Addressing Alcohol Use Practice Manual an Alcohol Screening and Brief Intervention Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 3: a Coordinated Federal Approach to Preventing and Reducing Underage Drinking
CHAPTER 3 A Coordinated Federal Approach to Preventing and Reducing Underage Drinking This document is excerpted from: The June 2015 Report to Congress on the Prevention and Reduction of Underage Drinking Chapter 3: A Coordinated Federal Approach to Preventing and Reducing Underage Drinking The 2006 STOP Act records the sense of Congress that “a multi-faceted effort is needed to more successfully address the problem of underage drinking in the United States. A coordinated approach to prevention, intervention, treatment, enforcement, and research is key to making progress. This Act recognizes the need for a focused national effort, and addresses particulars of the federal portion of that effort as well as federal support for state activities.” A Coordinated Approach The congressional mandate to develop a coordinated approach to prevent and reduce underage drinking and its adverse consequences recognizes that alcohol consumption by those under 21 is a serious, complex, and persistent societal problem with significant financial, social, and personal costs. Congress also recognizes that a long-term solution will require a broad, deep, and sustained national commitment to reducing the demand for, and access to, alcohol among young people. That solution will have to address not only the youth themselves but also the larger society that provides a context for that drinking and in which images of alcohol use are pervasive and drinking is seen as normative. The national responsibility for preventing and reducing underage drinking involves government at every level: institutions and organizations in the private sector; colleges and universities; public health and consumer groups; the alcohol and entertainment industries; schools; businesses; parents and other caregivers; other adults; and adolescents themselves. -
Brief Intervention and Motivational Interviewing Richard Ries, Md
UW PACC Psychiatry and Addictions Case Conference UW Medicine | Psychiatry and Behavioral Sciences BRIEF INTERVENTION AND MOTIVATIONAL INTERVIEWING RICHARD RIES, MD PROFESSOR AND DIRECTOR ADDICTIONS DIVISION DEPT OF PSYCHIATRY AND BEHAVIORAL SCIENCES UNIVERSITY OF WASHINGTON UW PACC ©2016 University of Washington EDUCATIONAL OBJECTIVES At the conclusion of this session, participants should be able to: Define doctor-based screening. Discuss at-risk advice. Review Motivational Interviewing. Discuss self-identification of problems and solutions. Determine how to focus on interaction. © Copyright AAAP 2016 UW PACC ©2016 University of Washington TWO MAIN MODELS: FOR BRIEF INTERVENTIONS • Doctor based-screening and at-risk advice (Fleming et al- NIAAA) – Based on standards of drinking and risk – Prescriptive – Focus on information • Psychologist based- (Miller et al) – Motivational interviewing – Self identification of problems and solutions – Focus on interaction © Copyright AAAP 2016 UW PACC ©2016 University of Washington LAST MONTH, HOW MANY AMERICANS DRANK > 5 DRINKS PER OCCASION? Binged 5 times 6 % Binged once 21% Mild use 83% 104 M people > 12 years old © Copyright AAAP 2016 UW PACC ©2016 University of Washington JAMA. 1997 Apr 2;277(13):1039-45. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. Fleming MF, Barry KL, 482 men and 292 women met inclusion criteria and were randomized into a control (n=382) or an experimental (n=392) group. A total of 723 subjects (93%) participated in the 12-month follow-up procedures. INTERVENTION: The intervention consisted of two 10- to 15-minute counseling visits delivered by physicians using a scripted workbook that included advice, education, and contracting information. -

SAFETY DATA SHEET Isopropyl Alcohol
SAFETY DATA SHEET Isopropyl Alcohol Section 1. Identification GHS product identifier : Isopropyl Alcohol Chemical name : Isopropyl alcohol Other means of : isopropanol; 2-Propanol identification Product type : Liquid. Product use : Synthetic/Analytical chemistry. Synonym : isopropanol; 2-Propanol SDS # : 001105 Supplier's details : Airgas USA, LLC and its affiliates 259 North Radnor-Chester Road Suite 100 Radnor, PA 19087-5283 1-610-687-5253 24-hour telephone : 1-866-734-3438 Section 2. Hazards identification OSHA/HCS status : This material is considered hazardous by the OSHA Hazard Communication Standard (29 CFR 1910.1200). Classification of the : FLAMMABLE LIQUIDS - Category 2 substance or mixture EYE IRRITATION - Category 2A SPECIFIC TARGET ORGAN TOXICITY (SINGLE EXPOSURE) (Narcotic effects) - Category 3 GHS label elements Hazard pictograms : Signal word : Danger Hazard statements : May form explosive mixtures with air. Highly flammable liquid and vapor. Causes serious eye irritation. May cause drowsiness or dizziness. Precautionary statements General : Read label before use. Keep out of reach of children. If medical advice is needed, have product container or label at hand. Prevention : Wear protective gloves. Wear eye or face protection. Keep away from heat, hot surfaces, sparks, open flames and other ignition sources. No smoking. Use explosion- proof electrical, ventilating, lighting and all material-handling equipment. Use only non- sparking tools. Take precautionary measures against static discharge. Keep container tightly closed. Use only outdoors or in a well-ventilated area. Avoid breathing vapor. Wash hands thoroughly after handling. Response : IF INHALED: Remove person to fresh air and keep comfortable for breathing. Call a POISON CENTER or physician if you feel unwell. -

Teen Intervene Manual File
Brief Intervention for Adolescent Alcohol and Drug Use Manual Ken Winters, Ph.D., Andria Botzet, M.A., Tamara Fahnhorst M.P.H., & Willa Leitten, M.A. Center for Adolescent Substance Abuse Research University of Minnesota, 2006 1 Table of Contents I. User Information and Development of Brief Intervention…….. 3 II. Adolescent Therapy Session One………………………………… 19 III. Adolescent Therapy Session Two………………………………… 43 IV. Parent or Guardian Therapy Session……………………………... 53 V. References…………………………………………………………….. 70 VI. Appendix A (Substance-Specific Information)…………………… 73 VII. Appendix B (Supplemental Resources)…………………………… 151 VII. Appendix C (Copy-ready Worksheets) …………………………… 198 All materials in this manual, with the exception of resources included in the appendices, are not reproducible without permission from the author. 2 SECTION I USER INFORMATION & DEVELOPMENT OF BRIEF INTERVENTION 3 Brief Cognitive-Behavioral Intervention Overview # of BCBI Module Sessions Primary Treatment Objectives Rational-Emotive 1 1. Identify activating events for drug use Curriculum a. attending a party where most adolescents use alcohol b. using alcohol or drugs to cope with negative emotions 2. Examine irrational beliefs underlying pros and cons to activating events a. all adolescents use drugs (false perception) b. fun parties always involve drugs (false perception) 3. Develop list of alternate beliefs that promote abstinence a. many adolescents have fun at parties without using drugs b. activities can be rewarding without having alcohol/drug involvement Problem Solving 1 1. Discuss rationale for problem-solving skill development Curriculum 2. Define problem-solving components 3. Apply problem-solving process to develop risk reduction coping skills to: a. identify high-risk situations b. resist peer pressure and handle negative emotions c. -

Alcohol Use Disorder
Section: A B C D E Resources References Alcohol Use Disorder (AUD) Tool This tool is designed to support primary care providers (family physicians and primary care nurse practitioners) in screening, diagnosing and implementing pharmacotherapy treatments for adult patients (>18 years) with Alcohol Use Disorder (AUD). Primary care providers should routinely offer medication for moderate and severe AUD. Pharmacotherapy alone to treat AUD is better than no therapy at all.1 Pharmacotherapy is most effective when combined with non-pharmacotherapy, including behavioural therapy, community reinforcement, motivational enhancement, counselling and/or support groups. 2,3 TABLE OF CONTENTS pg. 1 Section A: Screening for AUD pg. 7 Section D: Non-Pharmacotherapy Options pg. 4 Section B: Diagnosing AUD pg. 8 Section E: Alcohol Withdrawal pg. 5 Section C: Pharmacotherapy Options pg. 9 Resources SECTION A: Screening for AUD All patients should be screened routinely (e.g. annually or when indicators are observed) with a recommended tool like the AUDIT. 2,3 It is important to screen all patients and not just patients eliciting an index of suspicion for AUD, since most persons with AUD are not recognized. 4 Consider screening for AUD when any of the following indicators are observed: • After a recent motor vehicle accident • High blood pressure • Liver disease • Frequent work avoidance (off work slips) • Cardiac arrhythmia • Chronic pain • Rosacea • Insomnia • Social problems • Rhinophyma • Exacerbation of sleep apnea • Legal problems Special Patient Populations A few studies have reviewed AUD in specific patient populations, including youth, older adults and pregnant or breastfeeding patients. The AUDIT screening tool considered these populations in determining the sensitivity of the tool. -

Prevention of Alcohol Abuse and Illicit Drug Use Annual Awareness and Prevention Program Notice to System Offices Employees
Prevention of Alcohol Abuse and Illicit Drug Use Annual Awareness and Prevention Program Notice to System Offices Employees Alcohol abuse and illicit drug use disrupt the work and learning environment and create an unsafe and unhealthy workplace. To protect its employees and students and fully serve the citizens of Texas, The Texas A&M University System prohibits alcohol abuse and illicit drug use. This brochure, which is distributed annually, serves as an awareness and prevention tool for System Offices employees by providing basic information about A&M System policy and regulations, legal sanctions and health risks related to alcohol abuse and illicit drug use. Information about counseling, treatment and rehabilitation programs is included. As an employee of The Texas A&M University System, motivation. Drug use by a pregnant woman may cause you must abide by state and federal laws on controlled additional health complications in her unborn child. substances, illicit drugs and use of alcohol. In addition, you must comply with A&M System policy, which states: A&M System Sanctions The Texas A&M University System (system) strictly The A&M System’s drug and alcohol abuse policy and prohibits the unlawful manufacture, distribution, regulation are included in the System Orientation course possession or use of illicit drugs or alcohol on reviewed by new employees as part of their orientation. system property, and/or while on official duty and/or The policy and regulation are posted online at as part of any system activities. http://policies.tamus.edu/34-02.pdf and http://policies.tamus.edu/34-02-01.pdf. -

Alcohol Abuse and Acute Lung Injury and Acute Respiratory Distress
Journal of Anesthesia & Critical Care: Open Access Review Article Open Access Alcohol abuse and acute lung injury and acute respiratory distress syndrome Introduction Volume 10 Issue 6 - 2018 Alcohol is one of the most commonly used and abused beverage Fadhil Kadhum Zwer Aliqa worldwide. Alcohol is known to have numerous systemic health Private clinic practice, Iraq effects, including on the liver and central nervous system. From a respiratory standpoint, alcohol abuse has long been associated with Correspondence: Fadhil Kadhum Zwer Aliqaby, Private clinic practice, Iraq, Email an increased risk of pneumonia. More recently, alcohol abuse has been strongly linked in epidemiologic studies to development of Received: December 11, 2017 | Published: November 28, ARDS in at-risk patients. The first demonstration of an association 2018 between chronic alcohol abuse and ARDS was made by Moss et al, who retrospectively examined 351 patients at risk for ARDS.1 In this subsequent decreased phagocytosis and bacterial killing. Chronic cohort, 43% of patients who chronically abused alcohol developed alcohol use is similarly associated with altered neutrophil function and ARDS compared to only 22% of those who did not abuse alcohol, decreased superoxide production. Interestingly, chronic alcohol use with the effect most pronounced in patients with sepsis. This study decreases levels of granulocyte/macrophage colony stimulating factor was limited by its retrospective design, particularly since this design (GM-CSF) receptor and signaling in lung epithelium, which has been required that alcohol use history be obtained by chart review and shown to result in defective alveolar macrophage maturation. The documented history; furthermore, this study did not adjust for net effect of these abnormalities is an increased pulmonary bacterial concomitant cigarette smoking. -

Pennsylvania Drug and Alcohol Abuse Control Act."
§ 1690.101. Short title This act shall be known and may be cited as the "Pennsylvania Drug and Alcohol Abuse Control Act." § 1690.102. Definitions (a) The definitions contained and used in the Controlled Substance, Drug, Device and Cosmetic Act shall also apply for the purposes of this act. (b) As used in this act: "CONTROLLED SUBSTANCE" means a drug, substance, or immediate precursor in Schedules I through V of the Controlled Substance, Drug, Device and Cosmetic Act. "COUNCIL" means the Pennsylvania Advisory Council on Drug and Alcohol Abuse established by this act. "COURT" means all courts of the Commonwealth of Pennsylvania, including magistrates and justices of the peace. "DEPARTMENT." The Department of Health. "DRUG" means (i) substances recognized in the official United States Pharmacopeia, or official National Formulary, or any supplement to either of them; and (ii) substances intended for use in the diagnosis, cure, mitigation, treatment or prevention of disease in man or other animals; and (iii) substances (other than food) intended to affect the structure or any function of the body of man or other animals; and (iv) substances intended for use as a component of any article specified in clause (i), (ii) or (iii), but not including devices or their components, parts or accessories. "DRUG ABUSER" means any person who uses any controlled substance under circumstances that constitute a violation of the law. "DRUG DEPENDENT PERSON" means a person who is using a drug, controlled substance or alcohol, and who is in a state of psychic or physical dependence, or both, arising from administration of that drug, controlled substance or alcohol on a continuing basis. -

N-BUTYL ALCOHOL
Right to Know Hazardous Substance Fact Sheet Common Name: n-BUTYL ALCOHOL Synonyms: Propyl Carbinol; n-Butanol CAS Number: 71-36-3 Chemical Name: 1-Butanol RTK Substance Number: 1330 Date: November 1998 Revision: January 2008 DOT Number: UN 1120 Description and Use EMERGENCY RESPONDERS >>>> SEE BACK PAGE n-Butyl Alcohol is a colorless liquid with a strong, sweet Hazard Summary alcohol odor. It is used as a solvent for fats, waxes, shellacs, Hazard Rating NJDOH NFPA resins, gums, and varnish, in making hydraulic fluids, and in HEALTH - 2 medications for animals. FLAMMABILITY - 3 REACTIVITY - 0 f ODOR THRESHOLD = 1 to 15 ppm FLAMMABLE f Odor thresholds vary greatly. Do not rely on odor alone to POISONOUS GASES ARE PRODUCED IN FIRE determine potentially hazardous exposures. CONTAINERS MAY EXPLODE IN FIRE Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; Reasons for Citation 4=severe f n-Butyl Alcohol is on the Right to Know Hazardous f n-Butyl Alcohol can affect you when inhaled and by Substance List because it is cited by OSHA, ACGIH, DOT, passing through the skin. NIOSH, DEP, IRIS, NFPA and EPA. f Contact can irritate and burn the skin. f This chemical is on the Special Health Hazard Substance f n-Butyl Alcohol can irritate and burn the eyes with possible List. eye damage. f Inhaling n-Butyl Alcohol can irritate the nose, throat and lungs. f Exposure to n-Butyl Alcohol can cause headache, dizziness, nausea and vomiting. SEE GLOSSARY ON PAGE 5. f n-Butyl Alcohol can damage the liver, kidneys, hearing, and sense of balance. -

6.14 Alcohol Use Disorders and Alcoholic Liver Disease
6. Priority diseases and reasons for inclusion 6.14 Alcohol use disorders and alcoholic liver disease See Background Paper 6.14 (BP6_14Alcohol.pdf) Background The WHO estimates that alcohol is now the third highest risk factor for premature mortality, disability and loss of health worldwide.1 Between 2004 to 2006, alcohol use accounted for about 3.8% of all deaths (2.5 million) and about 4.5% (69.4 million) of Disability Adjusted Life Years (DALYS).2 Europe is the largest consumer of alcohol in the world and alcohol consumption in this region emerges as the third leading risk factor for disease and mortality.3 In European countries in 2004, an estimated one in seven male deaths (95 000) and one in 13 female deaths (over 25 000) in the 15 to 64 age group were due to alcohol-related causes.3 Alcohol is a causal factor in 60 types of diseases and injuries and a contributing factor in 200 others, and accounts for 20% to 50% of the prevalence of cirrhosis of the liver. Alcohol Use Disorders (AUD) account for a major part of neuropsychiatric disorders and contribute substantially to the global burden of disease. Alcohol dependence accounts for 71% of all alcohol-related deaths and for about 60% of social costs attributable to alcohol.4 The acute effects of alcohol consumption on the risk of both unintentional and intentional injuries also have a sizeable impact on the global burden of disease.2 Alcoholic liver disease (ALD) is the commonest cause of cirrhosis in the western world, and is currently one of the ten most common causes of death.5 Liver fibrosis caused by alcohol abuse and its end stage, cirrhosis, present enormous problems for health care worldwide. -

Consultation-Referral Among Physicians: Practice and Process
Consultation-Referral Among Physicians: Practice and Process T. C. Saunders, MD Calgary, Alberta Consultation-referral is a part of everyday family practice. Al though the process is taken for granted, it is a complex phenomenon. Neither the practice nor the process always meet the expectations of the referring physician or the consul tant, and the patient may be the worse because of this discrep- any. Studies of the practice and the process support this view. A model of the process is elaborated which can be used for the teaching of medical students or residents and which the prac ticing physician may use to improve his/her consultation- referral practices. The words “consultation” and “referral” re communication—the practice and process of con flect the complexity of medical practice and imply sultation and referral between physicians—and that a physician cannot be all things to his/her pa will propose a model for the teaching of both. tients and community. Fifty years ago a physician The term “referral” is usually used to denote may have been able to fulfill such a role, depend the practice whereby one physician gives over the ing upon the physician’s degree of isolation, skill, care of a patient to another physician who has and knowledge. Nowadays, communication particular expertise, knowledge, or use of a facil technology and the availability of air travel make ity. The term “consultation” usually denotes the possible startling examples of compression of time practice whereby one physician consults with and distance. For example, a man suffering chest another about a patient with the implication that pain while working on a drilling crew in the Cana the first physician will continue to care for the dian Arctic, having the benefit of a paramedic who patient during and after the consultation. -
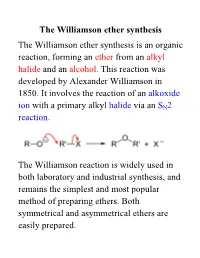
Williamson Ether Synthesis the Williamson Ether Synthesis Is an Organic Reaction, Forming an Ether from an Alkyl Halide and an Alcohol
The Williamson ether synthesis The Williamson ether synthesis is an organic reaction, forming an ether from an alkyl halide and an alcohol. This reaction was developed by Alexander Williamson in 1850. It involves the reaction of an alkoxide ion with a primary alkyl halide via an SN2 reaction. The Williamson reaction is widely used in both laboratory and industrial synthesis, and remains the simplest and most popular method of preparing ethers. Both symmetrical and asymmetrical ethers are easily prepared. The reaction for this week: an example of a Williamson ether synthesis acetaminophen ethyl iodide phenacetin starting material reagent product Phenacetin may be synthesized as an example of the Williamson ether synthesis The first synthesis of phenacetin was reported in 1878 by Harmon Morse. Procedure 1. Weigh an Extra-Strength Tylenol tablet. Pulverize the tablet with mortar and pestle. Weigh out 0.22 g and place it in a dry 15-ml round-bottom flask along with 0.28 g of finely pulverized K2CO3 (mortar and pestle) and 3.0 mL of butanone. Carefully add 0.28 mL of ethyl iodide with a syringe. 2. Add a stir bar; attach a microscale water-cooled condenser to the flask. Heat the mixture under reflux directly on a hot plate at medium setting for 1 hour. In the meantime, obtain the IR of acetaminophen. 3. Turn off the heat. Allow the mixture to cool down. Add 4 mL of water to the flask and transfer its contents to a 16 x 125 mm test tube with a screw cap. Rinse round-bottom flask 4 times with 1 mL of tert-butyl methyl ether (BME) and add the rinsings to the test tube.