The Influence of Movement Profile on the Female Athlete's
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2006 Higher Education Bond Report (2).Pdf
THE UNIVERSITY OF NORTH CAROLINA Report on the 2000 Higher Education Bond Program Joint Legislative Commission on Governmental Operations and Joint Legislative Education Oversight Committee September 2006 The Higher Education Facilities Financing Act bond program has entered into its sixth year and the constructed facilities are providing significant benefits to the students of the University of North Carolina and to the State. While providing more than 88,000 jobs, the program is ensuring that high quality resources, particularly in science and technology facilities, are available to students and researchers as North Carolina transitions from a manufacturing-based economy to one that is more knowledge-based and able to compete in the global environment. Over the last year, the campuses have made considerable progress. • All 318 of the bond projects are now under design, in construction or completed. Through July 2006, 36 projects are under design, 109 are in construction and 173 have been completed. • $2.19 billion or 88% of bond program dollars are now committed to design or construction contracts. It is expected that 90% of the bond program dollars will be committed by September 2006. • That the program will exceed $2 billion in expenditures in September 2006. • As part of its continuing commitment to contribute resources to its capital needs, the University has requested and the General Assembly has approved over $2.7 billion in projects from nonappropriated sources since 2000. • The program continues to exceed State goals recommended for Historically Underutilized Businesses (HUBs) by more than 60%. The University’s outreach efforts, including the “HUB Contractor Academy”, which teaches skills essential for managing a construction business, are building a momentum that promises long-term benefit for the minority contracting community. -

Chungdokwan Great Britain Newsletter
Taekwondo Chung Do Kwan Great Britain Newsletter A fantastic end to the year for TCGB Wow, where do I start - a lot has happened within the association over the last few months! In this issue we have a wide range of reports, including the opening of two new training halls, Scottish students sparring at an December 2010 international competition and an appeal to show off any of your Taekwondo- related tattoos (yep... you read that correctly). There are also articles on a Volume 2 high-energy Korean Taekwondo demonstration, the BTCB International Open in Manchester and the recent TCGB all-ages, all-grades seminar in Patron Swanmore. I really hope you enjoy reading this issue as much as I have Grandmaster Vincent enjoyed piecing it all together. Cheong (9th Dan) I would like to thank all the students and instructors that have kindly Officers 2010/11 provided articles for this edition. I cannot stress enough that without this kind of insightful input, the TCGB Newsletter would not be possible. Lets President maintain this momentum and continue to promote this mode of Grandmaster Lindsay communication between members. The next volume will be assembled at Lawrence (7th Dan) the beginning of April 2011, so please email us your articles by the end of March (just after the TCGB National Championships). Vice-President Best wishes over the festive period and enjoy your Taekwondo training! Grandmaster Mark Biddlecombe (7th Dan) David Honey TCGB Publicity Officer Technical Director Master Michael King Dan Grading Results (6th Dan) Congratulations -
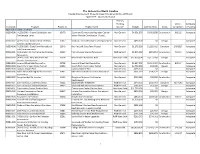
Institution Program Project ID Project Name Primary Funding Source
The University of North Carolina Capital Improvement Projects Report Required by S.L.2015-241 April 2017 - Quarterly Report Primary Funding Constr. Adequacy Institution Program Project ID Project Name Source* Budget Commitments Status Completion of Funding Appalachian State University 41230-308 [41230-308] - Steam Distribution and 10479 Steam and Condensate Upgrades Central Non-General $4,391,579 $4,361,838 Construction 6/3/16 Adequate Condensate Lines Steam Plant to Convocation Phase 1 41330-307 [41330-307] - Replacement of Steam 12067 Stadium Lot Condenstate Line Replacement Non-General $499,000 $0 Design Adequate System Condensate Line 41330-308 [41330-308] - State Farm Recreational 12040 Rec Fields @ State Farm Phase I Non-General $1,275,000 $1,269,419 Complete 1/3/2017 Adequate Field Improvements 41530-301 Panhellenic Hall Fermentation Sciences 12367 Fermentation Science Relocation R&R General $1,025,000 $811,853 Construction 7/1/16 Adequate Renovation 41530-302 [41430-304] - New Residence Hall - 12114 New Winkler Residence Hall Non-State Debt $32,000,000 $3,177,368 Design Adequate Winkler Replacement 41530-303 Howard Street Hall Renovation 12798 Howard Street Hall Renovation Non-General $2,657,905 $2,512,037 Construction 8/9/17 Adequate 41530-304 Steam Plant Vault Utility Tunnel 14052 Steam Plant Vault Utility Tunnel Non-General $2,750,000 $31,280 Design Adequate 41530-305 Campus Master Plan Campus Master Plan Non-General $375,000 $0 Adequate 41530-306 Miles Annas Building Wellness Center 15481 Miles Annas Wellness Center Renovation -

Appalachian State University
The University of North Carolina Capital Improvement Projects Report Required by S.L.2015-241 October 2017 - Quarterly Report Project Primary Funding Adequacy of Institution Program ID Project Name Source* Budget Commitments Status Constr. Completion Funding Appalachian State University [41230-308] - Steam Distribution and Steam and Condensate Upgrades Central Steam 41230-308 Condensate Lines 10479 Plant to Convocation Phase 1 Non-General $4,391,579 $4,361,838 Construction 06/03/2016 Adequate [41330-307] - Replacement of Steam System 41330-307 Condensate Line 12067 Stadium Lot Steam Manhole Repair Non-General $499,000 $33,900 Design Adequate Panhellenic Hall Fermentation Sciences 41530-301 Renovation 12367 Fermentation Science Relocation R&R General $1,025,000 $826,354 Construction 07/01/2016 Adequate [41430-304] - New Residence Hall - Winkler 41530-302 Replacement 12114 New Winkler Residence Hall Non-State Debt $32,000,000 $3,177,368 Design Adequate 41530-303 Howard Street Hall Renovation 12798 Howard Street Hall Renovation Non-General $2,657,905 $2,576,192 Construction 08/11/2017 Adequate 41530-304 Steam Plant Vault Utility Tunnel 14052 Steam Plant Vault Utility Tunnel Non-General $2,750,000 $226,571 Design Adequate 41530-305 Campus Master Plan Campus Master Plan Non-General $375,000 $0 Adequate Miles Annas Building Wellness Center 41530-306 Renovation 15481 Miles Annas Wellness Center Renovation Non-General $621,110 $596,670 Construction 11/18/2016 Adequate 41530-307 Doughton Hall Air Handler 14154 Doughton Make-up Air-Handler Replacement Non-General $440,669 $32,680 Construction Adequate 41530-308 2016 Carry-Forward 17256 Peacock Data Center Halon Replacement Non-General $175,000 $0 Adequate 41530-310 2016 Carry-Forward 17247 Chapel Wilson AC Replacement Non-General $105,000 $0 Adequate Physical Plant, Kerr Scott Hall, I.G. -

Gimghoul, She Why She Decided to Dig Into the Figured It May Cause a Stir
DTH/MATTIE COLLINS DTH/MATTIE On Feb. 12, Hanna Berg posted scanned pages from the secret society ‘s initiation rituals to a Facebook group. By Sasha Schroeder Inside the letter, sealed with red Staff Writer wax, there was one neatly-printed sentence: “LOOK NO FURTHER.” When sophomore Hanna Berg The public policy major heard a gave a speech in early February at a rumor that strange things happen to Dialectic and Philanthropic Societies people who pull documents from the meeting about the initiation rituals Order’s archives, which is precisely of the Order of Gimghoul, she why she decided to dig into the figured it may cause a stir. Wilson Library Special Collections, But she didn’t expect what would where she discovered the rituals. come next. According to a Wilson Library “I got a letter under my door that told me to stop looking,” Berg said. SEE GIMGHOUL, PAGE 6 Chapel Hill Nine monument erected on Franklin Street How to The monument was unveiled Chapel Hill Mayor Pam Hemminger vote in formed in 2017 to document the Civil at a ceremony on Friday — 60 Rights Movement in Chapel Hill. years after the historic sit-ins. “We decided we would like to honor brave events and things that Tuesday’s By Brittany McGee help shape us to being a better Staff Writer community,” Hemminger said. The marker, which was designed primary A group of Black high school by Durham artist Stephen Hayes, students set off a decade of civil rights has images of the protests and police PRIMARY 2020 demonstrations in Chapel Hill when officers outside of the drugstore, as well they sat down in a booth at Colonial as images of news headlines from the • Polls are open from Drug Store on Franklin Street on Feb. -

Alaga Syrup As a Symbol in King Hedley II
Vol. 2 | Summer 2020 Subverting the Role of Les Lieux de Memoire: Alaga Syrup as a Symbol in King Hedley II By Christopher Bell Associate Professor of English, University of North Georgia While the Alaga Billboard may evoke fond memories for those who recognize it, by the 1980s the Hill District, the setting of the play, was a food desert, a community wherein no healthy food options exist, and the product was no longer available in the neighborhood, rendering the presence of the Alaga billboard a negative symbol which complements Wilson’s depiction of the neighborhood as one that steadily declines during the second half of the Twentieth Century. Christopher Bell Abstract An analysis of the impact Alaga Syrup has had on Black communities and its relevance within August Wilson’s play, King Hedley II. Keywords August Wilson, Alaga Syrup, King Hedley II, Hill District, lieu de mémoire Introduction King Hedley II, the ninth play chronologically in August Wilson’s much lauded American Century Cycle, is the playwright’s darkest play. Set in 1985, approximately thirty years after the City of Pittsburgh began its so-called urban renewal project meant to revitalize the run-down Hill District neighborhood. The play focuses on the nadir of this plan. Beginning in the early 1950s, the city began demolishing the Lower Hill, displacing thousands of residents and shuttering hundreds of businesses. The Civic Arena was erected, establishing a tremendous source of income for both the white power structure and white owned businesses such as the Pittsburgh Penguins, while the Hill District benefitted little. -

Mechanics of the Jump Approach
MECHANICS OF THE JUMP APPROACH A Manuscript by Irving Schexnayder, University of Southwestern Louisiana Importance of the Jump Approach When projected into flight, the center of mass of any object (including the human body) follows a predetermined, predictable, unalterable parabolic curve. Thus, establishment of the proper flight path is totally dependant upon proper force application during ground contact. Since all takeoff forces, including eccentric forces, are applied while still in contact with the ground, any resultant rotations are produced during ground contact as well. These rotations continue into flight and assist or interfere with efficient landings and clearances. In light of these facts, it is obvious that proper force application at takeoff is the only way to produce good performances in the jumping events. Although good takeoffs produce good jumps, there are prerequisites to the execution of correct takeoff mechanics. Consider an athlete executing an approach run in a jumping event. A person running at relatively low speed can demonstrate greater accuracy in aligning the body into positions favorable for efficient takeoffs, because prior mechanical errors can be easily corrected. However, when dealing with the high velocities we see in competitive jumping, the correction of errors occurring during the run is limited due to time constraints, and is often impossible without great compromises. Also, at these higher velocities, reflexes play a much greater part in the pattern of movement, again minimizing the chances to correct earlier errors in body positioning. The execution of any part of an athletic endeavor is largely dependant upon the proper execution of prior parts. In cyclic tasks such as running, the correct execution of one cycle is prerequisite to the correct execution of the next cycle. -
The JUMP! Impact Fund Is an Initiative Created by the JUMP! Foundation to Bring Experiential Education to Youth in Underserved Communities
Impact The JUMP! Impact Fund is an initiative created by the JUMP! Foundation to bring experiential education to youth in underserved communities. The JUMP! Foundation is a non-profit social enterprise that uses experiential education to advance a world in which individuals, community leaders, and global citizens realize their passions and potential. GLOBAL HUB CHINA HUB CANADA HUB 1/5-1/6, Soi Ari 2, Phahonyothin Road No.15 9th Floor, Jingchao Mansion, SFU RADIUS Innovation Bangkok 10400 No.5 Nongzhangguan South Road, 308 W. Hastings Street, Thailand Chaoyang District, Beijing 100026 Vancouver, BC V6B 1K6 [email protected] JUMP! Impact The mission of JUMP! Impact is to: The Challenge? Today, children and youth aged 24 years and below make up nearly 40 percent of the world’s population, many of whom are concentrated in underdeveloped countries. Major challenges in these regions include inequity of wealth distribution, lack of employment opportunities, and rapid urbanization. The marginalization of youth in this context carries enormous negative implications for our global future as it causes a sense of disenfranchisement and lack of upward mobility, which can lead to ethnic, religious, and political conflicts1. Our Response? Innovative programming that utilizes experiential education to transform youth from under- served communities into globally competitive leaders for positives change in their lives and the world. We pair this approach with a unique methodology which brings together local NGOs, leaders, and youth to create sustainable impact. Where We Work 1. “Employment and Social Trends by Region.” World Employment and Social Outlook, vol. 2016, no. 1, 2016, pp. 27–59., doi:10.1002/wow3.77. -

Development of a Speed Model for Terrain Park Jumps
Project Number: CAB-001 ` THE DEVELOPMENT & SOCIETAL IMPACTS OF A SPEED MODEL FOR TERRAIN PARK JUMPS An Interactive Qualifying Project Report submitted to the Faculty of the WORCESTER POLYTECHNIC INSTITUTE in partial fulfillment of the requirements for the Degree of Bachelor of Science By Heather M. La Hart Date: Professor Chris A. Brown, IQP Advisor 1. Safety Analysis & Liability Project Number: CAB-001 ABSTRACT The objective of this project was to develop ways to design safer terrain parks. Two separate models, The Geometrical Jump Design Model and The Speed Model, were developed and produced criteria for the initial design and predicted the speed for any jump. To understand the opinions of society on terrain park safety and this research, questionnaires were distributed within the skiing culture. Through field data and surveys it was found that utilizing terrain park design models and integrating them into society and terrain would mostly be welcomed and used. ii Project Number: CAB-001 ACKNOWLEDGEMENTS I would first like to acknowledge Dan Delfino a fellow friend and student at WPI for his ongoing and continuous help, additions, and support of this project over the past two years. I would also like to thank my advisor Professor Chris Brown for the inspiration of this project, his continuous hard but helpful criticism, advice, guidance, and support throughout the entirety of this research. I would like to thank Hanna St.John for providing me a place to stay while conducting my research and support in Colorado. I would also like to thank the resorts of Copper Mountain and Breckenridge Mountain which made collecting data for this research possible. -

THE FINANCIAL LITERACY of YOUNG AMERICAN ADULTS Results of the 2008 National Jump$Tart Coalition Survey of High School Seniors and College Students
THE FINANCIAL LITERACY OF YOUNG AMERICAN ADULTS Results of the 2008 National Jump$tart Coalition Survey of High School Seniors and College Students By Lewis Mandell, Ph.D. University of Washington and the Aspen Institute For the Jump$tart Coalition® for Personal Financial Literacy THE JUMP$tart Coalition FOR PERSONAL FINANCIAL Literacy 919 18th Street, N.W. Suite 300 Washington, DC 20006 Phone: (888) 45-EDUCATE ● F ax: (202) 223-0321 E-mail: [email protected] THE FINANCIAL LITERACY OF YOUNG AMERICAN ADULTS - 2008 Mandell Lewis Mandell 1 THE FINANCIAL LITERACY OF YOUNG AMERICAN ADULTS TABLE OF CONTENTS Page Acknowledgements ..................................................................................................................4 Executive Summary .................................................................................................................5 Chapter 1 – The Financial Literacy of Young American Adults………………………… 7 Background – The 1997-98 Baseline Survey .............................................................7 Results of the 2000 Survey ..........................................................................................7 Results of the 2002 Survey ..........................................................................................7 Results of the 2004 Survey ......................................................................................... 8 Results of the 2006 Survey ..........................................................................................8 Results of the 2008 -

Dogs Diving for Dollars (D3 Series) Official Rulebook
2021 Dogs Diving for Dollars (D3 Series) Official Rulebook Last revision March 2021 www.d3series.com D3 Rulebook Copyright – Dogs Diving for Dollars 2021. All rights reserved Table of Contents Introduction . 3 Rules of Conduct/Sportsmanship. 3 Vaccinations . 4 Calls of Nature . 4 General Rules . 4 Definitions . 6 Entering an Event . 8 General Event Format . 8 Disciplines DOLLAR JUMP . 9 Divisions/Titles . 10 DOLLAR GRAB . 11 Divisions/Titles . 12 DOLLAR CATC . 13 Divisions/Titles . 13 DOLLAR TEAm . 14 Judging. 15 Resolving Ties . 15 Ribbons/Awards . 16 Junior Handler . 16 Lap Dogs . 17 Event Finals . .17 Championship Qualification . .17 Grand Championship . .17 Contesting a Score . 18 Refund policy . .18 Inclement Weather . 19 D3 Rulebook Copyright – Dogs Diving for Dollars 2021. All rights reserved 2 Introduction Dogs Diving for Dollars Series (hereby known as D3) is an independent governing body located in California, that hosts canine dock diving events. D3 promotes the active relationship between people and their dogs, by hosting the fun and exciting sport of dock diving. Safety and education of the handler and dogs are our number one priority. D3 will track the results, records and titles of all the dogs and handlers who enter our events. D3 was formed solely to promote the fun of dock diving competitions, which includes currently, jumping for distance, jumping to grab a suspended toy, and jumping to catch a toy in the air. Dogs compete and earn titles based on the distance they jump from a dock into a pool of water. The jump season for D3 is April 1st through September 30th, of any given year. -

Subject Knowledge Organiser Athletics – Track, Jump & Throw
Subject Knowledge Organiser Athletics – Track, Jump & Throw Sprint High jump Shot put This track event is a short running race. There are This jumping event requires athletes to jump This throwing event requires athletes to throw a generally three different sprint distances: 100m, over the bar using the Fosbury Flop technique. heavy metal ball called a shot as far as possible. 200m, and 400m. Stage one Start 8-10 strides away from the barrier. Run in a Drive phase curve with controlled speed. Lean your torso The drive is where you are looking to cover as into the curve, the opposite side to the barrier. much ground as possible through each stride, Keep your shoulder as high as possible. Stage one pushing with the leg that is in contact with the Hold the shot at the bottom and place the ground and driving the free leg through. In this Stage two thumb and little finger each side of the shot. phase the head must follow the body. You are ready to jump at approximately one Place the shot under the chin and touching the metre past the first post and an arm's length neck. Keep the throwing arm elbow high and the Transition phase away from the mat. At this point, plant the take- arm parallel to the floor. Stand on the balls of This transition phase is when you smoothly and off foot down. At the same time, drive your lead your feet with your knees bent and non-throwing gradually come upright into your stride. This is leg and arms upwards and shoulders high.