mode: 1800 / sec 2D: 30 / sec Disadvantages 1. Single Dimension (depth only) 2. Nonperpendicular orientation (always use 2D guidance). Normal MV MS M-Mode of RA & LA Myxomas Back cover of ECHOCARDIOGRAPHY Feigenbaum, 3rd edition MV Prolapse M-Mode in HOCM ASH / SAM Mid-systolic AV Closure Markers of LV Dysfunction A-C Shoulder (“B-Bump”) EPSS Feigenbaum, ECHOCARDIOGRAPHY What does the m-mode show? 1. MS 2. AI 3. Flail MV 4. Myxoma Answer: 3. Posterior Leaflet Motion in Flail MV Note that the posterior leaflet moves anteriorly in early diastole, before it moves posteriorly. ASD with Large L to R Shunt Note markedly dilated RV and “paradoxical” septal motion Dyssynchrony by M-Mode -LBBB 138msec Dyssynchrony of >130msec is associated with good CRT response (sensitivity 100%, specificity 63%) This M mode finding is not associated with increased risk of A. Coarctation B. Pulmonic Stenosis C. Subaortic Stenosis D. Aortic insufficiency Echo of pt with Endocarditis and Shock Best Rx is: 1. AVR 2. MVR 3. IABP 4. Can not tell Echo of pt with Endocarditis and Shock Answer: 1. AVR Note premature closure of MV & echogenic mass in LVOT (Ao veg. Vs. flail Ao cusp) Differential Dx of Premature MV Closure A. AR B. First Degree AV Block C. High Degree AV Block D. Blocked APC E. Atrial Flutter The most likely physical finding in this pt is 1. Absent left subclavian pulse 2. -

Cardiology-EKG Michael Bradley
Cardiology/EKG Board Review Michael J. Bradley D.O. DME/Program Director Family Medicine Residency Objectives • Review general method for EKG interpretation • Review specific points of “data gathering” and “diagnoses” on EKG • Review treatment considerations • Review clinical cases/EKG’s • Board exam considerations EKG EKG – 12 Leads • Anterior Leads - V1, V2, V3, V4 • Inferior Leads – II, III, aVF • Left Lateral Leads – I, aVL, V5, V6 • Right Leads – aVR, V1 11 Step Method for Reading EKG’s • “Data Gathering” – steps 1-4 – 1. Standardization – make sure paper and paper speed is standardized – 2. Heart Rate – 3. Intervals – PR, QT, QRS width – 4. Axis – normal vs. deviation 11 Step Method for Reading EKG’s • “Diagnoses” – 5. Rhythm – 6. Atrioventricular (AV) Block Disturbances – 7. Bundle Branch Block or Hemiblock of – 8. Preexcitation Conduction – 9. Enlargement and Hypertrophy – 10. Coronary Artery Disease – 11. Utter Confusion • The Only EKG Book You’ll Ever Need Malcolm S. Thaler, MD Heart Rate • Regular Rhythms Heart Rate • Irregular Rhythms Intervals • Measure length of PR interval, QT interval, width of P wave, QRS complex QTc • QTc = QT interval corrected for heart rate – Uses Bazett’s Formula or Fridericia’s Formula • Long QT syndrome – inherited or acquired (>75 meds); torsades de ponites/VF; syncope, seizures, sudden death Axis Rhythm • 4 Questions – 1. Are normal P waves present? – 2. Are QRS complexes narrow or wide (≤ or ≥ 0.12)? – 3. What is relationship between P waves and QRS complexes? – 4. Is rhythm regular or irregular? -

Pulmonary Arteriopathy in Patients with Mild Pulmonary Valve Abnormality Without Pulmonary Hypertension Or Intracardiac Shunt Karam Obeid1*, Subeer K
Original Scientific Article Journal of Structural Heart Disease, June 2018, Received: September 13, 2017 Volume 4, Issue 3:79-84 Accepted: September 27, 2017 Published online: June 2018 DOI: https://doi.org/10.12945/j.jshd.2018.040.18 Pulmonary Arteriopathy in Patients with Mild Pulmonary Valve Abnormality without Pulmonary Hypertension or Intracardiac Shunt Karam Obeid1*, Subeer K. Wadia, MD2, Gentian Lluri, MD, PhD2, Cherise Meyerson, MD3, Gregory A. Fishbein, MD3, Leigh C. Reardon, MD2, Jamil Aboulhosn, MD2 1 Department of Biological Sciences, Old Dominion University, Norfolk, Virginia, USA 2 Department of Internal Medicine, Ahmanson/UCLA Adult Congenital Heart Disease Center, Los Angeles, California, USA 3 Department of Pathology, Ronald Reagan/UCLA Medical Center, Los Angeles, California, USA Abstract benign course without episodes of dissection or rup- Background: The natural history of pulmonary artery ture despite 6/11 patients with PAA ≥ 5 cm. PA dilation aneurysms (PAA) without pulmonary hypertension, progresses slowly over time and does not appear to intracardiac shunt or significant pulmonary valvular cause secondary events. Echocardiography correlates disease has not been well studied. This study looks to well with magnetic resonance imaging and computed describe the outcome of a cohort of adults with PAA tomography and is useful in measuring PAA over time. without significant pulmonic regurgitation and steno- Copyright © 2018 Science International Corp. sis. Imaging modalities utilized to evaluate pulmonary artery (PA) size and valvular pathology are reviewed. Key Words Methods: Patients with PAA followed at the Ahmanson/ Pulmonary artery aneurysm • Pulmonary stenosis • UCLA Adult Congenital Heart Disease Center were in- Pulmonary hypertension • Aortic aneurysm cluded in this retrospective analysis. -

Unusual Right Ventricle Aneurysm and Dysplastic Pulmonary Valve With
CASE REPORT Unusual right ventricle aneurysm and dysplastic pulmonary valve with mitral valve hypoplasia Ozge Pamukcu, Abdullah Ozyurt, Mustafa Argun, Ali Baykan, Nazmi Narın, Kazım Uzum Erciyes University School of Medicine, Division of Pediatric Cardiology, Kayseri, Turkey ABSTRACT We report a newborn with an unusual combination of aneurysmally dilated thin‑walled right ventricle with hypertrophy of the apical muscles of the right ventricle. There was narrow pulmonary annulus, pulmonary regurgitation, and hypoplasia of the mitral valve and left ventricle. We propose that this heart represents a partial form of Uhl`s anomaly. Keywords: Absent pulmonary valve, right ventricle aneurysm, Uhl’s anomaly INTRODUCTION A pansystolic murmur was heard. The chest X‑ray showed marked cardiomegaly and a cardiothoracic ratio of 85%. Aneursymal dilatation of the right ventricle can be seen Echocardiography showed an aneurysmally dilated right in several malformations like congenital aneurysm, Uhl’s ventricle [Figure 1, Videos 1‑3]. The entire right ventricle anomaly, arrhythmogenic right ventricular dysplasia, except the apical portion was dilated. There was apical atrialized portion of the Ebstein’s anomaly, absent muscular hypertrophy of the right ventricle. [Figure 1] right pericardium, or post‑ischemic aneurysms.[1] Such The tricuspid valve was mildly hypoplastic (Z score ‑0.95) aneurysms are being increasingly diagnosed prenatally.[2] and prolapsing, but not displaced. The pulmonary valve was dysplastic and doming [Figure 2], with mild We report a case having an aneurysmatically dilated right pulmonary regurgitation [Figure 3]. Although the ventricle resembling the Uhl’s Anomaly, with an unusual pulmonary annulus was not very small, the anatomy combination of lesions. -

The Conversion to Rastelli's Type Operation from Patrick-Mcgoon's
General Thoracic and Cardiovascular Surgery (2019) 67:551–553 https://doi.org/10.1007/s11748-018-0942-x CASE REPORT The conversion to Rastelli’s type operation from Patrick-McGoon’s procedure of an adult with Taussig–Bing heart: a case report Keiichi Fujiwara1 · Kousuke Yoshizawa1 · Nobuhisa Ohno1 · Hisanori Sakazaki2 Received: 30 January 2018 / Accepted: 18 May 2018 / Published online: 11 June 2018 © The Japanese Association for Thoracic Surgery 2018 Abstract A 23-year-old female of Taussig–Bing heart with antero-posterior relation of the great arteries was underwent Patrick- McGoon’s intraventricular rerouting at 6 years old of age. The left ventricular outflow obstruction (peak pressure gradient of 100 mmHg) developed, and severe aortic valve regurgitation following bacterial endocarditis was noted. The conversion to Rastelli’s type operation and aortic valve replacement were performed successfully at 23 years old of age. She is doing well without any significant left or right ventricular outflow obstruction at 7 years postoperatively. Keywords Taussig–Bing heart · Intraventricular rerouting · Patrick-McGoon’s operation · Left ventricular outflow obstruction · Adult congenital heart disease Introduction Case Taussig–Bing heart is characterized by double-outlet right A 23-year-old female diagnosed of double outlet right ventricle with subpulmonary ventricular septal defect [1, 2]. ventricle with subpulmonary ventricular septal defect and Currently, the arterial switch procedure as anatomic repair, antero-posterior relation of the great arteries, was referred to connecting the left ventricle to aorta and the right ventricle our hospital for severe left ventricular outflow tract obstruc- to pulmonary artery, is a popular surgical management for tion following Patrick-McGoon’s intraventricular rerouting Taussig–Bing heart regardless of relation of the great arter- and moderate to severe aortic valve regurgitation following ies. -

Giant Right Atrium Or Ebstein Anomaly? Hacer Kamalı1, Abdullah Erdem1*, Cengiz Erol2 and Atıf Akçevin3
ISSN: 2378-2951 Kamalı et al. Int J Clin Cardiol 2017, 4:104 DOI: 10.23937/2378-2951/1410104 Volume 4 | Issue 4 International Journal of Open Access Clinical Cardiology CASE REPORT Giant Right Atrium or Ebstein Anomaly? Hacer Kamalı1, Abdullah Erdem1*, Cengiz Erol2 and Atıf Akçevin3 1Department of Pediatric Cardiology, Istanbul Medipol University, Turkey 2Department of Radiology, Istanbul Medipol University, Turkey 3Department of Cardiovascular Surgery, Istanbul Medipol University, Turkey *Corresponding author: Abdullah Erdem, Associate Professor of Pediatric Cardiology, Department of Pediatric Cardiology, Istanbul Medipol University, Istanbul, Turkey, Tel: +905-0577-05805, Fax: +90212467064, E-mail: drabdullaherdem@ hotmail.com partment for exercise intolerance. She had been diag- Abstract nosed and followed up as Ebstein anomaly for ten years. Many acquired and congenital pathologies could cause en- Her heart rate was 75/min with normal jugular venous largement of Right Atrium (RA). In rare pathologies we couldn’t find an obvious reason for enlargement of RA. Sometimes it pressure. Findings of lung examination were normal. leads to misdiagnosis if we try to explain an unknown pa- Auscultation of heart revealed a 2/6 systolic murmur on thology with well known pathology. In this article we de- the lower left edge of the sternum. On abdominal ex- scribe a woman who presented with giant enlargement of amination, there was no organomegaly. Arterial Oxygen the RA misdiagnosed as Ebstein anomaly. Cardiac MRI is highly helpful for differential diagnosis of these kinds of atrial Saturation (SpO2) was 98%. Electrocardiography (ECG) pathologies. Although it is rare, giant RA should be consid- revealed absence of atrial fibrillation, the rhythm was ered in differential diagnosis of huge RA without an obvious sinus but there was right axis deviation and right bundle cause. -

New Jersey Chapter American College of Physicians
NEW JERSEY CHAPTER AMERICAN COLLEGE OF PHYSICIANS ASSOCIATES ABSTRACT COMPETITION 2015 SUBMISSIONS 2015 Resident/Fellow Abstracts 1 1. ID CATEGORY NAME ADDITIONAL PROGRAM ABSTRACT AUTHORS 2. 295 Clinical Abed, Kareem Viren Vankawala MD Atlanticare Intrapulmonary Arteriovenous Malformation causing Recurrent Cerebral Emboli Vignette FACC; Qi Sun MD Regional Medical Ischemic strokes are mainly due to cardioembolic occlusion of small vessels, as well as large vessel thromboemboli. We describe a Center case of intrapulmonary A-V shunt as the etiology of an acute ischemic event. A 63 year old male with a past history of (Dominik supraventricular tachycardia and recurrent deep vein thrombosis; who has been non-compliant on Rivaroxaban, presents with Zampino) pleuritic chest pain and was found to have a right lower lobe pulmonary embolus. The deep vein thrombosis and pulmonary embolus were not significant enough to warrant ultrasound-enhanced thrombolysis by Ekosonic EndoWave Infusion Catheter System, and the patient was subsequently restarted on Rivaroxaban and discharged. The patient presented five days later with left arm tightness and was found to have multiple areas of punctuate infarction of both cerebellar hemispheres, more confluent within the right frontal lobe. Of note he was compliant at this time with Rivaroxaban. The patient was started on unfractionated heparin drip and subsequently admitted. On admission, his vital signs showed a blood pressure of 138/93, heart rate 65 bpm, and respiratory rate 16. Cardiopulmonary examination revealed regular rate and rhythm, without murmurs, rubs or gallops and his lungs were clear to auscultation. Neurologic examination revealed intact cranial nerves, preserved strength in all extremities, mild dysmetria in the left upper extremity and an NIH score of 1. -

Case Reports
Case Reports Quadrivalvular Heart Disease An Autopsied Case with Massive Pulmonary Regurgitation Tsuguya SAKAMOTO, M.D., Zen'ichiro UOZUMI, M.D., Nobuyoshi KAWAI, M.D., Yoshiyuki SAKAMOTO, M.D., Ryoko KATO, M.D., and Hideo UEDA, M.D. SUMMARY An autopsied case of quadrivalvular heart disease was described, in which pulmonary regurgitation due to possible bicuspid valve was pre- dominant and tricuspid stenosis, mitral stenosis, and aortic stenosis with insufficiency coexisted. The patient was 47, and finally 53 years old female with long-term history of cough due to bronchial compression by the enormously dilated pulmonary artery. Clinical examination revealed massive pulmonary regurgitation, which was further substantiated by right heart catheterization and cineangiocardiography. The phono- cardiograms and the reference tracings suggested the co-existence of tricuspid stenosis, aortic stenosis with regurgitation and mitral stenosis. Cardiac catheterization, intracardiac phonocardiography and angio- cardiography also favored to the diagnosis of organic tricuspid stenosis. However, the ignorance of the presence of such an unusual combination misled to the precise antemortem diagnosis. Discussion was made on the rarity of quadrivalvular heart disease, and the pathogenesis of this unusual pulmonary regurgitation was analyzed based on the autopsy finding and the history as well as the clinical mani- festation. Finally, combination of the murmurs of organic and relative tricuspid stenosis was presented to explain the acoustical findings of the present case. Additional Indexing Words: Phonocardiography Mechanocardiography Bronchial compression Right-sided Austin Flint murmur UADRIVALVULAR heart disease was first described by Shattuck1) in 1891. However, the involvement of all four valves in a given patient is extremely rare.2) The present paper describes one of such case, in which From the Second Department of Internal Medicine, Faculty of Medicine, University of Tokyo, Tokyo. -

Congenital Cardiac Surgery ICD9 to ICD10 Crosswalks Page 1 of 4 8
Congenital Cardiac Surgery ICD9 to ICD10 Crosswalks ICD-9 code ICD-9 Descriptor ICD-10 Code ICD-10 Descriptor 164.1 Malignant neoplasm of heart C38.0 Malignant neoplasm of heart 164.1 Malignant neoplasm of heart C45.2 Mesothelioma of pericardium 212.7 Benign neoplasm of heart D15.1 Benign neoplasm of heart 425.11 Hypertrophic obstructive cardiomyopathy I42.1 Obstructive hypertrophic cardiomyopathy 425.18 Other hypertrophic cardiomyopathy I42.2 Other hypertrophic cardiomyopathy 425.3 Endocardial fibroelastosis I42.4 Endocardial fibroelastosis 425.4 Other primary cardiomyopathies I42.0 Dilated cardiomyopathy 425.4 Other primary cardiomyopathies I42.5 Other restrictive cardiomyopathy 425.4 Other primary cardiomyopathies I42.8 Other cardiomyopathies 425.4 Other primary cardiomyopathies I42.9 Cardiomyopathy, unspecified 426.9 Conduction disorder, unspecified I45.9 Conduction disorder, unspecified 745.0 Common truncus Q20.0 Common arterial trunk 745.10 Complete transposition of great vessels Q20.3 Discordant ventriculoarterial connection 745.11 Double outlet right ventricle Q20.1 Double outlet right ventricle 745.12 Corrected transposition of great vessels Q20.5 Discordant atrioventricular connection 745.19 Other transposition of great vessels Q20.2 Double outlet left ventricle 745.19 Other transposition of great vessels Q20.3 Discordant ventriculoarterial connection 745.19 Other transposition of great vessels Q20.8 Other congenital malformations of cardiac chambers and connections 745.2 Tetralogy of fallot Q21.3 Tetralogy of Fallot 745.3 Common -
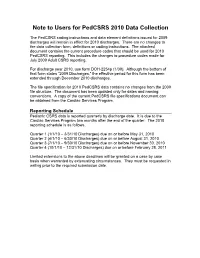
Note to Users for Pedcsrs 2010 Data Collection
Note to Users for PedCSRS 2010 Data Collection The PedCSRS coding instructions and data element definitions issued for 2009 discharges will remain in effect for 2010 discharges. There are no changes to the data collection form, definitions or coding instructions. The attached document contains the current procedure codes that should be used for 2010 PedCSRS reporting. This includes the changes to procedure codes made for July 2009 Adult CSRS reporting. For discharge year 2010, use form DOH-2254p (1/09). Although the bottom of that form states “2009 Discharges,” the effective period for this form has been extended through December 2010 discharges. The file specification for 2010 PedCSRS data contains no changes from the 2009 file structure. The document has been updated only for dates and naming conventions. A copy of the current PedCSRS file specifications document can be obtained from the Cardiac Services Program. Reporting Schedule Pediatric CSRS data is reported quarterly by discharge date. It is due to the Cardiac Services Program two months after the end of the quarter. The 2010 reporting schedule is as follows. Quarter 1 (1/1/10 – 3/31/10 Discharges) due on or before May 31, 2010 Quarter 2 (4/1/10 – 6/30/10 Discharges) due on or before August 31, 2010 Quarter 3 (7/1/10 – 9/30/10 Discharges) due on or before November 30, 2010 Quarter 4 (10/1/10 – 12/31/10 Discharges) due on or before February 28, 2011 Limited extensions to the above deadlines will be granted on a case by case basis when warranted by extenuating circumstances. -

A Human Laterality Disorder Associated with a Homozygous WDR16 Deletion
European Journal of Human Genetics (2015) 23, 1262–1265 & 2015 Macmillan Publishers Limited All rights reserved 1018-4813/15 www.nature.com/ejhg SHORT REPORT A human laterality disorder associated with a homozygous WDR16 deletion Asaf Ta-Shma*,1,3, Zeev Perles1,3, Barak Yaacov2, Marion Werner2, Ayala Frumkin2, Azaria JJT Rein1 and Orly Elpeleg2 The laterality in the embryo is determined by left-right asymmetric gene expression driven by the flow of extraembryonic fluid, which is maintained by the rotary movement of monocilia on the nodal cells. Defects manifest by abnormal formation and arrangement of visceral organs. The genetic etiology of defects not associated with primary ciliary dyskinesia is largely unknown. In this study, we investigated the cause of situs anomalies, including heterotaxy syndrome and situs inversus totalis, in a consanguineous family. Whole-exome analysis revealed a homozygous deleterious deletion in the WDR16 gene, which segregated with the phenotype. WDR16 protein was previously proposed to play a role in cilia-related signal transduction processes; the rat Wdr16 protein was shown to be confined to cilia-possessing tissues and severe hydrocephalus was observed in the wdr16 gene knockdown zebrafish. The phenotype associated with the homozygous deletion in our patients suggests a role for WDR16 in human laterality patterning. Exome analysis is a valuable tool for molecular investigation even in cases of large deletions. European Journal of Human Genetics (2015) 23, 1262–1265; doi:10.1038/ejhg.2014.265; published online 3 December 2014 INTRODUCTION and development, followed till 7 years, were normal. Her younger brother, Visceral asymmetry is determined through embryonic ciliary motion, patient II-4, was brought to medical attention at 7 weeks of age because of viral and normal function of the motile cilia plays a key role in the bronchiolitis.