PACKAGE INSERT TEMPLATE for ATENOLOL TABLET Brand Or Product Name
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
667783-Atenolol (ACC-UK)06-16-SPC-PIL
Artwork No. - Colours Used Customer Accord Pantone Black Description Atenolol Market UK Language English Size 170 x 550 mm PIL Min. Font Size 9.5 Version No. 13 (Page 1 of 2) (06-16-Atenolol SPC) Date 07_05_16 (Atenolol (ACC-UK)06-16-SPC-PIL) Prepared By Checked By Approved By Regulatory Affairs Regulatory Affairs Quality Assurance You must consult your doctor if you are If you forget to take Atenolol Tablets 6. Contents of the pack and other planning to combine Atenolol tablets with the If you forget to take a dose of the Atenolol information medicines listed below: Tablet, take it as soon as you remember, PACKAGE LEAFLET: INFORMATION FOR • Clonidine (for high blood pressure or unless it is time for your next dose. What Atenolol Tablet contains THE USER migraine). If you are taking clonidine and Do not take a double dose to make up for a • The active ingredient is Atenolol. Atenolol 25 mg Tablets Atenolol tablets together, do not stop taking forgotten dose. • The other ingredients are Heavy clonidine unless your doctor tells you to do Magnesium Carbonate, Maize Starch, Atenolol 50 mg Tablets so. If you have to stop taking clonidine, your If you stop taking Atenolol Tablets Sodium Lauryl Sulphate, Gelatin, doctor will give you careful instructions Do not stop taking Atenolol Tablets without Magnesium Stearate, Microcrystalline Atenolol 100 mg Tablets about how to do it. talking to your doctor. In some cases, you may Cellulose and Purified Talc. (Atenolol) • Verapamil, diltiazem and nifedipine (for high need to stop taking it gradually over 7-14 days blood pressure or chest pain). -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Pms-ATENOLOL Atenolol Tablets, BP 25 Mg, 50 Mg and 100 Mg
- PRODUCT MONOGRAPH Pr pms-ATENOLOL Atenolol Tablets, BP 25 mg, 50 mg and 100 mg Beta-adrenergic receptor blocking agent PHARMASCIENCE INC. Date of Revision: 6111 Royalmount Ave., Suite 100 November 3, 2017 Montreal, Quebec H4P 2T4 www.pharmascience.com Submission Control No: 201217 PRODUCT MONOGRAPH NAME OF DRUG Prpms-ATENOLOL Atenolol Tablets, BP 25 mg, 50 mg and 100 mg THERAPEUTIC CLASSIFICATION Beta-adrenergic receptor blocking agent ACTIONS AND CLINICAL PHARMACOLOGY Atenolol is a beta1-selective, beta adrenergic blocking agent, devoid of membrane stabilizing or intrinsic sympathomimetic (partial agonist) activities. It is a racemic mixture and the beta1 properties reside in the S (-) enantiomer. Beta1-selectivity decreases with increasing dose. The mechanism of the antihypertensive effect has not been established. Among the factors that may be involved are: a) competitive ability to antagonize catecholamine-induced tachycardia at the beta-receptor sites in the heart, thus decreasing cardiac output b) inhibition of renin release by the kidneys c) inhibition of the vasomotor centres The mechanism of the anti-anginal effect is also uncertain. An important factor may be the reduction of myocardial oxygen requirements by blocking catecholamine-induced increases in heart rate, systolic blood pressure, and the velocity and extent of myocardial contraction. In man atenolol reduces both isoproterenol- and exercise-induced increases in heart rate over the dose range of 50 to 200 mg. At an oral dose of 100 mg the beta1 blocking effects persist for at least 24 hours; the reduction in exercise-induced heart rate increase being about 32% and 13%, 2 and 24 hours after dosing, respectively. -

Migraine Headache Prophylaxis Hien Ha, Pharmd, and Annika Gonzalez, MD, Christus Santa Rosa Family Medicine Residency Program, San Antonio, Texas
Migraine Headache Prophylaxis Hien Ha, PharmD, and Annika Gonzalez, MD, Christus Santa Rosa Family Medicine Residency Program, San Antonio, Texas Migraines impose significant health and financial burdens. Approximately 38% of patients with episodic migraines would benefit from preventive therapy, but less than 13% take prophylactic medications. Preventive medication therapy reduces migraine frequency, severity, and headache-related distress. Preventive therapy may also improve quality of life and prevent the progression to chronic migraines. Some indications for preventive therapy include four or more headaches a month, eight or more headache days a month, debilitating headaches, and medication- overuse headaches. Identifying and managing environmental, dietary, and behavioral triggers are useful strategies for preventing migraines. First-line med- ications established as effective based on clinical evidence include divalproex, topiramate, metoprolol, propranolol, and timolol. Medications such as ami- triptyline, venlafaxine, atenolol, and nadolol are probably effective but should be second-line therapy. There is limited evidence for nebivolol, bisoprolol, pindolol, carbamazepine, gabapentin, fluoxetine, nicardipine, verapamil, nimodipine, nifedipine, lisinopril, and candesartan. Acebutolol, oxcarbazepine, lamotrigine, and telmisartan are ineffective. Newer agents target calcitonin gene-related peptide pain transmission in the migraine pain pathway and have recently received approval from the U.S. Food and Drug Administration; how- ever, more studies of long-term effectiveness and adverse effects are needed. The complementary treatments petasites, feverfew, magnesium, and riboflavin are probably effective. Nonpharmacologic therapies such as relaxation training, thermal biofeedback combined with relaxation training, electromyographic feedback, and cognitive behavior therapy also have good evidence to support their use in migraine prevention. (Am Fam Physician. 2019; 99(1):17-24. -
Clomipramine 25 Mg Capsules, Hard
Package leaflet: Information for the patient Other medicines and Clomipramine Tell your doctor if you are taking, have recently Clomipramine 10 mg Capsules, Hard taken or might take any other medicines. Clomipramine 25 mg Capsules, Hard Some medicines may increase the side effects of Clomipramine 50 mg Capsules, Hard Clomipramine and may sometimes cause very clomipramine hydrochloride serious reactions. Do not take any other medicines whilst taking Clomipramine without first talking to Read all of this leaflet carefully before you your doctor, especially: start taking this medicine because it contains - medicines for depression, particularly MAOIs (see important information for you. section “Do not take” above) e.g. tranylcypromine, - Keep this leaflet. You may need to read it again. phenelzine, moclobemide; SSRIs e.g. fluoxetine (or - If you have any further questions, ask your have taken within the last 3 weeks), fluvoxamine, doctor or pharmacist. paroxetine, sertraline; SNaRIs e.g. venlafaxine; - This medicine has been prescribed for you only. tricyclic and tetracyclic antidepressants e.g. Do not pass it on to others. It may harm them, amitriptyline, dothiepin, maprotiline even if their signs of illness are the same as yours. - diuretics, also known as ‘water tablets’, e.g. - If you get any side effects, talk to your doctor bendroflumethiazide, furosemide or pharmacist. This includes any possible side - anaesthetics, used for the temporary loss of effects not listed in this leaflet. See section 4. bodily sensation - antihistamines e.g. terfenadine What is in this leaflet - medicines for other mental health conditions 1. What Clomipramine is and what it is used for. such as schizophrenia or manic depression 2. -
Atenolol 25Mg, 50Mg and 100Mg Tablets
PhCode PhCode 25 mm Package leaflet: Information for the patient Atenolol 25mg, 50mg and 100mg tablets Read all of this leaflet carefully before you Warnings and Precautions start taking this medicine because it contains Talk to your doctor or pharmacist before taking important information for you. Atenolol tablets if you have: • asthma, wheezing or any other similar breathing • Keep this leaflet. You may need to read it again. problems, or you get allergic reactions, for example to • If you have any further questions, ask your insect stings. If you have ever had asthma or wheezing, doctor or pharmacist. do not take this medicine without first checking with • This medicine has been prescribed for you only. your doctor. Do not pass it on to others. It may harm them, • a type of chest pain (angina) called Prinzmetal’s angina. even if their signs of illness are the same as • poor blood circulation or controlled heart failure. yours. • first-degree heart block. • If you get any side effects, talk to your doctor • diabetes. Your medicine may change how you respond or pharmacist. This includes any possible side to having low blood sugar. You may feel your heart effects not listed in this leaflet. See section 4. beating faster. • thyrotoxicosis (a condition caused by an overactive What is in this leaflet thyroid gland). Your medicine may hide the symptoms of thyrotoxicosis. 1 What Atenolol tablets are and what they • problems with your kidneys. You may need to have are used for some check-ups during your treatment. 2 What you need to know before you take Other medicines and Atenolol tablets Atenolol tablets Tell your doctor or pharmacist if you are taking or have 3 How to take Atenolol tablets recently taken or might take any other medicines, including 4 Possible side effects medicines obtained without a prescription. -

Currently Prescribed Psychotropic Medications
CURRENTLY PRESCRIBED PSYCHOTROPIC MEDICATIONS Schizophrenia Depression Anxiety Disorders 1st generation antipsychotics: Tricyclics: Atarax (hydroxyzine) Haldol (haloperidol), *Anafranil (clomipramine) Ativan (lorazepam) Haldol Decanoate Asendin (amoxapine) BuSpar (buspirone) Loxitane (loxapine) Elavil (amitriptyline) *Inderal (propranolol) Mellaril (thioridazine) Norpramin (desipramine) Keppra (levetiracetam) Navane (thiothixene) Pamelor (nortriptyline) *Klonopin (clonazepam) Prolixin (fluphenazine), Prolixin Sinequan (doxepin) Librium (chlordiazepoxide) Decanoate Spravato (esketamine) Serax (oxazepam) Stelazine (trifluoperazine) Surmontil (trimipramine) Thorazine (chlorpromazine) *Tenormin (atenolol) Tofranil (imipramine) MEDICATIONS PSYCHOTROPIC PRESCRIBED CURRENTLY Trilafon (perphenazine) Tranxene (clorazepate) Vivactil (protriptyline) Valium (diazepam) 2nd generation antipsychotics: Zulresso (brexanolone) Vistaril (hydroxyzine) Abilify (aripiprazole) Aristada (aripiprazole) SSRIs: Xanax (alprazolam) Caplyta (lumateperone) Celexa (citalopram) *Antidepressants, especially SSRIs, are also used in the treatment of anxiety. Clozaril (clozapine) Lexapro (escitalopram) Fanapt (iloperidone) *Luvox (fluvoxamine) Geodon (ziprasidone) Paxil (paroxetine) Stimulants (used in the treatment of ADD/ADHD) Invega (paliperidone) Prozac (fluoxetine) Invega Sustenna Zoloft (sertraline) Adderall (amphetamine and Perseris (Risperidone injectable) dextroamphetamine) Latuda (lurasidone) MAOIs: Azstarys(dexmethylphenidate Rexulti (brexpiprazole) Emsam (selegiline) -
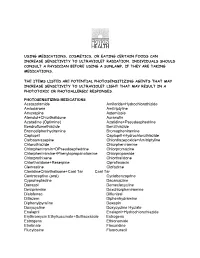
Using Medications, Cosmetics, Or Eating Certain Foods Can Increase Sensitivity to Ultraviolet Radiation
USING MEDICATIONS, COSMETICS, OR EATING CERTAIN FOODS CAN INCREASE SENSITIVITY TO ULTRAVIOLET RADIATION. INDIVIDUALS SHOULD CONSULT A PHYSICIAN BEFORE USING A SUNLAMP, IF THEY ARE TAKING MEDICATIONS. THE ITEMS LISTED ARE POTENTIAL PHOTOSENSITIZING AGENTS THAT MAY INCREASE SENSITIVITY TO ULTRAVIOLET LIGHT THAT MAY RESULT IN A PHOTOTOXIC OR PHOTOALLERGIC RESPONSES. PHOTOSENSITIZING MEDICATIONS Acetazolamide Amiloride+Hydrochlorothizide Amiodarone Amitriptyline Amoxapine Astemizole Atenolol+Chlorthalidone Auranofin Azatadine (Optimine) Azatidine+Pseudoephedrine Bendroflumethiazide Benzthiazide Bromodiphenhydramine Bromopheniramine Captopril Captopril+Hydrochlorothiazide Carbaamazepine Chlordiazepoxide+Amitriptyline Chlorothiazide Chlorpheniramine Chlorpheniramin+DPseudoephedrine Chlorpromazine Chlorpheniramine+Phenylopropanolamine Chlorpropamide Chlorprothixene Chlorthalidone Chlorthalidone+Reserpine Ciprofloxacin Clemastine Clofazime ClonidineChlorthalisone+Coal Tar Coal Tar Contraceptive (oral) Cyclobenzaprine Cyproheptadine Dacarcazine Danazol Demeclocycline Desipramine Dexchlorpheniramine Diclofenac Diflunisal Ditiazem Diphenhydramine Diphenylpyraline Doxepin Doxycycline Doxycycline Hyclate Enalapril Enalapril+Hydrochlorothiazide Erythromycin Ethylsuccinate+Sulfisoxazole Estrogens Estrogens Ethionamide Etretinate Floxuridine Flucytosine Fluorouracil Fluphenazine Flubiprofen Flutamide Gentamicin Glipizide Glyburide Gold Salts (compounds) Gold Sodium Thiomalate Griseofulvin Griseofulvin Ultramicrosize Griseofulvin+Hydrochlorothiazide Haloperidol -

List of Formulary Drug Removals
July 2021 Formulary Drug Removals Below is a list of medicines by drug class that have been removed from your plan’s formulary. If you continue using one of the drugs listed below and identified as a Formulary Drug Removal, you may be required to pay the full cost. If you are currently using one of the formulary drug removals, ask your doctor to choose one of the generic or brand formulary options listed below. Category Formulary Drug Formulary Options Drug Class Removals Acromegaly SANDOSTATIN LAR SOMATULINE DEPOT SIGNIFOR LAR SOMAVERT Allergies dexchlorpheniramine levocetirizine Antihistamines Diphen Elixir RyClora CARBINOXAMINE TABLET 6 MG Allergies BECONASE AQ flunisolide spray, fluticasone spray, mometasone spray, DYMISTA Nasal Steroids / Combinations OMNARIS QNASL ZETONNA Anticonvulsants topiramate ext-rel capsule carbamazepine, carbamazepine ext-rel, clobazam, divalproex sodium, (generics for QUDEXY XR only) divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, rufinamide, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT, XCOPRI BANZEL SUSPENSION clobazam, lamotrigine, rufinamide, topiramate, TROKENDI XR ONFI SABRIL vigabatrin ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium -

Drug-Induced Sleepiness and Insomnia: an Update Sonolência E Insônia Causadas Por Drogas: Artigo De Atualização
36 Drug-induced sleepiness UPDATE ARTICLE Drug-induced sleepiness and insomnia: an update Sonolência e insônia causadas por drogas: artigo de atualização Renato Gonçalves1, Sonia Maria Guimarães Togeiro2 ABSTRACT doctor’s task is more complex as more comorbid conditions are Medical practice of sleep medicine requires an extensive found in these patients, which makes patient evaluation more pharmacological knowledge, especially when you need to make difficult and intriguing. decisions about the drug scheme already adopted by a given In this update, we focus on the potential for sedation patient. The care of patients with multiple diseases and using of or insomnia of drugs used in the most common chronic multiple drugs has become common. The great challenge facing the physician is to what extent one or more drugs may be contributing diseases worldwide. Doctors often treat patients with multiple to the complaint of sleepiness or insomnia. Any drug with activity comorbidities. It is estimated that 25% of the population of in the central nervous system has the potential to affect sleep-wake North America presents more than one chronic disease(1). cycle. The pharmacokinetic drug knowledge’s will be useful in Among the more prevalent chronic diseases across the world are determining the likelihood of adverse effects on sleep-wake functioning. In this article we describe the potential sedative or in cardiovascular diseases (systemic hypertension, congestive heart generating insomnia by drugs used in the major chronic diseases in failure, and coronary insufficiency), diabetes mellitus, chronic the population. obstructive pulmonary diseases, arthritis, depression, and cere- Keywords: conscious sedation, drugs, hypersomnia, sleep, sleep brovascular accident(2). -

High-Risk Medication Pocket Guide
High-Risk Medication Pocket Guide Therapeutic Class High-Risk Medication Potential Risks Alternative Medication Option Antihistamines Brompheniramine, Carbinoxamine, Highly anticholinergic (can cause dry mouth, flushing, dry Allergies: Cetirizine, Fexofenadine, Loratadine, Chlorpheniramine, Clemastine, skin, confusion, or difficulty urinating); Sedation. Levocetirizine (as a single agent or as Cyproheptadine, Dexbrompheniramine, Anxiety: Buspirone, SSRIs (Fluoxetine, Paroxetine), part of a combination Dexchlorpheniramine, Diphenhydramine SNRIs (Venlafaxine, Cymbalta) product) - excludes (oral), Doxylamine, Hydroxyzine, OTC products Promethazine, Triprolidine Insomnia: Melatonin, low-dose Trazodone Anti-Infectives Nitrofurantoin (when cumulative day supply Potential for pulmonary toxicity or peripheral neuropathy Infection: Ciprofloxacin, Trimethoprim/ is >90 days during plan year) (numbness, tingling, or pain in the hands, feet, or toes. Sulfamethoxazole, Amoxicillin/Clavulanate, Muscle weakness. Cephalexin Difficulty walking and/or problems with balance or coordination). Antiparkinson Agents Benztropine (oral), Trihexyphenidyl Highly anticholinergic (can cause dry mouth, flushing, Parkinson Disease: Selegiline, dry skin, confusion, or difficulty urinating); Carbidopa/Levodopa, Ropinirole, Pramipexole, Not recommended for prevention of extrapyramidal Entacapone symptoms with antipsychotics due to potential Antipsychotic induced Extrapyramidal Symptoms: hallucinations. Quetiapine, Clozapine Antipsychotics Thioridazine Highly anticholinergic -

Medications to Avoid in Long QT Syndrome
Jackie Crawford Cardiac Inherited Disease Co-ordinator C/- Paediatric Cardiology; Level 3 Starship; Auckland City Hospital Private Bag 92024; Auckland Cardiac Inherited Disease Registry Phone: (09) 3074949 ext 23634 www.cidg.org Fax: (09) 6309877 Email: [email protected] Medications to be avoided, or requiring special caution, in people with Long QT syndrome This list includes medications which prolong the QT interval and is meant as a guide for people with Long QT syndrome, or acquired long QT interval from heart muscle disease, and their parents or guardians. It should not be seen as all inclusive. Those prescribing any medication to someone with Long QT syndrome should always check the drug specifications and contra-indications. The list has been compiled by review of publications and/or drug advice sheets provided with medications. Check also www.SADS.org and www.Torsades .org. Antibiotics Erythromycin, Clarithromycin, Gatifloxacin, levofloxacin, Moxifloxacin Sulfamethoxazole-trimethoprim (Septrin/Bactrim), Spiramycin, Pentamidine Antihistamines Terfenadine, Astemizole, Diphenhydramine, (These are particularly to be avoided (even in normal subjects) in combination with Erythromycin or grapefruit juice or the antifungals ketoconazole, miconazole, fluconazole or itraconazole) [Antihistamines that may be used safely are loratidine, cetirizine and fexofenadine, and phenergan] Appetite suppressants Fenfluramine, phentermine, Sibutramine Asthma treatments The Beta-2 agonists (e.g. Terbutaline, Salbutamol, Salmeterol) both work against