© in This Web Service Cambridge University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intestinal Obstruction Due to Pneumatosis Intestinalis ALED W
Postgrad Med J: first published as 10.1136/pgmj.43.504.680 on 1 October 1967. Downloaded from 680 Case reports Intestinal obstruction due to pneumatosis intestinalis ALED W. JONES F. M. COLE M.B., Ch.B., D.Path. M.D. Assistant Lecturer Lecturer Department ofPathology, University of Manchester PNEUMATOSIS intestinalis is a condition characterized Four years previously he had a perforated ulcer by the presence of numerous gas-filled cysts, most repaired surgically; no note was made at the time commonly found in the sub-serosa of the wall of the of any other lesion within the abdominal cavity. small intestine. Nearly 300 cases have been described Three years prior to admission he had a haema- and the literature of the adult cases has been re- temesis requiring blood transfusion. A barium meal viewed by Koss (1952), and those occurring in at this time suggested a certain amount of pyloric childhood and infancy by MacKenzie (1951). hold-up which was probably due to pylorospasm Although the cysts are frequently associated with caused by the duodenal ulcer; a second barium meal other intestinal lesions, they themselves are usually 1 year later showed no delay in gastric emptying. symptomless and rarely give rise to complications. For 6 months prior to the present admission he Those complications which have been described had, in addition to his ulcer pain, suffered a second include pneumo-peritoneum and intestinal obstruc- type of abdominal pain. This pain was situated in tion. Cysts can cause obstruction in several ways, the lower abdomen; it was intermittent, lasting up to one of which is by the formation of fibrous bands 1 week at a time, colicky in type and unrelieved by and strictures in relation to them, The following antacids. -

1979 Publications of the Staff of Henry Ford Hospital
Henry Ford Hospital Medical Journal Volume 27 Number 4 Article 2 12-1979 1979 Publications of the Staff of Henry Ford Hospital Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation (1979) "1979 Publications of the Staff of Henry Ford Hospital," Henry Ford Hospital Medical Journal : Vol. 27 : No. 4 , 310-337. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol27/iss4/2 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Henry Ford Hosp Med Journal Vol 27, No 4, 1979 1979 Publications of the Staff of Henry Ford Hospital Selected Abstracts and Titles Edited by George C. Bower, MD Abstracts Alam M, Madrazo AC, Magilligan DJ, Goldstein S. Mmode and two dimensional echocardiographic features of porcine valve dysfunction. Am J Cardiol 1979;43:502-09. We present the echocardiographic featuresof degeneration of nine loss ofthe cusp detail. In five patients severe regurgitation due to a glutaraldehyde-fixed porcine xenograft valves implanted in eight tear in one or more cusps developed in the valve in the mitral patients. These features occurred 11 to 68 months after implanta position. M mode echocardiography in all five patients revealed on tion and were correlated with surgical and necropsy findings. the valve systolic or diastolic fluttering echoes, or both. The two Acute bacterial endocard itis in three other patients 47 to 52 months dimensional echocardiogram demonstrated thickened cusps with before valve degeneration was recognized. -

Computed Tomography Colonography Imaging of Pneumatosis Intestinalis
Frossard et al. Journal of Medical Case Reports 2011, 5:375 JOURNAL OF MEDICAL http://www.jmedicalcasereports.com/content/5/1/375 CASE REPORTS CASEREPORT Open Access Computed tomography colonography imaging of pneumatosis intestinalis after hyperbaric oxygen therapy: a case report Jean-Louis Frossard1*, Philippe Braude2 and Jean-Yves Berney3 Abstract Introduction: Pneumatosis intestinalis is a condition characterized by the presence of submucosal or subserosal gas cysts in the wall of digestive tract. Pneumatosis intestinalis often remains asymptomatic in most cases but may clinically present in a benign form or less frequently in fulminant forms. Treatment for such conditions includes antibiotic therapy, diet therapy, oxygen therapy and surgery. Case presentation: The present report describes the case of a 56-year-old Swiss-born man with symptomatic pneumatosis intestinalis resistant to all treatment except hyperbaric oxygen therapy, as showed by computed tomography colonography images performed before, during and after treatment. Conclusions: The current case describes the response to hyperbaric oxygen therapy using virtual colonoscopy technique one month and three months after treatment. Moreover, after six months of follow-up, there has been no recurrence of digestive symptoms. Introduction form or less frequently in fulminant forms, the latter Pneumatosis intestinalis (PI) is a condition in which condition being associated with an acute bacterial pro- submucosal or subserosal gas cysts are found in the wall cess, sepsis, and necrosis of the bowel [1]. Symptoms of the small or large bowel [1]. PI may affect any seg- include abdominal distension, abdominal pain, diarrhea, ment of the gastrointestinal tract. The pathogenesis of constipation and flatulence, all symptoms that may lead PI is not understood but many different causes of pneu- to an erroneous diagnosis of irritable bowel syndrome matosis cystoides intestinalis have been proposed, [5]. -

Evidence-Based Management of Suspected Appendicitis in The
October 2011 Evidence-Based Management Volume 13, Number 10 Of Suspected Appendicitis In Authors Michael Alan Cole, MD Associate Physician, Department of Emergency Medicine, Brigham The Emergency Department and Women’s Hospital; Clinical Instructor, Harvard Medical School, Boston, MA Nicholas Maldonado, MD Abstract Emergency Physician, Brigham and Women’s Hospital/Massachusetts General Hospital, Harvard Affiliated Emergency Medicine Residency, Boston, MA Appendicitis is the most common cause of acute abdominal pain requiring surgical treatment in persons under 50 years of age, Peer Reviewers with a peak incidence in the second and third decades. Women John Howell, MD, FACEP, FAAEM Clinical Professor of Emergency Medicine, The George Washington have a greater risk of misdiagnosis and a higher negative appen- University, Washington, DC; Director of Academics and Risk Management, dectomy rate. Atypical presentations of appendicitis are com- Best Practices, Inc., Inova Fairfax Hospital, Falls Church, VA monly misdiagnosed, resulting in increased morbidity, mortality, Christopher Strother, MD Assistant Professor of Emergency Medicine and Pediatrics, Director, and potential litigation. The variability of presentation relates to Emergency and Undergraduate Simulation, Mount Sinai School of the varied anatomical location and the visceral innervation of the Medicine, New York, NY appendix. Patients presenting with possible appendicitis should Robert Vissers, MD, FACEP be risk stratified based on history, physical examination, and Chief, Emergency Medicine, Quality Director, Legacy Emanuel Hospital, Adjunct Associate Professor, Oregon Health & Science University School laboratory data. An elevated white blood cell (WBC) count alone of Medicine, Portland, OR (> 10,000 cells/mm3) offers poor diagnostic utility; however, CME Objectives combining WBC count > 10 and C-reactive protein (CRP) level > Upon completion of this article, you should be able to: 8 achieves notable predictive power in the diagnosis of acute ap- 1. -

Pneumatosis Intestinalis in Solid Organ Transplant Recipients
1997 Review Article Pneumatosis intestinalis in solid organ transplant recipients Vincent Gemma1, Daniel Mistrot1, David Row1, Ronald A. Gagliano1, Ross M. Bremner2, Rajat Walia2, Atul C. Mehta3, Tanmay S. Panchabhai2 1Department of Surgery, 2Norton Thoracic Institute, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA; 3Department of Pulmonary Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA Contributions: (I) Conception and design: D Row, RA Gagliano, TS Panchabhai; (II) Administrative support: RM Bremner, R Walia; (III) Provision of study materials or patients: V Gemma, D Mistrot, TS Panchabhai; (IV) Collection and assembly of data: V Gemma, D Mistrot, TS Panchabhai; (V) Data analysis and interpretation: RA Gagliano, RM Bremner, R Walia, AC Mehta, TS Panchabhai; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Tanmay S. Panchabhai, MD, FCCP. Associate Director, Pulmonary Fibrosis Center/Co-Director, Lung Cancer Screening Program, Norton Thoracic Institute, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA; Associate Professor of Medicine, Creighton University School of Medicine, Omaha, NE, USA. Email: [email protected]. Abstract: Pneumatosis intestinalis (PI) is an uncommon medical condition in which gas pockets form in the walls of the gastrointestinal tract. The mechanism by which this occurs is poorly understood; however, it is often seen as a sign of serious bowel ischemia, which is a surgical emergency. Since the early days of solid organ transplantation, PI has been described in recipients of kidney, liver, heart, and lung transplant. Despite the dangerous connotations often associated with PI, case reports dating as far back as the 1970s show that PI can be benign in solid organ transplant recipients. -

Scientific Letters
SCIENTIFIC LETTERS concerned. A confirmatory DNA test would prevent this supportive evidence for suspected NEe. For'confirmed NEe' situation. any of the following clinical criteria were diagnostic: severe abdominal distension, occult blood in stool, bile-stained JMHeckmann vomiting, persistent ileus, pneumatosis intestinalis or bowel A Bryer perforation requiring surgical intervention.' Neurology Unit Survey for rotavirus and ESKP. Stool specimens from all Groote Schuur Hospital and patients in both intermediate care wards were submitted for University ofCape Town rotavirus detection in a cross-sectional survey. Bi-weekly rectal swabs from all patients were submitted for ESKP culture as LJ Greenberg part of the infection control strategy. Department ofHuman Genetics Microbiology and virology. Rectal swabs were taken on dry, University ofCape Town cotton-tipped swabs. Stool samples were collected in sterile 1. Warner JP. Harmn L, Brock D]p. A new polymerase chain reaction (PCR) assay for the containers. All swabs were cultured on McConkey medium trinucleotide repeat that is unstable and expanded in Huntington's disease chromosomes. Mol Cell Probes 1993; 7: 235-239. (Biolab Diagnostics, Midrand, RSA) supplemented with 2. Gusella]F, Persichetti F, MacDonald ME. The genetic defect causing Huntington's disease: cefotaxime 0.5 mg/l, selecting organisms resistant to third repeated. in other contexts? Mol Med 1997; 3: 238-246. 5 3. Hayden MR. HWltington's chorea in South Africa. PhD thesis, University of Cape Town generation cephalosporins. Identification of K. pneumoniae was 1979: 137-159. verified by dehydrolisation of arginine, decarboxylation of 4. Corse!lis IAN. Aging and the dementias. In: Blackwood )W. Corsellis IAN. eels. -
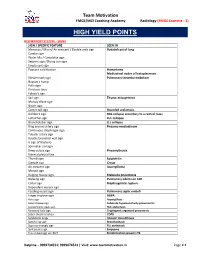
High Yield Points
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB -

Acute Appendicitis: Hispanics and the Hamburger Sign
Research Article More Information *Address for Correspondence: Romero- Acute Appendicitis: Hispanics and the Vazquez Ana M, MS, Ponce Health and Sciences University, Ponce, Puerto Rico- School of Medicine, Puerto Rico, Tel: (787)363-6739; Hamburger Sign Email: [email protected]; [email protected] 1 1 1 Garcia Gubern C , Colon Rolón L , Ruiz Mercado I , Oliveras Submitted: 12 November 2019 Garcia C1, Caban Acosta D1, Muñoz Pagán J1, Iriarte I3, Bolaños Approved: 19 November 2019 Published: 20 November 2019 Ávila G2, Peguero Rivera J2, Sánchez Gaetan F2, Oneill Castro J2, 1 1 How to cite this article: Garcia Gubern C, Colon Cordero Colón Paola N , Garcia-Colon Carlos A and Romero- Rolón L, Ruiz Mercado I, Oliveras Garcia C, Caban 4 Vazquez Ana M * Acosta D, et al. Acute Appendicitis: Hispanics and the Hamburger Sign. Arch Surg Clin Res. 1 MD, Department of Emergency Medicine Hospital San Lucas, Ponce, Puerto Rico 2019; 3: 078-081. 2Department of Surgery Hospital San Lucas, Ponce, Puerto Rico DOI: dx.doi.org/10.29328/journal.ascr.1001041 3Ponce Health and Sciences University, Ponce, School of Public Health, Puerto Rico ORCiD: orcid.org/0000-0001-7214-0748 4Ponce Health and Sciences University, Ponce, School of Medicine, Puerto Rico Copyright: © 2019 Garcia Gubern C, et al. This is an open access article distributed under the Creative Commons Attribution License, Abstract which permits unrestricted use, distribution, and reproduction in any medium, provided the Objective: To describe the presenting clinical fi ndings of patients with acute appendicitis and original work is properly cited. compare them with those described in the medical literature. -

Netherlands Journal of Critical Care
Volume 26 - No 2 - March 2018 Netherlands Journal of Critical Care Bi-monthly journal of the Dutch Society of Intensive Care REVIEW ORIGINAL ARTICLE CASE REPORT Ultrasound imaging of the diaphragm: facts and To see or not to see: ultrasound-guided Hepatopulmonary syndrome – a rare cause of future: A guide for the bedside clinician percutaneous tracheostomy hypoxaemia M.E. Haaksma, L. Atmowihardjo, L. Heunks, J.E. Lopez Matta, C.V. Elzo Kraemer, D.J. van Westerloo W.A.C. Koekkoek, C.R. Lamers, R. Meiland, A. Spoelstra-de Man, P.R. Tuinman M.J. van der Veen, D.C. Burgers – Bonthuis 2018 NVIC NAJAARSCONGRES 13 september 2018 SAVE THE DATE WWW.NVIC.NL NVIC_SAVE THE DATE 2018_210x275_TBV_NJCC_MAGAZINE.indd 1 08-03-18 18:39 Netherlands Journal of Critical Care 2018 NETHERLANDS JOURNAL OF CRITICAL CARE EXECUTIVE EDITORIAL BOARD N.P. Juffermans, editor in chief CONTENTS I. van Stijn, managing editor H. Dupuis, language editor J. Horn, editorial board EDITORIAL A.P.J. Vlaar, editorial board 56 The golden age of ultrasound is only just beginning M. Kuiper, associate editor P. Spronk, associate editor F.H. Bosch, P.R. Tuinman [email protected] REVIEW COPYRIGHT 58 Ultrasound imaging of the diaphragm: facts and future: A guide for the bedside clinician Netherlands Journal of Critical Care ISSN: 1569-3511 M.E. Haaksma, L. Atmowihardjo, L. Heunks, A. Spoelstra-de Man, P.R. Tuinman NVIC p/a Domus Medica P.O. Box 2124, 3500 GC Utrecht T: +31-(0)30 - 282 38 38 ORIGINAL ARTICLE 66 To see or not to see: ultrasound-guided percutaneous tracheostomy © 2018 NVIC. -

Acute Appendicitis in Adults
International Surgery Journal Vagholkar K. Int Surg J. 2020 Sep;7(9):3180-3186 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: http://dx.doi.org/10.18203/2349-2902.isj20203822 Review Article Acute appendicitis in adults Ketan Vagholkar* Department of Surgery, D. Y. Patil University School of Medicine, Navi Mumbai, Maharashtra, India Received: 16 June 2020 Revised: 28 July 2020 Accepted: 03 August 2020 *Correspondence: Dr. Ketan Vagholkar, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Acute appendicitis is one of the commonest abdominal emergency encountered by a general surgeon. Understanding the surgical pathology is pivotal in identifying the stage of disease at which the patient presents for better correlation of clinical features, laboratory and imaging reports. Various scoring systems enhance and aid this process. Imaging confirms the diagnosis. Early diagnosis is essential to prevent complications. Surgery is the mainstay of treatment. Appendicitis may present in various forms in different clinical settings. A uniform approach to presentations may not always yield good results. Though appendectomy is the mainstay of treatment yet a tailor made surgical plan needs to be developed after holistic evaluation of the patient. The article discusses the differential surgical approach based on the etiopathogenesis, diagnosis and variable clinical presentations. Keywords: Acute appendicitis, Diagnosis, Scoring, Treatment INTRODUCTION decreased bowel transit time and reduces the formation of faecoliths, which lead to obstruction and initiation of the Acute appendicitis is one of the most common abdominal inflammatory cascade.2-4 The disease is more common in emergency managed by a general surgeon. -

Surgical Abdomen
GI module Jane R. Perlman Fellowship Program Nurse Practitioner and Physician Assistant Fellowship in Emergency Medicine Jennifer S. Foster PA-C Dina Mantis PA-C Acute Abdomen – causes Acute appendicitis Acute mesenteric ischemia/ischemic colitis Perforated bowel, acute peptic ulcer or tumor Spectrum of cholecystitis Asymptomatic gallstones Biliary colic Acute Cholecystitis Choledocholithiasis Cholangitis Pancreatitis Hemoperitoneum – perforated AAA, trauma, surgery Abcess Bariatric surgery complications Acute abdomen Worry about abdominal pain in elderly, children, HIV infection, immune suppressed from steroids or chemotherapy History questions to ask: MerckManuals.com Where is the pain? What is the pain like? Have you had it before? Yes – recurrent problem such as ulcers, biliary colic, diverticulitis, mittelsherz No – think perforated ulcer, ectopic pregnancy, torsion How severe is pain? Pain out of proportion – mesenteric ischemia Does pain travel to other body parts? Right scapula – gallbladder pain Left shoulder – ruptured spleen, pancreatitis Other questions re abdominal pain: What relieves the pain? Sitting up right and leaning forward, think acute pancreatitis What other sx occur with the pain? a) vomiting before pain, then diarrhea = gastroenteritis b) delayed vomiting, no bowel movements, no gas = acute intestinal obstruction, SBO c) severe vomiting, then intense epigastric left chest or shoulder pain = perforation of esophagus Other historical questions the surgeon will want to know: Prior surgeries Surgical history, when – how recently, what, where, who did it? Also postop complications, postop course Pregnant or not Physical exam General, are they texting and talking and telling you pain is 10/10 or quiet, pale and diaphoretic? Ask patient where most tender area is, then start away from there, listen first, then percuss and palpate. -

12.2% 125000 145M Top 1% 154 5000
We are IntechOpen, the world’s leading publisher of Open Access books Built by scientists, for scientists 5,000 125,000 145M Open access books available International authors and editors Downloads Our authors are among the 154 TOP 1% 12.2% Countries delivered to most cited scientists Contributors from top 500 universities Selection of our books indexed in the Book Citation Index in Web of Science™ Core Collection (BKCI) Interested in publishing with us? Contact [email protected] Numbers displayed above are based on latest data collected. For more information visit www.intechopen.com Provisional chapter Clinical Approach in the Diagnosis of Acute Appendicitis Alfredo Alvarado Additional information is available at the end of the chapter Abstract Abdominal pain is the most common reason for consultation in the emergency depart- ment, and most of the times, its cause is an episode of acute appendicitis. However, the misdiagnosis rate of acute appendicitis is high due to the unusual presentation of the symptoms. Therefore, the clinician has to be very alert in order to establish a correct diagnosis. Keywords: diagnosis of acute appendicitis, clinical approach, Alvarado score 1. Introduction The lifetime risk of appendicitis is 8.6% for males and 6.7% for females with an overall preva- lence of 7% worldwide. The incidence of acute appendicitis has been declining steadily since the late 1940s, and the current annual incidence is 10 cases per 100,000 population. In Asian and African countries, the incidence of acute appendicitis is probable lower because of the dietary habits of the inhabitants of these geographic areas.