Spinal Subarachnoid Hemorrhage Migrated from Traumatic Intracranial Subarachnoid Hemorrhage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Positive Cases in Suspected Cauda Equina Syndrome
Edinburgh Research Explorer The clinical features and outcome of scan-negative and scan- positive cases in suspected cauda equina syndrome Citation for published version: Hoeritzauer, I, Pronin, S, Carson, A, Statham, P, Demetriades, AK & Stone, J 2018, 'The clinical features and outcome of scan-negative and scan-positive cases in suspected cauda equina syndrome: a retrospective study of 276 patients', Journal of Neurology, vol. 265, no. 12. https://doi.org/10.1007/s00415- 018-9078-2 Digital Object Identifier (DOI): 10.1007/s00415-018-9078-2 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Journal of Neurology Publisher Rights Statement: This is an open access article distributed under the terms of the Creative Commons CC BY license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 04. Oct. 2021 Journal of Neurology (2018) 265:2916–2926 https://doi.org/10.1007/s00415-018-9078-2 ORIGINAL COMMUNICATION The clinical features and outcome of scan-negative and scan-positive cases in suspected cauda equina syndrome: a retrospective study of 276 patients Ingrid Hoeritzauer1,2,5 · Savva Pronin1,5 · Alan Carson1,2,3 · Patrick Statham2,4,5 · Andreas K. -

Management of the Head Injury Patient
Management of the Head Injury Patient William Schecter, MD Epidemilogy • 1.6 million head injury patients in the U.S. annually • 250,000 head injury hospital admissions annually • 60,000 deaths • 70-90,000 permanent disability • Estimated cost: $100 billion per year Causes of Brain Injury • Motor Vehicle Accidents • Falls • Anoxic Encephalopathy • Penetrating Trauma • Air Embolus after blast injury • Ischemia • Intracerebral hemorrhage from Htn/aneurysm • Infection • tumor Brain Injury • Primary Brain Injury • Secondary Brain Injury Primary Brain Injury • Focal Brain Injury – Skull Fracture – Epidural Hematoma – Subdural Hematoma – Subarachnoid Hemorrhage – Intracerebral Hematorma – Cerebral Contusion • Diffuse Axonal Injury Fracture at the Base of the Skull Battle’s Sign • Periorbital Hematoma • Battle’s Sign • CSF Rhinorhea • CSF Otorrhea • Hemotympanum • Possible cranial nerve palsy http://health.allrefer.com/pictures-images/ Fracture of maxillary sinus causing CSF Rhinorrhea battles-sign-behind-the-ear.html Skull Fractures Non-depressed vs Depressed Open vs Closed Linear vs Egg Shell Linear and Depressed Normal Depressed http://www.emedicine.com/med/topic2894.htm Temporal Bone Fracture http://www.vh.org/adult/provider/anatomy/ http://www.bartleby.com/107/illus510.html AnatomicVariants/Cardiovascular/Images0300/0386.html Epidural Hematoma http://www.chestjournal.org/cgi/content/full/122/2/699 http://www.bartleby.com/107/illus769.html Epidural Hematoma • Uncommon (<1% of all head injuries, 10% of post traumatic coma patients) • Located -

Cardiovascular Collapse Following Succinylcholine in a Paraplegic Patient
ParajJleg£a (I973), II, 199-204 CARDIOVASCULAR COLLAPSE FOLLOWING SUCCINYLCHOLINE IN A PARAPLEGIC PATIENT By J. C. SNOW,! M.D., B. J. KRIPKE, M.D. , G. P. SESSIONS, M.D. and A. J. FINCK, M.D. University Hospital, Boston, DeKalb General Hospital, Decatur, Georgia, and Boston University School of Medicine, Boston, Massachusetts 02118 INTRODUCTION SEVERAL reports have been presented that have discussed cardiovascular collapse following the intravenous infusion of succinylcholine in patients with burns, massive trauma,tetanus, spinal cord injury, brain injury,upper or lower motor neuron disease,and uraemia with increased serum potassium. The purpose of this article is to report a spinal cord injured patient who developed cardiac arrest following administration of succinylcholine, possibly due to succinylcholine-induced hyperkalaemia. The anaesthesia management during the course of subsequent surgical procedure proved to be uneventful. CASE REPORT On 7 December 1971, a 20-year-old white man was admitted to the hospital after he fell 50 feet from a scaffold to the ground. He was reported to have been in good health until this accident. His legs and outstretched hands absorbed the major impact. No loss of consciousness was reported at any time. Neurologic examination revealed absent function of muscle groups in the distribution distal to L4, including the sacral segments. There were contractions of both quadriceps muscles in the adductors of the legs. The legs were held in flexion with no evidence of function in his hip abductors, extensors, knee flexors or anything below his knee. He had intact sensation over the entire thigh and medial calf. He had no apparent abdominal or cremasteric reflexes, no knee or ankle jerks, no Babinski responses, and no sacral sparing. -

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Intracranial Hemorrhage As Initial Presentation of Cerebral Venous Sinus Thrombosis
Case Report Journal of Heart and Stroke Published: 31 Dec, 2019 Intracranial Hemorrhage as Initial Presentation of Cerebral Venous Sinus Thrombosis Joseph Y Chu1* and Marc Ossip2 1Department of Medicine, University of Toronto, Canada 2Department of Diagnostic Imaging, William Osler Health System, Canada Abstract Intracranial Hemorrhage (ICH) as initial presentation is an uncommon complication of Cerebral Venous-Sinus Thrombosis (CVT). Clinical and neuro-imaging studies of 4 cases of ICH due cerebral venous-sinus thrombosis seen at the William Osler Health System in Toronto will be presented. Discussion of the immediate and long-term management of these interesting cases will be reviewed with emphasis on the appropriate neuro-imaging studies. Literature review of Direct Oral Anticoagulants (DOAC) in the long-term management of these challenging cases will be discussed. Introduction The following are four cases of Cerebral Venous-Sinus Thrombosis (CVT) who present initially as Intracranial Hemorrhage (ICH). Clinical details, including immediate and long term management and neuro-imaging studies are presented. Results Case 1 A 43 years old R-handed house wife, South-Asian decent, who was admitted to hospital on 06- 10-2014 with sudden headache and right hemiparesis. Her past health shows no prior hypertension or stroke. She is not on any hormone replacement therapy, non-smoker and non-drinker. Married with 1 daughter. Examination shows BP=122/80, P=70 regular, GCS=15, with right homonymous hemianopsia, right hemiparesis: arm=leg 1/5, extensor R. Plantar response. She was started on IV Heparin after her unenhanced CT showed acute left parietal intracerebral hemorrhage and her MRV showed extensive sagittal sinus thrombosis extending into the left transverse OPEN ACCESS sinus (Figures 1,2). -

Early Management of Retained Hemothorax in Blunt Head and Chest Trauma
World J Surg https://doi.org/10.1007/s00268-017-4420-x ORIGINAL SCIENTIFIC REPORT Early Management of Retained Hemothorax in Blunt Head and Chest Trauma 1,2 1,8 1,7 1 Fong-Dee Huang • Wen-Bin Yeh • Sheng-Shih Chen • Yuan-Yuarn Liu • 1 1,3,6 4,5 I-Yin Lu • Yi-Pin Chou • Tzu-Chin Wu Ó The Author(s) 2018. This article is an open access publication Abstract Background Major blunt chest injury usually leads to the development of retained hemothorax and pneumothorax, and needs further intervention. However, since blunt chest injury may be combined with blunt head injury that typically requires patient observation for 3–4 days, other critical surgical interventions may be delayed. The purpose of this study is to analyze the outcomes of head injury patients who received early, versus delayed thoracic surgeries. Materials and methods From May 2005 to February 2012, 61 patients with major blunt injuries to the chest and head were prospectively enrolled. These patients had an intracranial hemorrhage without indications of craniotomy. All the patients received video-assisted thoracoscopic surgery (VATS) due to retained hemothorax or pneumothorax. Patients were divided into two groups according to the time from trauma to operation, this being within 4 days for Group 1 and more than 4 days for Group 2. The clinical outcomes included hospital length of stay (LOS), intensive care unit (ICU) LOS, infection rates, and the time period of ventilator use and chest tube intubation. Result All demographics, including age, gender, and trauma severity between the two groups showed no statistical differences. -

Iatrogenic Spinal Subarachnoid Hematoma After Diagnostic Lumbar Puncture
https://doi.org/10.14245/kjs.2017.14.4.158 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(4):158-161, 2017 www.e-kjs.org Iatrogenic Spinal Subarachnoid Hematoma after Diagnostic Lumbar Puncture Jung Hyun Park, Spinal subarachnoid hematoma (SSH) following diagnostic lumbar puncture is very rare. Generally, Jong Yeol Kim SSH is more likely to occur when the patient has coagulopathy or is undergoing anticoagulant therapy. Unlike the usual complications, such as headache, dizziness, and back pain at the Department of Neurosurgery, Kosin needle puncture site, SSH may result in permanent neurologic deficits if not properly treated University Gospel Hospital, Kosin within a short period of time. An otherwise healthy 43-year-old female with no predisposing University College of Medicine, factors presented with fever and headache. Diagnostic lumbar puncture was performed under Busan, Korea suspicion of acute meningitis. Lumbar magnetic resonance imaging was performed due to hypo- Corresponding Author: esthesia below the level of T10 that rapidly progressed after the lumbar puncture. SSH was Jong Yeol Kim diagnosed, and high-dose steroid therapy was started. Her neurological symptoms rapidly deterio- Department of Neurosurgery, rated after 12 hours despite the steroids, necessitating emergent decompressive laminectomy Kosin University Gospel Hospital, and hematoma removal. The patient’s condition improved after the surgery from a preoperative Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan motor score of 1/5 in the right leg and 4/5 in the left leg to brace-free ambulation (motor grade 49267, Korea 5/5) 3-month postoperative. -

Symptomatic Intracranial Hemorrhage (Sich) and Activase® (Alteplase) Treatment: Data from Pivotal Clinical Trials and Real-World Analyses
Symptomatic intracranial hemorrhage (sICH) and Activase® (alteplase) treatment: Data from pivotal clinical trials and real-world analyses Indication Activase (alteplase) is indicated for the treatment of acute ischemic stroke. Exclude intracranial hemorrhage as the primary cause of stroke signs and symptoms prior to initiation of treatment. Initiate treatment as soon as possible but within 3 hours after symptom onset. Important Safety Information Contraindications Do not administer Activase to treat acute ischemic stroke in the following situations in which the risk of bleeding is greater than the potential benefit: current intracranial hemorrhage (ICH); subarachnoid hemorrhage; active internal bleeding; recent (within 3 months) intracranial or intraspinal surgery or serious head trauma; presence of intracranial conditions that may increase the risk of bleeding (e.g., some neoplasms, arteriovenous malformations, or aneurysms); bleeding diathesis; and current severe uncontrolled hypertension. Please see select Important Safety Information throughout and the attached full Prescribing Information. Data from parts 1 and 2 of the pivotal NINDS trial NINDS was a 2-part randomized trial of Activase® (alteplase) vs placebo for the treatment of acute ischemic stroke. Part 1 (n=291) assessed changes in neurological deficits 24 hours after the onset of stroke. Part 2 (n=333) assessed if treatment with Activase resulted in clinical benefit at 3 months, defined as minimal or no disability using 4 stroke assessments.1 In part 1, median baseline NIHSS score was 14 (min: 1; max: 37) for Activase- and 14 (min: 1; max: 32) for placebo-treated patients. In part 2, median baseline NIHSS score was 14 (min: 2; max: 37) for Activase- and 15 (min: 2; max: 33) for placebo-treated patients. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -
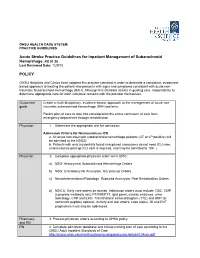
Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 POLICY
OHSU HEALTH CARE SYSTEM PRACTICE GUIDELINES Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 Last Reviewed Date: 1/29/10 POLICY OHSU Hospitals and Clinics have adopted this practice standard in order to delineate a consistent, evidenced- based approach to treating the patient who presents with signs and symptoms consistent with acute non- traumatic Subarachnoid Hemorrhage (SAH). Although this standard assists in guiding care, responsibility to determine appropriate care for each individual remains with the provider themselves. Outcomes/ Create a multi-disciplinary, evidence-based, approach to the management of acute non- goals traumatic subarachnoid hemorrhage (SAH) patients. Patient plan of care to take into consideration the entire continuum of care from emergency department through rehabilitation. Physician 1. Determine the appropriate unit for admission. Admission Criteria for Neurosciences ICU a. All acute non-traumatic subarachnoid hemorrhage patients (CT or LP positive) will be admitted to the NSICU. b. Patients with only incidentally found unruptured aneurysms do not need ICU care, unless routine post-op ICU care is required, and may be admitted to 10K. ( Physician 2. Complete appropriate physician order set in EPIC: a) NSG: Aneurysmal Subarachnoid Hemorrhage Orders. b) NSG: Craniotomy for Aneurysm: ICU post-op Orders. c) NeuroInterventional Radiology: Ruptured Aneurysm: Post Embolization Orders. d) NSICU: Daily care orders on rounds. Admission orders must include: CBC, CMP (complete metabolic set), PT/INR/PTT, lipid panel, cardiac enzymes, urine toxicology, CXR and EKG. Transthoracic echocardiogram (TTE) and BNP (B- natriuretic peptide) optional. Activity and diet orders, code status, GI and DVT prophylaxis must also be addressed. -

A Cauda Equina Syndrome in a Patient Treated with Oral Anticoagulants
Paraplegia 32 (1994) 277-280 © 1994 International Medical Society of Paraplegia A cauda equina syndrome in a patient treated with oral anticoagulants. Case report l l l 2 l J Willems MD, A Anne MD, P Herregods MD, R Klaes MD, R Chappel MD 1 Department of Physical Medicine and Rehabilitation, 2 Department of Neurosurgery, A.z. Middelheim, Lindendreef 1, B-2020 Antwerp, Belgium. The authors report a patient who was on oral anticoagulants because of mitral valve disease and who developed paraplegia from subarachnoid bleeding involv ing the cauda equina. The differential diagnosis, investigations and treatment of the cauda equina syndrome are described. Keywords: cauda equina syndrome; anticoagulants; subarachnoid haemorrhage; mitral valve disease. Case report A 32 year old woman from Chile presented with a complete paraplegia. She claimed that the paraplegia had developed progressively over 8 months. Initially she had paraesthesiae in her feet, followed by progressive paresis of both legs, beginning distally, over a period of 3 months. Two months after the onset of illness she complained of bladder incontinence. There was no history of trauma or low back pain. Clinical examination in our hospital revealed a flaccid paraplegia at L1 level, and loss of sensation from the groins to the feet, including saddle anaesthesia. The knee and ankle jerks were absent. The anal sphincter was atonic. She had an indwelling urethral catheter, and she was faecally incontinent. Myelography and a CT scan were carried out, and a space-occupying lesion at the level of T12-L4 (Figs 1, 2) was defined. Surgical ex ploration was done to determine the cause. -

On Lumbar Disc Herniation – Aspects of Outcome After Surgical Treatment
From the Dept. of Clinical Sciences, Intervention and Technology (CLINTEC), Karolinska Institutet and the Dept. of Clinical Science and Education, Södersjukhuset, Karolinska Institutet Stockholm Sweden On Lumbar Disc Herniation – Aspects of outcome after surgical treatment Peter Elkan Stockholm 2017 1 The frontpage picture is published with license from: Zephyr/Science Photo Library/IBL http://www.sciencephoto.com/ All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by E-PRINT © Peter Elkan, 2017 ISBN 978-91-7676-712-2 2 Institutionen för klinisk vetenskap, intervention och teknik, Enheten för ortopedi och bioteknologi, Karolinska Institutet On Lumbar Disc Herniation – Aspects of outcome after surgical treatment AKADEMISK AVHANDLING som för avläggande av medicine doktorsexamen vid Karolinska Institutet offentligen försvaras i Aulan, 6 tr, Södersjukhuset Sjukhusbacken 10, Stockholm Fredag 19 maj, kl 09:00 Av Peter Elkan Handledare Opponent Docent Paul Gerdhem Enheten för ortopedi Docent Bengt Sandén Institutionen för och bioteknologi Institutionen för klinisk kirurgiska vetenskaper vetenskap, intervention och teknik Uppsala Universitet Karolinska Institutet Bihandledare Betygsnämnd Professor Sari Ponzer Institutionen för klinisk Professor Olle Svensson Institutionen för forskning och utbildning, Södersjukhuset kirurgi och perioperativ vetenskap Karolinska institutet Umeå Universitet Med dr Ulric Willers Institutionen för klinisk Professor Lars Weidenhielm Institutionen för forskning och utbildning, Södersjukhuset molekylär medicin och kirurgi Karolinska institutet Karolinska Institutet Adj. professor Rune Hedlund Institutionen för Docent Gunnar Ordeberg Institutionen för kliniska vetenskaper kirurgiska vetenskaper Sahlgrenska Akademin Uppsala Universitet Stockholm 2017 3 4 To my dear family, all patients suffering from sciatic pain and all patients who have contributed with data in this project.