Synthetic, Natural, and Semisynthetic Polymer Carriers for Controlled Nitric Oxide Release in Dermal Applications: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Biology of Nitric Oxide, Part 7
Cell Death and Differentiation (2001) 8, 106 ± 108 ã 2001 Nature Publishing Group All rights reserved 1350-9047/01 $15.00 www.nature.com/cdd Book Review The Biology of Nitric Oxide, Part 7 B BruÈne University of Erlangen-NuÈrnberg, Medical Department IV, Experimental Division, Loschgestrasse 8, 91054 Erlangen, Germany The Biology of Nitric Oxide Part 7. Edited by S Moncada, LE Gustafsson, NP Wiklund, EA Higgs, Portland Press, London, UK: 2000, Pp. 234, £110, ISBN: 1 85578 142 5 This book is in the tradition of previously related titles (The covered by this book are quite extensive and an up-to-date Biology of Nitric Oxide, Parts 1 ± 6) that cover cutting edge summary of the current status of the field is provided. This scientific contribution related to the chemistry, biology, and is excellent for insiders, looking for detailed information, medicine of nitric oxide. Ten years after the initiating new cross-links, or just being interested in the current conference on a series of NO conventions, which was held research focus of individual groups. In this respect, most of in London in September 1989, this book now summarizes the chapters are well organized, providing background about 35 oral communications and approximately 300 poster information, technical comments, results, and a brief presentations of the 6th International Meeting on the Biology discussion. In most papers, figures or tables illustrate of Nitric Oxide, which was organized in September 1999 in major findings and references provide information for more Stockholm, Sweden. With the editors, especially Professor advanced reading on a particular topic. At the same time, Dr. -

A Biochemical Rationale for the Discrete Behavior of Nitroxyl and Nitric Oxide in the Cardiovascular System
A biochemical rationale for the discrete behavior of nitroxyl and nitric oxide in the cardiovascular system Katrina M. Miranda*†‡, Nazareno Paolocci§, Tatsuo Katori§, Douglas D. Thomas*, Eleonora Ford¶, Michael D. Bartbergerʈ, Michael G. Espey*, David A. Kass§, Martin Feelisch**, Jon M. Fukuto¶, and David A. Wink*† *Radiation Biology Branch, Building 10, Room B3-B69, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892; §Division of Cardiology, Department of Medicine, The Johns Hopkins Medical Institutions, Baltimore, MD 21287; ¶Department of Molecular and Medical Pharmacology, Center for the Health Sciences, University of California, Los Angeles, CA 90095; ʈDepartment of Chemistry and Biochemistry, University of California, Los Angeles, CA 90095; and **Department of Molecular and Cellular Physiology, Louisiana State University Health Sciences Center, Shreveport, LA 71130 Edited by Louis J. Ignarro, University of California School of Medicine, Los Angeles, CA, and approved May 20, 2003 (received for review February 20, 2003) The redox siblings nitroxyl (HNO) and nitric oxide (NO) have often cellular thiol functions (14, 15). Conversely, NO reacts only indi- been assumed to undergo casual redox reactions in biological sys- rectly with thiols after RNOS formation (17). tems. However, several recent studies have demonstrated distinct Contrasting effects are also apparent in vivo or ex vivo,for pharmacological effects for donors of these two species. Here, infu- example in models of ischemia reperfusion injury. Exposure to NO sion of the HNO donor Angeli’s salt into normal dogs resulted in donors at the onset of reperfusion provides protection against elevated plasma levels of calcitonin gene-related peptide, whereas reperfusion injury in the heart and other organs (18–20). -

Novel Antagonists for the Human Adenosine
UvA-DARE (Digital Academic Repository) Novel antagonists for the human adenosine A2A and A3 receptor via purine nitration: synthesis and biological evaluation of C2-substituted 6- trifluoromethylpurines and 1-deazapurines Koch, M. Publication date 2011 Document Version Final published version Link to publication Citation for published version (APA): Koch, M. (2011). Novel antagonists for the human adenosine A2A and A3 receptor via purine nitration: synthesis and biological evaluation of C2-substituted 6-trifluoromethylpurines and 1- deazapurines. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:05 Oct 2021 Novel antagonists for the human adenosine A Novel antagonists for the human adenosine Uitnodiging Novel antagonists for the voor het bijwonen van human adenosine de openbare verdediging van het proefschrift van A2A and A3 receptor via purine nitration Melle Koch op vrijdag 21 oktober 2011 om 14:00 uur in de Agnietenkapel van de Universiteit van Amsterdam Synthesis and biological evaluation Oudezijds Voorburgwal 231 of C2-substituted te Amsterdam 2A Na afloop van de promotie and A 6-trifluoromethylpurines zal hier tevens de receptie . -

Nitric Oxide in Health and Disease of the Nervous System H-Y Yun1,2, VL Dawson1,3,4 and TM Dawson1,3
Molecular Psychiatry (1997) 2, 300–310 1997 Stockton Press All rights reserved 1359–4184/97 $12.00 PROGRESS Nitric oxide in health and disease of the nervous system H-Y Yun1,2, VL Dawson1,3,4 and TM Dawson1,3 Departments of 1Neurology; 3Neuroscience; 4Physiology, Johns Hopkins University School of Medicine, Baltimore, MD, USA Nitric oxide (NO) is a widespread and multifunctional biological messenger molecule. It mediates vasodilation of blood vessels, host defence against infectious agents and tumors, and neurotransmission of the central and peripheral nervous systems. In the nervous system, NO is generated by three nitric oxide synthase (NOS) isoforms (neuronal, endothelial and immunologic NOS). Endothelial NOS and neuronal NOS are constitutively expressed and acti- vated by elevated intracellular calcium, whereas immunologic NOS is inducible with new RNA and protein synthesis upon immune stimulation. Neuronal NOS can be transcriptionally induced under conditions such as neuronal development and injury. NO may play a role not only in physiologic neuronal functions such as neurotransmitter release, neural development, regeneration, synaptic plasticity and regulation of gene expression but also in a variety of neurological disorders in which excessive production of NO leads to neural injury. Keywords: nitric oxide synthase; endothelium-derived relaxing factor; neurotransmission; neurotoxic- ity; neurological diseases Nitric oxide is probably the smallest and most versatile NO synthases isoforms and regulation of NO bioactive molecule identified. Convergence of multi- generation disciplinary efforts in the field of immunology, cardio- vascular pharmacology, chemistry, toxicology and neu- NO is formed by the enzymatic conversion of the guan- robiology led to the revolutionary novel concept of NO idino nitrogen of l-arginine by NO synthase (NOS). -
Meat Curing and Sodium Nitrite
MEDIA MYTHCRUSHER Meat Curing and Sodium Nitrite The use of nitrite to produce cured meats like salami, ham, bacon and hot dogs, is a safe, regulated practice that has distinct public health benefits. However, much confusion and even mythology surrounds nitrite. Being mindful of key words and statistics and providing appropriate context can help reporters improve the accuracy of their coverage and the information that is passed on to readers and viewers. We’ve compiled ten tips to improve accuracy when writing about the use of sodium nitrite in cured meats. #1: Nitrite is not ‘unnatural’. Before the terms nitrate and nitrite are often used refrigeration was available, humans salted and interchangeably, meat companies mainly use dried meat to preserve it. It was discovered sodium nitrite to cure meat, not sodium nitrate. that the nitrate in saltpeter was extremely At the turn of the 20th century, German effective in causing a chemical reaction known scientists discovered nitrite (and not nitrate) as “curing.” Not only did this give meat a was the active form of these curing salts. When distinct taste and flavor, it also preserved it and added directly, rather than as nitrate, meat prevented the growth of Clostridium botulinum, processors can have better control of this which causes botulism. important curing ingredient and more closely manage how much they are adding. Later on, scientists came to understand that nitrate naturally found in the environment #3: Cured meats are a miniscule source of converts to nitrite when in the presence of total human nitrite intake. Scientists say that certain bacteria. -

Inhibition of Grb2‑Mediated Activation of MAPK Signal Transduction
566 ONCOLOGY LETTERS 4: 566-570, 2012 Inhibition of Grb2‑mediated activation of MAPK signal transduction suppresses NOR1/CB1954‑induced cytotoxicity in the HepG2 cell line RONG GUI1, DENGQING LI1, GUANNAN QI1,2, ALI SUHAD2 and XINMIN NIE1 1Clinical Laboratory Centre of the Third Xiangya Hospital, Central South University, Changsha, Hunan 410013, P.R. China; 2Hormones and Cancer Research Unit, Royal Victoria Hospital, McGill University, Quebec H3A 1A1, Canada Received March 12, 2012; Accepted June 22, 2012 DOI: 10.3892/ol.2012.774 Abstract. The nitroreductase oxidored-nitro domain Introduction containing protein 1 (NOR1) gene may be involved in the chemical carcinogenesis of hepatic cancer and nasopharyn- The oxidored-nitro domain containing protein 1 (NOR1) gene geal carcinoma (NPC). We have previously demonstrated that was previously cloned in our laboratory at the Third Xiangya NOR1 overexpression is capable of converting the monofunc- Hospital (Hunan, China) using suppression subtractive hybrid- tional alkylating agent 5-(aziridin-1-yl)-2,4-dinitrobenzamide ization and cDNA microarrays (1,2). By examining the human (CB1954) into a toxic form by reducing the 4-nitro group of genome working sequence, it has been identified that that the CB1954. Toxic CB1954 is able to enhance cell killing in the NOR1 gene is located on 1p34.3 and contains 10 exons and NPC cell line CNE1; however, the underlying mechanisms 9 introns. Additionally, the PROSITE database identified remain unknown. Using cDNA microarrays and quantitative two possible cAMP and cGMP-dependent protein kinase real-time PCR, we previously discovered that NOR1 increases phosphorylation sites, two tyrosine phosphorylation sites the expression of growth factor receptor-bound protein 2 and four N-myristoylation sites in NOR1. -

Role of Sodium/Calcium Exchangers in Tumors
biomolecules Review Role of Sodium/Calcium Exchangers in Tumors Barbora Chovancova 1, Veronika Liskova 1, Petr Babula 2 and Olga Krizanova 1,2,* 1 Institute of Clinical and Translational Research, Biomedical Research Center, Slovak Academy of Sciences, Dubravska cesta 9, 845 45 Bratislava, Slovakia; [email protected] (B.C.); [email protected] (V.L.) 2 Department of Physiology, Faculty of Medicine, Masaryk University, Kamenice 753/5, 625 00 Brno, Czech Republic; [email protected] * Correspondence: [email protected]; Tel.: +4212-3229-5312 Received: 6 August 2020; Accepted: 29 August 2020; Published: 31 August 2020 Abstract: The sodium/calcium exchanger (NCX) is a unique calcium transport system, generally transporting calcium ions out of the cell in exchange for sodium ions. Nevertheless, under special conditions this transporter can also work in a reverse mode, in which direction of the ion transport is inverted—calcium ions are transported inside the cell and sodium ions are transported out of the cell. To date, three isoforms of the NCX have been identified and characterized in humans. Majority of information about the NCX function comes from isoform 1 (NCX1). Although knowledge about NCX function has evolved rapidly in recent years, little is known about these transport systems in cancer cells. This review aims to summarize current knowledge about NCX functions in individual types of cancer cells. Keywords: sodium-calcium exchanger; cancer cells; calcium; apoptosis 1. Background Intracellular calcium ions are considered the most abundant secondary messengers in human cells, since they have a substantial diversity of roles in fundamental cellular physiology. Accumulating evidence has demonstrated that intracellular calcium homeostasis is altered in cancer cells and that this alteration is involved in tumor initiation, angiogenesis, progression and metastasis. -

Acute Exposure Guideline Levels for Selected Airborne Chemicals: Volume 11
This PDF is available from The National Academies Press at http://www.nap.edu/catalog.php?record_id=13374 Acute Exposure Guideline Levels for Selected Airborne Chemicals: Volume 11 ISBN Committee on Acute Exposure Guideline Levels; Committee on 978-0-309-25481-6 Toxicology; National Research Council 356 pages 6 x 9 PAPERBACK (2012) Visit the National Academies Press online and register for... Instant access to free PDF downloads of titles from the NATIONAL ACADEMY OF SCIENCES NATIONAL ACADEMY OF ENGINEERING INSTITUTE OF MEDICINE NATIONAL RESEARCH COUNCIL 10% off print titles Custom notification of new releases in your field of interest Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Request reprint permission for this book Copyright © National Academy of Sciences. All rights reserved. Acute Exposure Guideline Levels for Selected Airborne Chemicals: Volume 11 Committee on Acute Exposure Guideline Levels Committee on Toxicology Board on Environmental Studies and Toxicology Division on Earth and Life Studies Copyright © National Academy of Sciences. All rights reserved. Acute Exposure Guideline Levels for Selected Airborne Chemicals: Volume 11 THE NATIONAL ACADEMIES PRESS 500 FIFTH STREET, NW WASHINGTON, DC 20001 NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the National Academy of Sciences, the National Academy of Engineering, and the Insti- tute of Medicine. The members of the committee responsible for the report were chosen for their special competences and with regard for appropriate balance. -
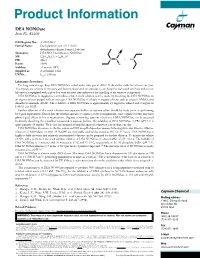
Download Product Insert (PDF)
Product Information DEA NONOate Item No. 82100 CAS Registry No.: 372965-00-9 Formal Name: Diethylammonium (Z)-1-(N,N- diethylamino)diazen-1-ium-1,2-diolate O Synonyms: DEA/NO, Diethylamine NONOate N MF: C4H10N3O2 • C4H12N + N N • H N FW: 206.3 2 Purity: ≥98% O- Stability: ≥1 year at -80°C Supplied as: A crystalline solid l UV/Vis.: max: 250 nm Laboratory Procedures For long term storage, keep DEA NONOate sealed under nitrogen at -80°C. It should be stable for at least one year. The crystals are sensitive to moisture and become discolored on exposure to air. Keep the vial sealed until use unless your laboratory is equipped with a glove box with an inert atmosphere for the handling of air sensitive compounds. DEA NONOate is supplied as a crystalline solid. A stock solution may be made by dissolving the DEA NONOate in an organic solvent purged with an inert gas. DEA NONOate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of DEA NONOate is approximately 25 mg/ml in ethanol and 2 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of DEA NONOate can be prepared by directly dissolving the crystalline compound in aqueous buffers. The solubility of DEA NONOate in PBS (pH 7.2) is approximately 10 mg/ml. -

Exisulind, a Novel Proapoptotic Drug, Inhibits Rat Urinary Bladder Tumorigenesis1
[CANCER RESEARCH 61, 3961–3968, May 15, 2001] Exisulind, a Novel Proapoptotic Drug, Inhibits Rat Urinary Bladder Tumorigenesis1 Gary A. Piazza, W. Joseph Thompson,2 Rifat Pamukcu, Hector W. Alila, Clark M. Whitehead, Li Liu, John R. Fetter, William E. Gresh, Jr., Andres J. Klein-Szanto, Daniel R. Farnell, Isao Eto, and Clinton J. Grubbs Cell Pathways, Inc., Horsham, Pennsylvania 19044 [G. A. P., W. J. T., R. P., H. W. A., C. M. W., L. L., J. R. F., W. E. G.]; Fox Chase Cancer Center, Philadelphia, Pennsylvania 19111 [A. J. K.]; Southern Research Institute, Birmingham, Alabama 35205 [D. R. F.]; and The University of Alabama at Birmingham, Birmingham, Alabama 35205-7340 [I. E., C. J. G.] ABSTRACT systemic or intravesical delivery of chemotherapeutic drugs, which produce relatively modest efficacy and are associated with serious Exisulind (Aptosyn) is a novel antineoplastic drug being developed for side effects and/or delivery complications. The high rate of mortality the prevention and treatment of precancerous and malignant diseases. In from urinary bladder cancer and the high incidence of disease recur- colon tumor cells, the drug induces apoptosis by a mechanism involving cyclic GMP (cGMP) phosphodiesterase inhibition, sustained elevation of rence emphasize the need for new therapeutic agents alone or in cGMP, and protein kinase G activation. We studied the effect of exisulind combination with existing therapies. Research to identify the specific on bladder tumorigenesis induced in rats by the carcinogen, N-butyl-N- molecular defects involved in bladder tumorigenesis has identified (4-hydroxybutyl) nitrosamine. Exisulind at doses of 800, 1000, and 1200 mutations in a number of genes (i.e., ras and p53) or altered expres- mg/kg (diet) inhibited tumor multiplicity by 36, 47, and 64% and tumor sion of proteins (cyclin D and p21 WAF1/CIP1), which are known to incidence by 31, 38, and 61%, respectively. -

Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics
Review Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics Joel Mintz 1,†, Anastasia Vedenko 2,†, Omar Rosete 3 , Khushi Shah 4, Gabriella Goldstein 5 , Joshua M. Hare 2,6,7 , Ranjith Ramasamy 3,6,* and Himanshu Arora 2,3,6,* 1 Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Davie, FL 33328, USA; [email protected] 2 John P Hussman Institute for Human Genomics, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] (A.V.); [email protected] (J.M.H.) 3 Department of Urology, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] 4 College of Arts and Sciences, University of Miami, Miami, FL 33146, USA; [email protected] 5 College of Health Professions and Sciences, University of Central Florida, Orlando, FL 32816, USA; [email protected] 6 The Interdisciplinary Stem Cell Institute, Miller School of Medicine, University of Miami, Miami, FL 33136, USA 7 Department of Medicine, Cardiology Division, Miller School of Medicine, University of Miami, Miami, FL 33136, USA * Correspondence: [email protected] (R.R.); [email protected] (H.A.) † These authors contributed equally to this work. Abstract: Nitric oxide (NO) is a short-lived, ubiquitous signaling molecule that affects numerous critical functions in the body. There are markedly conflicting findings in the literature regarding the bimodal effects of NO in carcinogenesis and tumor progression, which has important consequences for treatment. Several preclinical and clinical studies have suggested that both pro- and antitumori- Citation: Mintz, J.; Vedenko, A.; genic effects of NO depend on multiple aspects, including, but not limited to, tissue of generation, the Rosete, O.; Shah, K.; Goldstein, G.; level of production, the oxidative/reductive (redox) environment in which this radical is generated, Hare, J.M; Ramasamy, R.; Arora, H. -

Antiproliferative Effects of Carbon Monoxide on Pancreatic Cancer
Digestive and Liver Disease 46 (2014) 369–375 Contents lists available at ScienceDirect Digestive and Liver Disease jou rnal homepage: www.elsevier.com/locate/dld Oncology Antiproliferative effects of carbon monoxide on pancreatic cancer a,b,∗ c,1 a a Libor Vítek , Helena Gbelcová , Lucie Muchová , Katerinaˇ Vánovᡠ, a,2 a a a Jaroslav Zelenka , Renata Koníckovᡠ, Jakub Sukˇ , Marie Zadinova , c d,e d d,e c,∗∗ Zdenekˇ Knejzlík , Shakil Ahmad , Takeshi Fujisawa , Asif Ahmed , Tomásˇ Ruml a Institute of Medical Biochemistry and Laboratory Diagnostics, 1st Faculty of Medicine, Charles University in Prague, Prague 2, Czech Republic b 4th Department of Internal Medicine, 1st Faculty of Medicine, Charles University in Prague, Prague 2, Czech Republic c Department of Biochemistry and Microbiology, Institute of Chemical Technology, Prague 6, Czech Republic d Queen’s Medical Research Institute, University of Edinburgh, Edinburgh, UK e School of Life & Health Sciences, Aston University, Birmingham, UK a r t i c l e i n f o a b s t r a c t Article history: Background: Carbon monoxide, the gaseous product of heme oxygenase, is a signalling molecule with Received 14 June 2013 a broad spectrum of biological activities. The aim of this study was to investigate the effects of carbon Accepted 4 December 2013 monoxide on proliferation of human pancreatic cancer. Available online 14 January 2014 Methods: In vitro studies were performed on human pancreatic cancer cells (CAPAN-2, BxPc3, and PaTu- 8902) treated with a carbon monoxide-releasing molecule or its inactive counterpart, or exposed to Keywords: carbon monoxide gas (500 ppm/24 h).