Gut-Pancreas-Liver Axis As a Target for Treatment of NAFLD/NASH
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bile Acid Receptor Farnesoid X Receptor: a Novel Therapeutic Target for Metabolic Diseases
Review J Lipid Atheroscler 2017 June;6(1):1-7 https://doi.org/10.12997/jla.2017.6.1.1 JLA pISSN 2287-2892 • eISSN 2288-2561 Bile Acid Receptor Farnesoid X Receptor: A Novel Therapeutic Target for Metabolic Diseases Sungsoon Fang Severance Biomedical Science Institute, BK21 PLUS project for Medical Science, Yonsei University College of Medicine, Seoul, Korea Bile acid has been well known to serve as a hormone in regulating transcriptional activity of Farnesoid X receptor (FXR), an endogenous bile acid nuclear receptor. Moreover, bile acid regulates diverse biological processes, including cholesterol/bile acid metabolism, glucose/lipid metabolism and energy expenditure. Alteration of bile acid metabolism has been revealed in type II diabetic (T2D) patients. FXR-mediated bile acid signaling has been reported to play key roles in improving metabolic parameters in vertical sleeve gastrectomy surgery, implying that FXR is an essential modulator in the metabolic homeostasis. Using a genetic mouse model, intestinal specific FXR-null mice have been reported to be resistant to diet-induced obesity and insulin resistance. Moreover, intestinal specific FXR agonism using gut-specific FXR synthetic agonist has been shown to enhance thermogenesis in brown adipose tissue and browning in white adipose tissue to increase energy expenditure, leading to reduced body weight gain and improved insulin resistance. Altogether, FXR is a potent therapeutic target for the treatment of metabolic diseases. (J Lipid Atheroscler 2017 June;6(1):1-7) Key Words: Bile acids, Farnesoid X receptor, Metabolic diseases INTRODUCTION of endogenous bile acid nuclear receptor FXR proposes new perspectives to understand molecular mechanisms Bile acids are converted from cholesterol in the liver and physiological roles of bile acids and their receptors by numerous cytochrome P450 enzymes, including in various tissues to maintain whole body homeostasis. -

Gut Health in Veterinary Medicine: a Bibliometric Analysis of the Literature
animals Article Gut Health in Veterinary Medicine: A Bibliometric Analysis of the Literature Elena Colombino 1,*,† , Daniel Prieto-Botella 2,† and Maria Teresa Capucchio 1 1 Department of Veterinary Sciences, University of Turin, 10095 Grugliasco, Italy; [email protected] 2 Department of Surgery and Pathology, Miguel Hernandez University, 03550 Alicante, Spain; [email protected] * Correspondence: [email protected] † Equally contribution. Simple Summary: Gut health has been a main topic in veterinary medicine research after the ban on the use of antimicrobial growth promoters. Gut health has been defined as absence/prevention/avoidance of gastrointestinal disease so that the animal is able to perform its physiological functions. A biblio- metric analysis is a set of statistical methods used to explore trends in the scientific literature such as number of publications, most prolific countries and main research areas to highlight publication dynamics and gaps of knowledge. In this case, a bibliometric analysis was performed on veterinary gut health using the database Web of Science and the R package Bibliometrix. A total of 1696 docu- ments were retrieved between 2000 and 2020, showing an increase of 22.4% in the number of annual publications. Pigs (34.8%), poultry (chicken, duck, turkey and quail—33.9%) and aquaculture (fishes, crustaceans and frog—15.0%) were the most studied species while a scarce number of publications was found on felines, cows, horses, rodents, goats and sheep. China (24.7%), USA (17.2%) and Canada (5.7%) were the most productive countries. Three main research lines aimed to explore animal nutrition, prevention of inflammatory diseases and microbiota composition were identified. -

Obeticholic Acid and INT-767 Modulate Collagen Deposition in a NASH in Vitro Model Beatrice Anfuso 1, Claudio Tiribelli 1, Luciano Adorini2 & Natalia Rosso 1*
www.nature.com/scientificreports OPEN Obeticholic acid and INT-767 modulate collagen deposition in a NASH in vitro model Beatrice Anfuso 1, Claudio Tiribelli 1, Luciano Adorini2 & Natalia Rosso 1* Pharmacological treatments for non-alcoholic steatohepatitis (NASH) are still unsatisfactory. Fibrosis is the most signifcant predictor of mortality and many anti-fbrotic agents are under evaluation. Herein, we assessed in vitro the efects of the FXR agonist obeticholic acid (OCA) and the dual FXR/TGR5 agonist INT-767 in a well-established co-culture NASH model. Co-cultures of human hepatoma and hepatic stellate (HSCs) cells were exposed to free fatty acids (FFAs) alone or in combination with OCA or INT-767. mRNA expression of HSCs activation markers and FXR engagement were evaluated at 24, 96 and 144 hours. Collagen deposition and metalloproteinase 2 and 9 (MMP2-9) activity were compared to tropifexor and selonsertib. FFAs induced collagen deposition and MMP2-9 activity reduction. Co- treatment with OCA or INT-767 did not afect ACTA2 and COL1A1 expression, but signifcantly reduced FXR and induced SHP expression, as expected. OCA induced a dose-dependent reduction of collagen and induced MMP2-9 activity. Similarly, INT-767 induced collagen reduction at 96 h and a slight increase in MMP2-9. Tropifexor and Selonsertib were also efective in collagen reduction but showed no modulation of MMP2-9. All tested compounds reduced collagen deposition. OCA exerted a more potent and long-lasting efect, mainly related to modulation of collagen turn-over and MMP2-9 activity. Obesity prevalence is booming in both hig- and low-income countries has led to a surge in non-alcoholic fatty liver disease (NAFLD), a condition characterized by liver steatosis. -

Role of Bile Acids in the Regulation of Food Intake, and Their Dysregulation in Metabolic Disease
nutrients Review Role of Bile Acids in the Regulation of Food Intake, and Their Dysregulation in Metabolic Disease Cong Xie 1,† , Weikun Huang 1,2,† , Richard L. Young 1,3 , Karen L. Jones 1,4 , Michael Horowitz 1,4, Christopher K. Rayner 1,5 and Tongzhi Wu 1,4,6,* 1 Adelaide Medical School, Center of Research Excellence (CRE) in Translating Nutritional Science to Good Health, The University of Adelaide, Adelaide 5005, Australia; [email protected] (C.X.); [email protected] (W.H.); [email protected] (R.L.Y.); [email protected] (K.L.J.); [email protected] (M.H.); [email protected] (C.K.R.) 2 The ARC Center of Excellence for Nanoscale BioPhotonics, Institute for Photonics and Advanced Sensing, School of Physical Sciences, The University of Adelaide, Adelaide 5005, Australia 3 Nutrition, Diabetes & Gut Health, Lifelong Health Theme South Australian Health & Medical Research Institute, Adelaide 5005, Australia 4 Endocrine and Metabolic Unit, Royal Adelaide Hospital, Adelaide 5005, Australia 5 Department of Gastroenterology and Hepatology, Royal Adelaide Hospital, Adelaide 5005, Australia 6 Institute of Diabetes, School of Medicine, Southeast University, Nanjing 210009, China * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Bile acids are cholesterol-derived metabolites with a well-established role in the digestion and absorption of dietary fat. More recently, the discovery of bile acids as natural ligands for the nuclear farnesoid X receptor (FXR) and membrane Takeda G-protein-coupled receptor 5 (TGR5), and Citation: Xie, C.; Huang, W.; Young, the recognition of the effects of FXR and TGR5 signaling have led to a paradigm shift in knowledge R.L.; Jones, K.L.; Horowitz, M.; regarding bile acid physiology and metabolic health. -

British Society of Gastroenterology Guidelines on the Gut: First Published As 10.1136/Gutjnl-2021-324598 on 26 April 2021
Guidelines British Society of Gastroenterology guidelines on the Gut: first published as 10.1136/gutjnl-2021-324598 on 26 April 2021. Downloaded from management of irritable bowel syndrome Dipesh H Vasant ,1,2 Peter A Paine,2,3 Christopher J Black ,4,5 Lesley A Houghton ,5,6 Hazel A Everitt,7 Maura Corsetti,8 Anurag Agrawal,9 Imran Aziz ,10,11 Adam D Farmer,12,13 Maria P Eugenicos,14 Rona Moss- Morris,15 Yan Yiannakou,16 Alexander C Ford 4,5 ► Additional supplemental ABSTRACT (abdominal pain or discomfort, in association material is published online Irritable bowel syndrome (IBS) remains one of the most with altered bowel habit, for at least 6 months, only. To view, please visit the journal online (http:// dx. doi. org/ common gastrointestinal disorders seen by clinicians in in the absence of alarm symptoms or signs) is 10. 1136/ gutjnl- 2021- 324598). both primary and secondary care. Since publication of the more pragmatic and may be more applicable to last British Society of Gastroenterology (BSG) guideline patients with IBS in primary care than diagnostic For numbered affiliations see end of article. in 2007, substantial advances have been made in criteria derived from patients in secondary care, understanding its complex pathophysiology, resulting in such as the Rome IV criteria (recommendation: Correspondence to its re- classification as a disorder of gut- brain interaction, weak, quality of evidence: low). Professor Alexander C Ford, rather than a functional gastrointestinal disorder. ► All patients presenting with symptoms of IBS Leeds Gastroenterology Moreover, there has been a considerable amount of for the first time in primary care should have Institute, St James’s University new evidence published concerning the diagnosis, a full blood count, C reactive protein or eryth- Hospital, Leeds, UK; alexf12399@ yahoo. -

Evolution of the Bile Salt Nuclear Receptor FXR in Vertebrates
Supplemental Material can be found at: http://www.jlr.org/cgi/content/full/M800138-JLR200/DC1 Evolution of the bile salt nuclear receptor FXR in vertebrates † † † †† †† Erica J. Reschly,* Ni Ai, Sean Ekins, ,§,** William J. Welsh, Lee R. Hagey, Alan F. Hofmann, and Matthew D. Krasowski1,* † Department of Pathology,* University of Pittsburgh, Pittsburgh, PA 15261; Department of Pharmacology, University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School, Piscataway, NJ 08854; Collaborations in Chemistry,§ Jenkintown, PA 19046; Department of Pharmaceutical Sciences,** †† University of Maryland, Baltimore, MD 21202; and Department of Medicine, University of California-San Diego, San Diego, CA 92093-0063 Abstract Bile salts, the major end metabolites of cho- Bile salts are water-soluble, amphipathic end metabolites lesterol, vary significantly in structure across vertebrate of cholesterol that facilitate intestinal absorption of lipids species, suggesting that nuclear receptors binding these (1), enhance proteolytic cleavage of dietary proteins (2), Downloaded from molecules may show adaptive evolutionary changes. We com- and have potent antimicrobial activity in the small intestine pared across species the bile salt specificity of the major (3). In addition, bile salt signaling via nuclear hormone re- transcriptional regulator of bile salt synthesis, the farnesoid X receptor (FXR). We found that FXRs have changed speci- ceptors (NHRs) is important for bile salt homeostasis (4). ficity for primary bile salts across species by altering the Bile salts have not been detected in invertebrate animals. shape and size of the ligand binding pocket. In particular, In contrast to steroid hormones and vitamins, whose struc- the ligand binding pockets of sea lamprey (Petromyzon marinus) tures tend to be strongly conserved, bile salts exhibit www.jlr.org and zebrafish (Danio rerio) FXRs, as predicted by homology marked structural diversity across species (5–7). -

775 Sixth International Conference on Webometrics, Informetrics And
Sixth International Conference on Webometrics, Informetrics and Scientometrics & Eleventh COLLNET Meeting, October 19 – 22, 2010, University of Mysore, ALGORITHMIC GENERATION OF SPECIALTY PROFILES FOR MEDICAL JOURNALS Pudovkin A.I Institute of Marine Biology, Vladivostok 690041, Russia; e-mail: [email protected] E. Garfield ThomsonReuters Scientific, 1500 Spring Garden Street, Philadelphia, PA 19130-4067, e-mail: [email protected] Abstract A procedure for generating a topical profile of a medical journal is proposed. The procedure consists in calculating of the relatedness index Rgeom of a target journal with all 50 JCR medical categories and identification of top-related ones. The set of highly related categories (3 or 5) may be regarded as the specialty profile of the target journal. We illustrate the method by considering the content of 7 medical journals, 6 specialized ones and a leading multi-scope journal: Annals of Surgery, Circulation, Clinical Infectious diseases, European Heart Journal, Gut, Shock, and New England Journal of Medicine. The data for our analyses are taken from the 2006 and 2009 JCR Science Edition ―Related Journals‖ listings for each medical category. It is shown that the resulting specialty profiles are quite stable in time and well correspond to JCR‘s assignment of journals to subject categories. JCR‘s category assignment is a heuristic procedure performed by an expert, while our procedure is comletely algorithmic. KeyWords: journal topical specification; medical journals; JCR; Journal Relatedness Indexes Introduction The problem of classification, that is, specialty characterization of journals is an old and difficult one (Katz and Hicks, 1995; Boyack et al., 2005; Klavans and Boyack, 2006; Leydesdorff, 2006; Zhang et al., 2010a, b). -

Pancreatic Diseases and Microbiota: a Literature Review and Future Perspectives
Journal of Clinical Medicine Review Pancreatic Diseases and Microbiota: A Literature Review and Future Perspectives Marcantonio Gesualdo , Felice Rizzi *, Silvia Bonetto, Stefano Rizza, Federico Cravero, Giorgio Maria Saracco and Claudio Giovanni De Angelis * Gastroenterology and Digestive Endoscopy Unit, AOU Città della Salute e della Scienza, University of Turin, 10126 Turin, Italy; [email protected] (M.G.); [email protected] (S.B.); [email protected] (S.R.); [email protected] (F.C.); [email protected] (G.M.S.) * Correspondence: [email protected] (F.R.); [email protected] (C.G.D.A.) Received: 13 October 2020; Accepted: 30 October 2020; Published: 1 November 2020 Abstract: Gut microbiota represent an interesting worldwide research area. Several studies confirm that microbiota has a key role in human diseases, both intestinal (such as inflammatory bowel disease, celiac disease, intestinal infectious diseases, irritable bowel syndrome) and extra intestinal disorders (such as autism, multiple sclerosis, rheumatologic diseases). Nowadays, it is possible to manipulate microbiota by administering prebiotics, probiotics or synbiotics, through fecal microbiota transplantation in selected cases. In this scenario, pancreatic disorders might be influenced by gut microbiota and this relationship could be an innovative and inspiring field of research. However, data are still scarce and controversial. Microbiota manipulation could represent an important therapeutic strategy in the pancreatic diseases, in addition to standard therapies. In this review, we analyze current knowledge about correlation between gut microbiota and pancreatic diseases, by discussing on the one hand existing data and on the other hand future possible perspectives. Keywords: pancreatic diseases; microbiota; microbiome; gut microbiota; acute pancreatitis; chronic pancreatitis; diabetes mellitus; pancreatic ductal adenocarcinoma; pancreatic cystic neoplasms 1. -

Molecular Tuning of Farnesoid X Receptor Partial Agonism
ARTICLE https://doi.org/10.1038/s41467-019-10853-2 OPEN Molecular tuning of farnesoid X receptor partial agonism Daniel Merk1,6, Sridhar Sreeramulu2,6, Denis Kudlinzki2,3,4, Krishna Saxena2,3,4, Verena Linhard2, Santosh L. Gande2,3,4, Fabian Hiller2, Christina Lamers 1, Ewa Nilsson5, Anna Aagaard 5, Lisa Wissler 5, Niek Dekker5, Krister Bamberg 5, Manfred Schubert-Zsilavecz1 & Harald Schwalbe2,3,4 The bile acid-sensing transcription factor farnesoid X receptor (FXR) regulates multiple 1234567890():,; metabolic processes. Modulation of FXR is desired to overcome several metabolic patholo- gies but pharmacological administration of full FXR agonists has been plagued by mechanism-based side effects. We have developed a modulator that partially activates FXR in vitro and in mice. Here we report the elucidation of the molecular mechanism that drives partial FXR activation by crystallography- and NMR-based structural biology. Natural and synthetic FXR agonists stabilize formation of an extended helix α11 and the α11-α12 loop upon binding. This strengthens a network of hydrogen bonds, repositions helix α12 and enables co- activator recruitment. Partial agonism in contrast is conferred by a kink in helix α11 that destabilizes the α11-α12 loop, a critical determinant for helix α12 orientation. Thereby, the synthetic partial agonist induces conformational states, capable of recruiting both co- repressors and co-activators leading to an equilibrium of co-activator and co-repressor binding. 1 Institute of Pharmaceutical Chemistry, Goethe University, Frankfurt 60348, Germany. 2 Center for Biomolecular Magnetic Resonance (BMRZ), Institute for Organic Chemistry and Chemical Biology, Goethe University, Frankfurt 60438, Germany. 3 German Cancer Consortium (DKTK), Heidelberg 69120, Germany. -

Journals from BMJ
Journals from BMJ journals.bmj.com BMJ started out over 170 years ago as Providing high quality content for health professionals and a medical journal, publishing our first researchers across the world. Our journals include not only the BMJ, research paper. but some of the most influential speciality journals in their field. Now, as a global brand with a worldwide audience, we help medical organisations and clinicians tackle today’s most critical • In the last 12 months, over 50 million unique users accessed healthcare challenges. our subscription journals online, generating over 107 million page views. What is an Our vision is to create ‘a healthier world’. • Nearly 80% of our titles saw Impact Factor rises in 2014. Impact Factor? BMJ’s journals division now publishes more than 50 of the • 21% of our users view journal content from mobile devices. An Impact Factor (IF) is a measure of world’s leading medical and allied science journals. In doing so, the frequency with which the average we have pioneered the migration to digital publishing and the article in a journal has been cited in development of open access. a particular year. The annual Journal For more information or to of Citation Reports impact factor is a ratio between citations and recent Today, our expertise extends to medical education, clinical arrange a trial, please contact: citable items published. Thus, the decision support, data analytics and quality improvement to BMJ Consortia sales impact factor of a journal is calculated enhance day to day decision-making and healthcare delivery. by dividing the number of current E: [email protected] year citations to the source items T: +44 (0) 20 7383 6438 published in that journal during the “At BMJ we believe the work we do previous two years. -
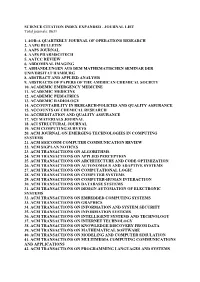
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

The Human Gut Microbiota: a Dynamic Interplay with the Host from Birth to Senescence Settled During Childhood
Review nature publishing group The human gut microbiota: a dynamic interplay with the host from birth to senescence settled during childhood Lorenza Putignani1, Federica Del Chierico2, Andrea Petrucca2,3, Pamela Vernocchi2,4 and Bruno Dallapiccola5 The microbiota “organ” is the central bioreactor of the gastroin- producing immunological memory (2). Indeed, the intestinal testinal tract, populated by a total of 1014 bacteria and charac- epithelium at the interface between microbiota and lymphoid terized by a genomic content (microbiome), which represents tissue plays a crucial role in the mucosa immune response more than 100 times the human genome. The microbiota (2). The IS ability to coevolve with the microbiota during the plays an important role in child health by acting as a barrier perinatal life allows the host and the microbiota to coexist in a against pathogens and their invasion with a highly dynamic relationship of mutual benefit, which consists in dispensing, in modality, exerting metabolic multistep functions and stimu- a highly coordinated way, specific immune responses toward lating the development of the host immune system, through the biomass of foreign antigens, and in discriminating false well-organized programming, which influences all of the alarms triggered by benign antigens (2). The failure to obtain growth and aging processes. The advent of “omics” technolo- or maintain this complex homeostasis has a negative impact gies (genomics, proteomics, metabolomics), characterized by on the intestinal and systemic health (2). Once the balance complex technological platforms and advanced analytical and fails, the “disturbance” causes the disease, triggering an abnor- computational procedures, has opened new avenues to the mal inflammatory response as it happens, for example, for the knowledge of the gut microbiota ecosystem, clarifying some inflammatory bowel diseases in newborns (2).