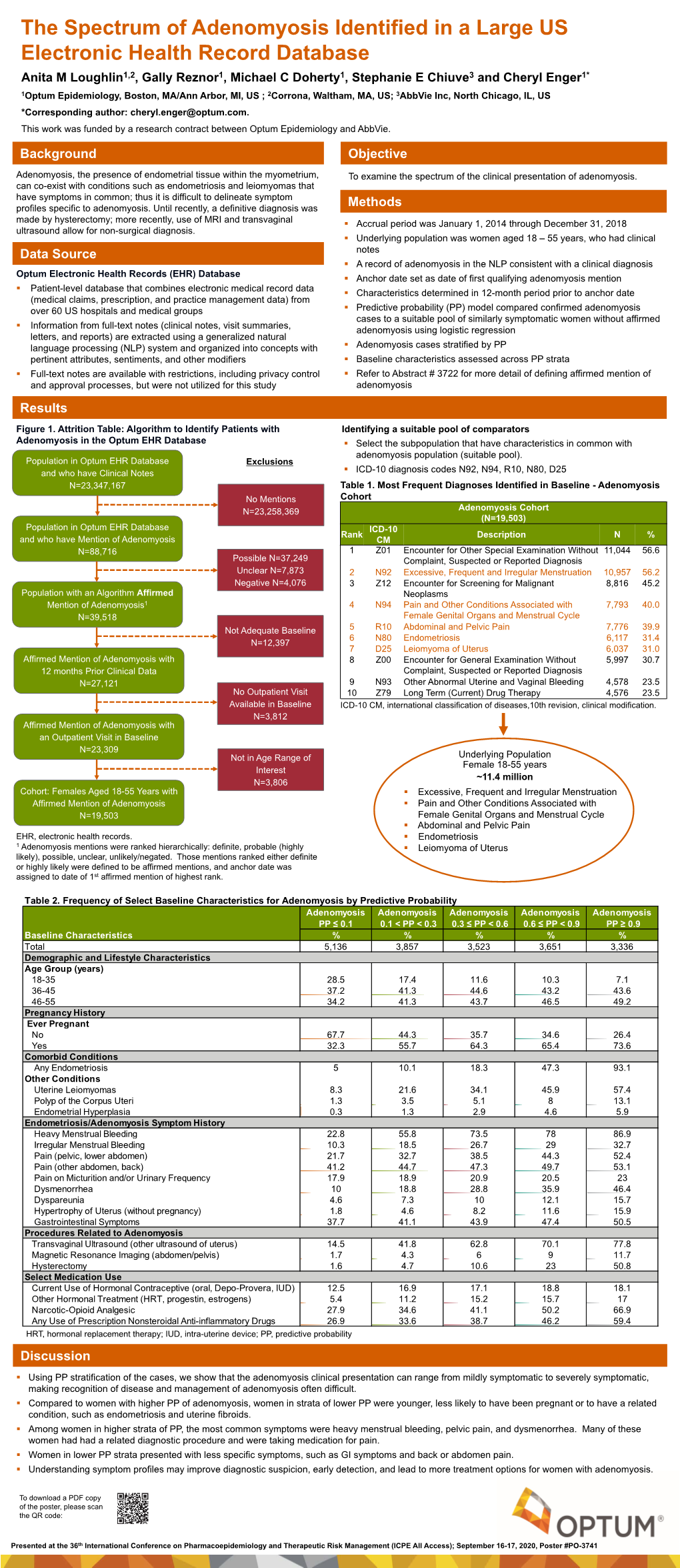
The Spectrum of Adenomyosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pelvic Inflammatory Disease -PID Examination and STI Screening
How do I get tested for PID? What about my partner? a guide to PID is diagnosed by a medical assessment/ As PID can be caused by a sexually transmitted Pelvic Inflammatory Disease -PID examination and STI screening. There is no one infection it is important that all current partners simple test. are tested for STIs and are treated with antibiotics You can still have PID even if your STI screen is too (even if their STI tests are negative). negative. Sometimes ex partners will need to be tested too If your doctor suspects PID you will be advised - you will be advised about this. to have a course of antibiotics. This is because the consequences of leaving PID untreated or not When can I have sex again? treating promptly (see below) can be serious. It’s best you don’t have sex at all (not even with a We also need to make sure you are not pregnant condom and not even any oral sex) until you and – please tell your doctor if you think you could be your partner have finished your antibiotics. pregnant. What happens if my PID is left untreated? How is PID treated? Untreated PID can cause serious problems: It is important to get treated quickly to reduce the Persistent or recurrent bouts of pelvic pain risk of complications. Infertility PID is treated with a mixture of antibiotics to cover An ectopic pregnancy (this is a serious condition the most likely infections. requiring urgent surgery) The treatment course is usually for 2 weeks. Pelvic abscess The treatment is free and issued to you directly in Persistent or recurrent bouts of pelvic or the clinic. -

Pelvic Inflammatory Disease (PID) PELVIC INFLAMMATORY DISEASE (PID)
Clinical Prevention Services Provincial STI Services 655 West 12th Avenue Vancouver, BC V5Z 4R4 Tel : 604.707.5600 Fax: 604.707.5604 www.bccdc.ca BCCDC Non-certified Practice Decision Support Tool Pelvic Inflammatory Disease (PID) PELVIC INFLAMMATORY DISEASE (PID) SCOPE RNs (including certified practice RNs) must refer to a physician (MD) or nurse practitioner (NP) for all clients who present with suspected PID as defined by pelvic tenderness and lower abdominal pain during the bimanual exam. ETIOLOGY Pelvic inflammatory disease (PID) is an infection of the upper genital tract that involves any combination of the uterus, endometrium, ovaries, fallopian tubes, pelvic peritoneum and adjacent tissues. PID consists of ascending infection from the lower-to-upper genital tract. Prompt diagnosis and treatment is essential to prevent long-term sequelae. Most cases of PID can be categorized as sexually transmitted and are associated with more than one organism or condition, including: Bacterial: Chlamydia trachomatis (CT) Neisseria gonorrhoeae (GC) Trichomonas vaginalis Mycoplasma genitalium bacterial vaginosis (BV)-related organisms (e.g., G. vaginalis) enteric bacteria (e.g., E. coli) (rare; more common in post-menopausal people) PID may be associated with no specific identifiable pathogen. EPIDEMIOLOGY PID is a significant public health problem. Up to 2/3 of cases go unrecognized, and under reporting is common. There are approximately 100,000 cases of symptomatic PID annually in Canada; however, PID is not a reportable infection so, exact -

Pelvic Inflammatory Disease (PID) Brown Health Services Patient Education Series
Pelvic Inflammatory Disease (PID) Brown Health Services Patient Education Series the uterine lining to treat abnormal What is PID? bleeding) PID (pelvic inflammatory disease) is ● PID risk from insertion of an IUD inflammation caused by infections ascending (intrauterine device) – occurs in the first 3 weeks post insertion from the vagina or cervix to the upper genital ● Abortion tract. This includes the lining of the uterus, the ovaries, the fallopian tubes, the uterine wall Why is it important to treat PID? and the uterine ligaments that hold these ● structures in place. PID is the most common serious infection of women aged 16 to 25 years What causes it? of age ● Untreated pelvic infections may cause Most cases of PID are caused by sexually adhesions in the fallopian tubes, which transmitted infections (STIs). The disease can be may lead to infertility caused by many different organisms or ● 1 in 4 women with acute PID develop combinations of organisms, but is frequently future problems such as ectopic caused by gonorrhea and chlamydia. Although pregnancy or chronic pelvic pain from Bacterial Vaginosis (BV) is associated with PID, adhesions whether the incidence of PID can be reduced by What are the symptoms? identifying and treating people with vaginas with BV is unclear. If you notice abnormal ● Painful intercourse could be the first discharge and a fishy vaginal odor (signs of BV) sign of infection ● you should be evaluated at Health Services. Pain and tenderness involving the lower abdomen, cervix, uterus and ovaries PID may also occur following procedures that ● Fever and chills create an open wound where infectious ● Nausea and/or diarrhea organisms can more easily enter, such as: ● Abnormal vaginal bleeding or discharge ● Biopsy from the lining of the uterus Early treatment can usually prevent these ● D & C (dilation and curettage – a problems. -

Endometriosis
www.pelvicpain.org All information, content, and material of this website / handout is for informational purposes only and are not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider. The information is not intended to recommend the self-management of health problems or wellness. It is not intended to endorse or recommend any particular type of medical treatment. Should the reader have any health care related questions, that person should promptly call or consult your physician or healthcare provider. This information should not be used by any reader to disregard medical and/or health related advice or provide a basis to delay consultation with a physician or a qualified healthcare provider. Endometriosis Endometriosis occurs when tissue that is similar to the lining of the uterus (endometrium) grows in other parts of the body and causes chronic inflammation that can cause scarring. It affects an estimated 5-10% of all women. It is most commonly found in the pelvic cavity and ovaries. Less commonly, these lesions may grow on the intestines and bladder, and rarely in the lungs or other body locations. Growths of endometriosis are almost always benign (not cancerous). Symptoms The most common symptom is pain in the pelvis, lower abdomen, or lower back. Pain is most often during the menstrual cycle, but women may have pain at other times. Not everyone with endometriosis has pain. Other symptoms include difficulty getting pregnant, pain during or after sex, pain with bowel movements or urination, constipation, diarrhea and bloating (often around the menstrual cycle). -

The Differential Diagnosis of Acute Pelvic Pain in Various Stages of The
Osteopathic Family Physician (2011) 3, 112-119 The differential diagnosis of acute pelvic pain in various stages of the life cycle of women and adolescents: gynecological challenges for the family physician in an outpatient setting Maria F. Daly, DO, FACOFP From Jackson Memorial Hospital, Miami, FL. KEYWORDS: Acute pain is of sudden onset, intense, sharp or severe cramping. It may be described as local or diffuse, Acute pain; and if corrected takes a short course. It is often associated with nausea, emesis, diaphoresis, and anxiety. Acute pelvic pain; It may vary in intensity of expression by a woman’s cultural worldview of communicating as well as Nonpelvic pain; her history of physical, mental, and psychosocial painful experiences. The primary care physician must Differential diagnosis dissect in an orderly, precise, and rapid manner the true history from the patient experiencing pain, and proceed to diagnose and treat the acute symptoms of a possible life-threatening problem. © 2011 Elsevier Inc. All rights reserved. Introduction female’s presentation of acute pelvic pain with an enlarged bulky uterus may often be diagnosed as a leiomyoma in- Women at various ages and stages of their life cycle may stead of a neoplastic mass. A pregnant female, whose preg- present with different causes of acute pelvic pain. Estab- nancy is either known to her or unknown, presenting with lishing an accurate diagnosis from the multiple pathologies acute pelvic pain must be rapidly evaluated and treated to in the differential diagnosis of their specific pelvic pain may prevent a rapid downward cascading progression to mater- well be a challenge for the primary care physician. -

Grading Pelvic Prolapse and Pelvic Floor Relaxation Using Dynamic Magnetic Resonance Imaging
ADULT UROLOGY GRADING PELVIC PROLAPSE AND PELVIC FLOOR RELAXATION USING DYNAMIC MAGNETIC RESONANCE IMAGING CRAIG V. COMITER, SANDIP P. VASAVADA, ZORAN L. BARBARIC, ANGELO E. GOUSSE, AND SHLOMO RAZ ABSTRACT Objectives. With significant vaginal prolapse, it is often difficult to differentiate among cystocele, enterocele, and high rectocele by physical examination alone. Our group has previously demonstrated the utility of magnetic resonance imaging (MRI) for evaluating pelvic prolapse. We describe a simple objective grading system for quantifying pelvic floor relaxation and prolapse. Methods. One hundred sixty-four consecutive women presenting with pelvic pain (n ϭ 39) or organ prolapse (n ϭ 125) underwent dynamic MRI. The “H-line” (levator hiatus) measures the distance from the pubis to the posterior anal canal. The “M-line” (muscular pelvic floor relaxation) measures the descent of the levator plate from the pubococcygeal line. The “O” classification (organ prolapse) characterizes the degree of visceral prolapse beyond the H-line. Results. The image acquisition time was 2.5 minutes per study. Each study cost $540. In the pain group, the H-line averaged 5.2 Ϯ 1.1 cm versus 7.5 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). The M-line averaged 1.9 Ϯ 1.2 cm in the pain group versus 4.1 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). Incidental pelvic pathologic features were commonly noted, including uterine fibroids, ovarian cysts, hydroureter, urethral diverticula, and foreign body. Conclusions. The HMO classification provides a straightforward and reproducible method for staging and quantifying pelvic floor relaxation and visceral prolapse. -

Heavy Menstrual Bleeding
25/06/2018 Definition • Heavy menstrual bleeding (HMB) is defined as excessive menstrual blood loss which interferes with a woman's physical, social, emotional and/or material quality of life. Heavy Menstrual Bleeding (HMB): Replaced ‘menorrhagia’ Objective definition of HMB >80mL/ cycle or duration of >7 days Causes and Management • It can occur alone or in combination with other symptoms (e.g. intermenstrual bleeding, pelvic pain, pressure symptoms) Dr. William (Wee-Liak) Hoo, MD MRCOG Consultant Gynaecologist Prevalence King’s College Hospital NHS FT • The prevalence of HMB in objective studies (9 to 14%) and subjective studies 20 to 52%) in studies based on subjective assessment. • In the UK, almost 1.5 million women consult their General Practitioners UKCPA Women’s Health Group Masterclass (GPs) each year with menstrual complaints and the annual treatment cost Friday 22nd June 2018 exceeds £65 million. Causes • Uterine: Uterine fibroids (dysmenorrhoea, palpable mass, pressure symptoms) Adenomyosis (dysmenorrhoea, subfertility) Endometrial polyps (intermenstrual bleeding) Pelvic inflammatory disease (PID)/ infection (vaginal discharge, pelvic pain, intermenstrual and postcoital bleeding and pyrexia) Malignancy or atypical hyperplasia (irregular/ postcoital/ intermenstrual bleeding, pelvic pain, weight loss). • Ovarian: Polycystic ovary syndrome (acne, hursuitism) • Systemic diseases: Hypothyroidism (fatigue, constipation, cold intolerance and hair and skin changes) Coagulation disorders (e.g. von Willebrand disease) Liver -

Guidelines on Chronic Pelvic Pain
GUIDELINES ON CHRONIC PELVIC PAIN (Limited text update April 2010) M. Fall (chairman), A.P. Baranowski, D. Engeler, S. Elneil, J. Hughes, E. J. Messelink, F. Oberpenning, A.C. de C. Williams Eur Urol 2004;46(6):681-9 Eur Urol 2010;57(1):35-48 Diagnosis and classification of CPP Chronic (also known as persistent) pain occurs for at least 3 months. It is associated with changes in the central nervous system (CNS) that may maintain the perception of pain in the absence of acute injury. These changes may also mag- nify perception so that non-painful stimuli are perceived as painful (allodynia) and painful stimuli become more painful than expected (hyperalgesia). Core muscles, e.g. pelvic mus- cles, may become hyperalgesic with multiple trigger points. Other organs may also become sensitive, e.g. the uterus with dyspareunia and dysmenorrhoea, or the bowel with irritable bowel symptoms. The changes within the CNS occur throughout the whole neuroaxis and as well as sensory changes result in both func- tional changes (e.g. irritable bowel symptoms) and structural changes (e.g. neurogenic oedema in some bladder pain syn- dromes). Central changes may also be responsible for some of the psychological consequences, which also modify pain mechanisms in their own right. 262 Chronic Pelvic Pain Basic investigations are carried out to exclude ‘well- defined’ pathologies. Negative results mean a ‘well-defined’ pathology is unlikely. Any further investigations are only done for specific indications, e.g. subdivision of a pain syn- drome. The EAU guidelines avoid spurious diagnostic terms, which are associated with inappropriate investigations, treatments and patient expectations and, ultimately, a worse prognostic outlook. -

Postoperative Adhesions in Gynecologic Surgery: a Committee Opinion
ASRM PAGES Postoperative adhesions in gynecologic surgery: a committee opinion Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society of Reproductive Surgeons American Society for Reproductive Medicine, Birmingham, Alabama Postoperative adhesions are a natural consequence of surgical tissue trauma and healing and may result in infertility, pain, and bowel obstruction. Adherence to microsurgical principles and minimally invasive surgery may help to decrease postoperative adhesions. Some surgical barriers have been demonstrated to be effective for reducing postoperative adhesions, but there is no substantial evidence that their use improves fertility, decreases pain, or reduces the incidence of postoperative bowel obstruction. This document replaces the document, ‘‘Pathogenesis, consequences, and control of peritoneal adhesions in gynecologic surgery: a committee opinion,’’ last pub- lished in 2013. (Fertil SterilÒ 2019;112:458–63. Ó2019 by American Society for Reproductive Medicine.) Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/users/16110-fertility- and-sterility/posts/50136-28463 INTRODUCTION Health Service hospitals and helped to dian women admitted to the hospital fi Postoperative adhesions are a natural de ne the epidemiology and impact of with a diagnosis of small-bowel consequence of surgical tissue trauma postoperative adhesions (1, 2). Overall, obstruction after gynecologic proced- and healing. Peritoneal adhesions may approximately one third of patients ures found that hysterectomy was a sig- fi result in infertility, pain, or bowel who underwent open abdominal or ni cant cause of adhesion-related obstruction and may increase the tech- pelvic surgery were readmitted an small-bowel obstruction and that lapa- nical difficulty of subsequent abdom- average of 2 times over the subsequent roscopic supracervical hysterectomy inal or pelvic surgery. -

Irritable Bowel Syndrome and Endometriosis: Twins in Disguise
Review Irritable Bowel Syndrome and Endometriosis: Twins in Disguise Meredith Aragon, MD, MPH, and Bruce A. Lessey, MD, PhD From the Department of OB/GYN, Greenville Health System, Greenville, SC (M.A., B.A.L.) hronic pelvic pain (CPP) is a debilitating, IBS patients incur higher annual healthcare costs lifelong struggle for some individuals. compared to those without IBS,11 with spending C The diagnosis and treatment of CPP also ranging from $1562 to $7547 per year for the contribute to significant annual healthcare costs average IBS patient. Annually, IBS is estimated in the United States (US).1 The most common to result in $1.6 billion in direct costs and $19.2 diagnoses associated with CPP include endo- billion in indirect costs in the US alone. metriosis, interstitial cystitis, irritable bowel syndrome (IBS), myofascial pain, pelvic floor It can be argued that IBS is a constellation of hypertonia, and dysmenorrhea.2,3 In reality, CPP symptoms that includes bloating, diarrhea, con- in women often represents undiagnosed endo- stipation, and varied other bowel complaints, metriosis that may contribute to these other rather than a defined disease.12,13 In general, associated pain syndromes. Since a diagnosis of gastroenterologists (GIs) and others specializ- endometriosis requires surgery, there is a delay ing in gastroenterology complaints are largely in the diagnosis of endometriosis of greater than unaware of the strong links between IBS and 11 years in the US.4,5 endometriosis; therefore, it is rarely included in the differential diagnosis for bowel complaints. For some practitioners, symptoms including This fact may contribute to the poor satisfac- bowel, bladder, and pelvic complaints are recog- tion of patients with current IBS treatments. -

Chronic Pelvic Pain D
Guidelines on Chronic Pelvic Pain D. Engeler (Chair), A.P. Baranowski, J. Borovicka, A. Cottrell (Guidelines Associate), P. Dinis-Oliveira, S. Elneil, J. Hughes, E.J. Messelink (Vice-chair), A. van Ophoven, Y. Reisman, A.C. de C Williams © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 Aim 6 1.1.1 Structure and scope 6 1.2 Publication history 6 1.3 Panel composition 7 1.4 Methods 7 2. CHRONIC PELVIC PAIN 8 2.1 Introduction to chronic urogenital pain syndromes 8 2.2 Pain mechanisms - pain as a disease process 8 2.2.1 Ongoing peripheral visceral pain mechanisms as a cause of CPP 9 2.2.2 Central sensitisation - spinal and higher mechanisms of visceral pain 9 2.2.3 Spinal mechanisms and visceral hyperalgesia 9 2.2.4 Supraspinal modulation of pain perception 10 2.2.5 Higher centre modulation of spinal nociceptive pathways 10 2.2.6 Neuromodulation and psychology 10 2.2.7 Autonomic nervous system 10 2.2.8 Endocrine system 10 2.2.9 Genetics and chronic pain 10 2.3 Clinical paradigms and CPP 11 2.3.1 Referred pain 11 2.3.2 Referred pain to somatic tissues with hyperalgesia in the somatic tissues 11 2.3.3 Muscles and pelvic pain 11 2.3.4 Visceral hyperalgesia 11 2.3.5 Viscero-visceral hyperalgesia 11 2.4 Classification of CPP syndromes 12 2.4.1 Importance of classification 12 2.4.2 Pain syndromes 14 2.4.2.1 Definition of chronic pelvic pain (CPP) 14 2.4.2.2 Definition of chronic pelvic pain syndrome 14 2.4.2.2.1 Further subdivision of CPPS 14 2.4.2.2.2 Psychological considerations for classification 14 2.4.2.2.3 Functional considerations for classification 15 2.5.2.2.4 Multisystem subdivision 15 2.4.2.2.5 Dyspareunia 15 2.4.2.2.6 Perineal pain syndrome 15 2.5 Conclusions and recommendations: CPP and mechanisms 15 2.6 An algorithm for CPP diagnosis and treatment 16 3. -
Management of Adenomyosis a Review of Characteristic Imaging Findings and Treatment Options, with an Emphasis on the Use of Uterine Artery Embolization
WOMEN’S HEALTH Management of Adenomyosis A review of characteristic imaging findings and treatment options, with an emphasis on the use of uterine artery embolization. BY THERESA M. CARIDI, MD, AND JAMES B. SPIES, MD, MPH denomyosis is defined as ectopic endometrial tis- myosis on MRI include thickening of the junctional sue within the musculature of the uterus.1 It is a zone exceeding 12 mm and high-signal-intensity foci challenging condition in that it often overlaps in on T2/T1-weighted images similar to the case shown in symptoms and is found in conjunction with other Figure 1.4 Many studies have evaluated the diagnostic Agynecologic disorders, including endometriosis and uterine accuracy of TVUS and MRI techniques for adenomyosis. leiomyoma (fibroids).2 The typical clinical manifestations TVUS has a sensitivity of approximately 72% and speci- of adenomyosis occur in women who are 40 to 50 years of ficity of 81% versus 77% and 89% for MRI, respectively.8 age and include abnormal uterine bleeding and dysmenor- In addition, MRI can provide greater detail about the rhea (65% of patients).1 The exact pathogenesis is not fully extent of disease and additional uterine lesions, as well defined but is thought to be the result of direct invagina- as information about the less common presentation of tion of the endometrium into the myometrium.3 The adenomyosis, where focal disease in the form of an ade- interventionalist’s role is to offer uterine artery emboliza- nomyoma is present rather than the more typical diffuse tion (UAE), which provides some benefits over traditional adenomyosis findings.