Research Project Directory Spring 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SAL Farooqiq7 PD 3-Col
State of the art lecture Primary care: the custodian of diabetes care? Azhar Farooqi Abstract General Practitioner and Honorary Professor, Type 2 diabetes is the disease of our times. With some 3 million cases in the UK, primary care University of Leicester, East Leicester Medical Practice, has a vital role in coordinating and delivering evidence-based care which includes the Leicester, UK prevention, detection and management of diabetes. However, primary care has not always been able to deliver such a role; up to the end of the 1980s, despite the drawbacks of busy hospital outpatient clinics, primary care could rarely Correspondence to: offer the systematic care and skills that people with diabetes require. Professor Azhar Farooqi OBE, East Leicester Medical Quality improvement and audit in the 1990s heralded the increased adoption of Practice, 131 Uppingham Rd, Leicester LE5 4BP, UK; email: [email protected] evidence-based practice in primary care. Many GP practices significantly improved the organisation and quality of care for diabetes as a result. The widespread adoption of IT Received: 30 July 2012 systems and the emergence of a more robust evidence base for care (for example, UKPDS) Accepted: 1 August 2012 accelerated this process. More lately, investment in general practice through the Quality and Outcomes Framework This paper was presented as the 2012 Mary and practice education programmes have helped deliver significant improvements in the Mackinnon lecture at the 2012 Diabetes UK Annual quality of primary care diabetes. Professional Conference held in Glasgow However, there is still much to do, with variation in care and health inequalities persisting. -
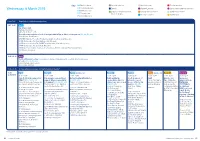
To View the Programme at a Glance
Key BS Basic science Awards sessions Masterclasses Poster sessions Wednesday, 6 March 2019 CC Community care Breaks Named Lectures Sponsored symposia sessions CS Clinical science Diabetes UK professional Oral abstract sessions Symposia sessions PC Primary care interest groups Plenary sessions Workshops SC Specialist care From 7.45 Registration, exhibition and posters 8.45 –10.25 Hall 1 Opening plenary 8.45 Opening words Chris Askew, Diabetes UK Prevention and remission at scale: Paradigm shifts in Type 2 diabetes management (CC, CS, PC, SC) Chair: George Alberti, London 8.55 NHS Diabetes Prevention Programme update Jonathan Valabhji, London 9.10 Patient perspective Harry Matharu, High Wycombe 9.25 Diabetes remission: The DiRECT way Roy Taylor, Newcastle upon Tyne 9.40 Patient perspective David Paul, Warenford 9.55 Diabetes prevention: Can mass treatment be part of the strategy? Paul Aveyard, Oxford 10.10 Panel discussion 10.25 –11.05 Hall 1 Banting Memorial Lecture: The ongoing challenge of hypoglycaemia, a century after the discovery of insulin (CC, CS, PC, SC) Chair: Stephanie Amiel, London Simon Heller, Sheffield 11.05 –11.35 Coffee, exhibition, posters and Demonstration Theatre* 11.35 – Hall 1 Room 11 Hall 2L (Exhibition Hall) Room 3A Room 4 Arena (Exhibition Hall) Room 3B Room 12 12.35/13.05 11.35 –13.05 11.35 –13.05 11.35 –13.05 11.35 –12.35 11.35 –12.35 11.35 –13.05 11.35 –12.35 11.35 –12.35 Diabetic Medicine symposium: Psychological and emotional Enteral feeding with diabetes Reintegrating the Practical aspects of Audit Exercise -

2018 Annual Report & Financial Statements(PDF
Our story Annual report and accounts 2018 Contents Foreword 4 Our vision, mission and values 6 Our strategy 8 Our year in numbers 10 Strategic report: Knowledge is power 12 Getting together, giving support 16 Research changing lives 20 Raising standards in care 24 Preventing Type 2 diabetes 28 Making life easier 32 The fight for Flash 36 Making it happen: partnerships 40 Making it happen: volunteers 44 Making it happen: fundraisers 48 Thank you 54 Future plans 56 Get involved 58 Get support 60 Our finances and how we are run 62 Independent auditor’s report 85 Financial statements 2018 90 Foreword As we reflect on a year of huge achievement for people living with and Our own fundraising events like Swim22 and the One Million Step Challenge at risk of diabetes, a simple but important truth is powerfully clear: grew significantly in 2018, while the growth in our partnership and philanthropy together we achieve more. It’s an idea that shines through our story of fundraising has played an important part too. As always, we are indebted to 2018 time and again. every single person who has supported our work. Thank you. We’re proud to have worked alongside people with diabetes, healthcare While we reflect on our successes in 2018, we cannot shy away from how the professionals and NHS leaders, and to have joined forces with the business changing world around us affects the way we provide the support, information community and other charities. Our world-class researchers, life-changing and research that people need. At the time of writing, we continue to demand campaigners and fundraisers make it all possible and, vitally, our work that the government ensures the vital needs of people with diabetes are met continues to be inspired by people whose lives have been affected by when we leave the European Union. -

Diabetes in Old Age THIRD EDITION
Diabetes in Old Age THIRD EDITION Diabetes in Old Age Third Edition Edited by Alan J. Sinclair © 2009 John Wiley & Sons Ltd. ISBN: 978-0-470-06562-4 Other titles in the Wiley Diabetes in Practice Series Exercise and Sport in Diabetes Second Edition Edited by Dinesh Nagi 978 0470 022061 Complementary Therapies and the Management of Diabetes and Vascular Disease Edited by Patricia Dunning 978 0470 014585 Diabetes in Clinical Practice: Questions and Answers from Case Studies Edited by N. Katsilambros, E. Diakoumopoulou, I. Ioannidis, S. Liatis, K. Makrilakis, N. Tentolouris and P. Tsapogas 978 0470 035221 Obesity and Diabetes Second Edition Edited by Anthony Barnett and Sudhesh Kumar 9780 0470 848982 Prevention of Type 2 Diabetes Edited by Manfred Ganz 978 0470 857335 Diabetes – Chronic Complications Second Edition Edited by Kenneth Shaw and Michael Cummings 978 0470 865798 The Metabolic Syndrome Edited by Christopher Byrne and Sarah Wild 978 0470 025116 Psychology in Diabetes Care Second Edition Edited by Frank J. Snoek and T. Chas Skinner 978 0470 015049 The Foot in Diabetes Fourth Edition Edited by Andrew J. M. Boulton, Peter R. Cavanagh and Gerry Rayman 978 0470 015049 Gastrointestinal Function in Diabetes Mellitus Edited by Michael Horowitz and Melvin Samson 978 0471 899167 Diabetic Nephropathy Edited by Christopher Hasslacher 978 0471 589924 Nutritional Management of Diabetis Mellitus Edited by Gary Frost, Anne Dornhorst and David R. Hadden 978 0471 962045 Hypoglycaemia in Clinical Diabetes Second Edition Edited by Brian M. Frier and Miles Fisher 978 0470 018446 Diabetic Cardiology Edited by Miles Fisher and John McMurray 978 0470 862049 Diabetes in Old Age THIRD EDITION Editor Alan J. -

Diabetes UK Annual Report and Accounts 2019
our story Annual report and accounts 2019 Contents Foreword 4 Our vision, our values, our mission 6 Our strategy 8 Our year in numbers 10 Strategic report: Shining a light on mental health 12 The remission revolution 16 Life-changing advances in research 20 Reducing the risk of type 2 24 Support at every step 28 The best care for everyone 32 Partners in our vision 36 Thank you 40 Our future plans 46 Get involved 50 Get support 52 Our finances and how we’re run 54 Independent auditor’s report 78 Financial statements 2019 82 Contents Foreword Welcome to our Annual Report 2019, in which we are proud to share all that we achieved last year, and introduce you to a few of the people for whom our work made a difference. Thank you to everyone – each individual supporter, community group, philanthropic organisation and business – who has supported us to achieve so much for so many in the past 12 months. At the time of writing this introduction, we are in the midst of the coronavirus (Covid-19) pandemic. As a charity, we are meeting unprecedented levels of demand upon our services, by many thousands of people living with or near diabetes who are understandably concerned or worried or who are seeking guidance and support. At the same time as meeting the calls upon us, we are steering the charity through the impacts of loss of income and of severe disruption to our work, whilst ensuring that all our staff are supported to do their work and to look after their own health and that of their loved ones. -

Wednesday, 14 March 2018
Key BS Basic science Awards sessions Oral abstract sessions Sponsored symposia sessions Wednesday, 14 March 2018 CS Clinical science Diabetes UK professional Plenary sessions Symposia sessions PC Primary care interest groups Poster sessions Workshops SC Secondary care Named lectures Breaks From 7.45 Registration, exhibition and posters 8.45 –10.25 ICC Auditorium Opening plenary 8.45 Opening words Chris Askew, Diabetes UK Cardiovascular risk reduction in diabetes: Maximising patient benefits (CS, PC, SC) Chair: Naveed Sattar, Glasgow 8.55 Epidemiology: The burden of cardiovascular disease in people with diabetes – Martin Rutter, Manchester 9.13 New clinical trials: The promise of added benefit – David Preiss, Oxford 9.31 Making cardiovascular disease risk reduction happen in primary care – Tony Willis, London 9.49 A patients perspective on cardiovascular disease risk reduction in diabetes – David Garrell, Dundee 10.07 Open discussion 10.25 –10.55 ICC Auditorium Plenary session with Simon Stevens Chair: Chris Askew, Diabetes UK Simon Stevens, NHS England 10.55 –11.35 Coffee, exhibition and posters 11.35 – ICC Auditorium Rooms 8–11 Rooms 7 and 12 Rooms 3 and 4 Arena (Exhibition Hall) Room 14 Room 17 Rooms 15 and 16 12.35/13.05 11.35–13.05 11.35–13.05 11.35–12.35 11.35–12.35 11.35–12.35 11.35–13.05 11.35–13.05 11.35–12.35 Diabetes UK’s evidence based Inpatient care and the National The REPOSE trial Diabetes and cancer Weaving psychological Population health Workshop: Sponsored nutrition guidelines for the Diabetes Inpatient Audit (NaDIA) of insulin pump therapy (CS, SC) principles into routine (CS) Hypoglycaemia: symposia: prevention and management (CS, SC) vs. -

PROJECT DIRECTORY 2016 –17 RESEARCH SPOTLIGHTS INTRODUCTION 03 Welcome to Diabetes UK’S 2016–2017 MIKE’S STORY Research Directory
PROJECT DIRECTORY 2016 –17 RESEARCH SPOTLIGHTS INTRODUCTION 03 Welcome to Diabetes UK’s 2016–2017 MIKE’S STORY Research Directory. We’re delighted to 04 share with you the innovative studies we’re supporting across the UK. Each ADOPT A PROJECT 05 one is only possible thanks to the continued support of our members, 06 EASTERN donors and Diabetes UK groups. Everything we know about managing and treating diabetes LONDON is as a result of research. Diabetes UK awarded its first 07 research grant in 1935 and the impact of the research we’ve MIDLANDS funded over the last 85 years on people’s lives is immense. 15 For example, the first ever insulin pen, ‘Penject’, was released in 1983, designed by researchers in Glasgow and NORTH WEST 16 tested in a Diabetes UK trial involving 76 people with Type 1 diabetes. It replaced the traditional syringe and NORTHERN & YORKSHIRE influenced the pens that came after. Thanks to early 18 Diabetes UK funding, the insulin pen became an important NORTHERN IRELAND tool for people with Type 1 and Type 2 diabetes all over 21 the world. SCOTLAND We’re now the largest charitable funder of diabetes research 24 in the UK. The pioneering work we fund covers all forms of diabetes and related complications. Through research, we SOUTH EAST 28 can support the ideas and people that will transform the treatment and prevention of diabetes, and lead us to a cure. SOUTH WEST 32 Every year we spend around £7 million on new and ongoing diabetes research. In 2015 alone we committed to invest in WALES 33 new projects supporting established researchers and 25 leaders of the future. -
Research Project Directory Spring 2018
Research project directory Spring 2018 Our research 2018 1 Introduction Welcome to Diabetes UK’s directory of research projects for Spring 2018. I’m delighted to share with you the innovative research we’re supporting across the UK. Each project is only In 2017 alone, we supported 37 new projects possible thanks to the and committed around £7 million to world-leading continued support of our diabetes research. I hope that you enjoy reading members, donors and about the research we fund, and you might Diabetes UK groups. consider helping us fund more research in We’ve been funding the future. research for over 80 years, You can support research projects that interest awarding our first ever you through our Adopt a Project scheme (page 5). grant in 1935. Since then, To find out more about each project, go to we’ve seen some incredible steps forward in diabetes.org.uk/research. diabetes care: the insulin pen, glucose meters, I’d like to take this opportunity to personally thank islet transplants. The researchers behind these all of our current supporters. Without your donations, discoveries have all had our support. we wouldn’t be able to achieve what we do. We’re the largest charitable funder of diabetes Please get in touch with us at research in the UK. The pioneering work we fund [email protected] if you have any today covers all forms of diabetes and related questions, comments or suggestions about complications. Everything we know about our research. managing and treating diabetes is thanks to research. And through this, we want to reach a world where diabetes can do no harm. -

Conference Program
AASD 2020 16TH INTERNATIONAL CONFERENCE OF ARABIC ASSOCIATION FOR THE STUDY OF DIABETES AND METABOLISM الجمعية العربية لدراسة أمراض السكر والميتابوليزم MEMBER OF INTERNATIONAL DIABETES FEDERATION, IDF 28 – 31 OCTOBER, 2020, EGYPT VIRTUAL MEETING Guest of Honor Prof Andrew JM Boulton IDF President AASD & Conference Honorary President Prof Raafat Rashwan AASD & Conference President Prof Inass Shaltout AASD & Conference Vice-President Prof Amr Abdel Wahab Conference Vice-President Prof Mohamed Hassanein Conference is accredited with 20 hours By (CEMTA) 1 AASD 2020 Guest of Honor IDF President Prof Andrew JM Boulton AASD & Conference Honorary President Prof Raafat Rashwan AASD & Conference President Prof Inass Shaltout AASD & Conference Vice-President Prof Amr Abdel Wahab Conference Vice-President Prof Mohamed Hassanein 2 Conference & AASD Secretary Prof Omar El-Saadany Prof Abdel Khalek Hamed Prof Hazem El Ashmawy Scientific Committee Chairmen Prof Amr Elmeligi Prof Ashraf Attia Prof Atef Elbahry Prof Mohamed Naguieb Prof Shereen Abdel Ghaffar Prof Yasser Abdel Hamid Dr Nader Wadie Scientific Committee Moderators AASD Treasure Dr Mazen Attia Dr Hisham Habib Dr. Sayed Gad 3 16TH International Conference of Arabic Association for the Study of Diabetes and Metabolism (AASD) Member of International Diabetes Federation, IDF Dear professors and colleagues, It gives us a great pleasure to welcome you in 16th annual virtual AASD conference. On behalf of AASD board and members, we appreciate the strong participation and support of International Diabetes Federation, IDF. AASD as a member of IDF puts a great responsibility on all AASD members to do extra efforts for the cause of Diabetes. Let me express our gratitude to prof Andrew Boulton, president of the International Diabetes Federation and guest of honor of AASD conference 2020 for his extraordinary support of all AASD activities.