(QIP) Narrative for Health Care Organizations in Ontario
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Academic Gastroenterologist University Health Network, Sinai Health System, and University of Toronto
Assistant / Associate Professor - Academic Gastroenterologist University Health Network, Sinai Health System, and University of Toronto The Department of Medicine, Faculty of Medicine at the University of Toronto and the Division of Gastroenterology of the University Health Network (UHN) and Sinai Health System (SHS) is seeking to recruit a permanent, full-time Clinician-Teacher, Clinician Investigator or Clinician in Quality Improvement in Gastroenterology. The successful candidate must be eligible for a full-time clinical academic appointment at the rank of Assistant or Associate Professor at the University of Toronto. The anticipated start date will be on June 1, 2017 or to be mutually agreed upon The successful candidate must hold a MD and FRCPC qualifications or equivalent, be eligible for certification by the Royal College of Physicians and Surgeons of Canada in Gastroenterology and have, or be eligible for, licensure in Ontario. In addition, completion of a postgraduate degree such as a MSc or equivalent is required. The position requires an individual who has demonstrated excellence in advanced endoscopic skills which include being proficient in ERCP and associated therapeutic interventions with significant experience in hepatopancreatobiliary malignancy and liver transplantation patient populations. Excellent teaching abilities are also required. The combined Division of Gastroenterology of the UHN and SHS in Toronto is a group of 26 luminal gastroenterologists and hepatologists. The Division has active clinical and research programs in many areas of gastroenterology and hepatology including IBD, nutrition, pancreatic physiology, neurogastroenterology and motility, viral hepatitis, cholestatic and autoimmune liver diseases, fatty liver, portal hypertension, hepatocellular carcinoma and liver transplantation. SHS is a health care organization comprised of Mount Sinai Hospital, Bridgepoint Active Healthcare and Circle of Care as an affiliate, extending SHS’s continuum of care into home and community programs. -

Active COVID-19 Outbreaks in Toronto Hospitals and Retirement Homes, December 7, 2020
Active COVID-19 Outbreaks in Toronto Hospitals and Retirement Homes, December 7, 2020 Current Outbreak Number Location Name Resident Cases Staff Cases Deaths Reported Date Hospitalizations 3895-2020-02040 AMICA BALMORAL CLUB RETIREMENT HOME 2 3 0 1 23-Nov-20 3895-2020-02098 AMICA BAYVIEW VILLAGE 1 2 0 0 25-Nov-20 3895-2020-01871 ARUL OLI SENIOR CENTRE 8 3 0 0 16-Nov-20 3895-2020-02211 BRIDGEPOINT ACTIVE HEALTHCARE - SINAI HEALTH SYSTEM 2 0 0 0 30-Nov-20 3895-2020-02053 CENTRE FOR ADDICTION AND MENTAL HEALTH - QUEEN SITE 2 0 0 0 24-Nov-20 3895-2020-02250 CENTRE FOR ADDICTION AND MENTAL HEALTH - QUEEN SITE 0 2 0 0 02-Dec-20 3895-2020-01662 CHARTWELL SCARLETT HEIGHTS RETIREMENT HOME 22 5 1 0 01-Nov-20 3895-2020-02130 DOWLING REST HOME 6 0 0 2 26-Nov-20 3895-2020-01747 FOREST HILL PLACE R.R.-REVERA 21 22 2 3 04-Nov-20 3895-2020-01825 HAROLD AND GRACE BAKER CENTRE 2 2 0 0 13-Nov-20 3895-2020-01830 LEASIDE 8 3 0 0 14-Nov-20 3895-2020-02004 MCCALL CENTRE FOR CONTINUING CARE 4 3 0 0 23-Nov-20 3895-2020-02239 MOUNT SINAI HOSPITAL - SINAI HEALTH SYSTEM 3 0 0 2 30-Nov-20 3895-2020-01395 SAGE CARE 44 48 11 0 23-Oct-20 3895-2020-02140 SCARBOROUGH HEALTH NETWORK - BIRCHMOUNT HOSPITAL 3 0 1 1 27-Nov-20 3895-2020-02153 SCARBOROUGH HEALTH NETWORK - CENTENARY HOSPITAL 4 0 0 3 27-Nov-20 3895-2020-02066 SCARBOROUGH HEALTH NETWORK - GENERAL HOSPITAL 6 1 0 3 24-Nov-20 3895-2020-02082 SCARBOROUGH HEALTH NETWORK - GENERAL HOSPITAL 4 2 1 1 25-Nov-20 3895-2020-02350 SCARBOROUGH HEALTH NETWORK - GENERAL HOSPITAL 2 0 0 2 05-Dec-20 3895-2020-02100 ST. -

Sinai Health System
Financial statements of Sinai Health System March 31, 2016 Sinai Health System For the year ended March 31, 2016 Table of contents Independent auditor’s report ...................................................................................................................... 1-2 Statement of financial position ...................................................................................................................... 3 Statement of operations ................................................................................................................................ 4 Statement of changes in net assets .............................................................................................................. 5 Statement of remeasurement gains and losses .......................................................................................... 6 Statement of cash flows ................................................................................................................................ 7 Notes to the financial statements ............................................................................................................. 8-23 June 14, 2016 Independent Auditor’s Report To the Board of Directors of Sinai Health System We have audited the accompanying financial statements of Sinai Health System, which comprise the statements of financial position as at March 31, 2016 and the statements of operations, statements of changes in net assets (deficit), remeasurement gains and losses and cash flows for the years -
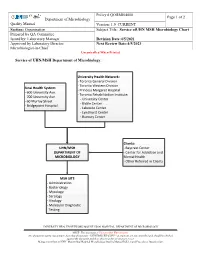
Service of UHN/MSH Microbiology Chart
Policy # QORMI04000 Page 1 of 2 Department of Microbiology Quality Manual Version: 1.0 CURRENT Section: Organization Subject Title: Service ofUHN MSH Microbiology Chart Prepared by QA Committee Issued by: Laboratory Manager Revision Date:4/5/2021 Approved by Laboratory Director: Next Review Date:4/5/2023 Microbiologist-in-Chief Uncontrolled When Printed Service of UHN/MSH Department of Microbiology: University Health Network: - Toronto General Division - Toronto Western Division Sinai Health System: - Princess Margaret Hospital - 600 University Ave. - Toronto Rehabilitation Institute: - 700 University Ave. - University Center - 60 Murray Street - Bickle Center - Bridgepoint Hospital - Lakeside Center - Lyndhurst Center - Rumsey Center Clients: UHN/MSH - Baycrest Center DEPARTMENT OF - Center for Addiction and MICROBIOLOGY Mental Health - Other Referred in Clients MSH SITE - Administration - Bacteriology - Mycology - Serology - Virology - Molecular Diagnostic Testing UNIVERSITY HEALTH NETWORK/MOUNT SINAI HOSPITAL, DEPARTMENT OF MICROBIOLOGY NOTE: This document is Uncontrolled When Printed. Any documents appearing in paper form that do not state "CONTROLLED COPY " in red print are not controlled and should be checked against the document (titled as above) on the server prior to use. Management System\UHN_Mount Sinai Hospital Microbiology\Quality Manual Policies and Procedures\Organization\ Policy # QORMI04000 Page 2 of 2 Department of Microbiology Quality Manual Version: 1.0 CURRENT Section: Organization Subject Title: Service ofUHN MSH Microbiology Chart Record of Edited Revisions Manual Section Name: Service of UHN MSH Microbiology Chart Page Number / Item Date of Revision Signature of Approval Annual Review March 5, 2005 Dr. T. Mazzulli Annual Review April 24, 2006 Dr. T. Mazzulli Annual Review May 2, 2007 Dr. T. Mazzulli Annual Review June 16, 2008 Dr. -

Supporting Those Impacted by COVID-19
Supporting those impacted by COVID-19 Many of you have reached out to us either looking for suggestions or offering ideas on how our TFS community can support those impacted by COVID-19. We are indeed a strong community and we know that it is essential, as citizens, that we act for the common good, most especially in situations such as this one. Please see below a list of organizations that you might want to support, specifically considering the shortage of personal protective equipment and other items. Of the many worthy institutions making an impact, we have put together a list of those with which we have partnered over the years as part of our citizenship program or where our alumni and parents are engaged. We will post this list online at tfs.ca and sr.tfs.ca/coronavirus. To quote President John F. Kennedy, from his inaugural speech, “Ask not what your country can do for you - ask what you can do for your country.” Or province or city. And, of course, for the world at large. Thank you! Baycrest Hospital CAMH Canadian Cancer Society Daily Bread Food Bank Holland Bloorview Kids Rehabilitation Hospital Humber River Hospital Lakeridge Health Mackenzie Health Markham Stouffville Hospital Michael Garron Hospital Foundation Oakville Hospital Foundation North York General Hospital Foundation Second Harvest Scarborough Hospital Network Foundation Sick Kids Foundation Sinai Health System Southlake Regional Health Centre Sunnybrook Health Sciences Centre Toronto General & Western Hospitals Toronto Rehab Trillium Health Partners Foundation Unity Health (St. Michael's, St. Joseph's and Providence Health Care) War Child William Osler Health System Women's College Hospital Foundation . -

Active COVID-19 Outbreaks in Toronto Hospitals and Retirement Homes, December 9, 2020
Active COVID-19 Outbreaks in Toronto Hospitals and Retirement Homes, December 9, 2020 Current Outbreak Number Location Name Resident Cases Staff Cases Deaths Reported Date Hospitalizations 3895-2020-02040 AMICA BALMORAL CLUB RETIREMENT HOME 2 3 1 1 23-Nov-20 3895-2020-02098 AMICA BAYVIEW VILLAGE 1 3 0 0 25-Nov-20 3895-2020-01871 ARUL OLI SENIOR CENTRE 8 3 0 0 16-Nov-20 3895-2020-02211 BRIDGEPOINT ACTIVE HEALTHCARE - SINAI HEALTH SYSTEM 2 0 0 0 30-Nov-20 3895-2020-02250 CENTRE FOR ADDICTION AND MENTAL HEALTH - QUEEN SITE 0 2 0 0 02-Dec-20 3895-2020-01662 CHARTWELL SCARLETT HEIGHTS RETIREMENT HOME 22 5 1 0 01-Nov-20 3895-2020-02130 DOWLING REST HOME 6 0 0 1 26-Nov-20 3895-2020-01747 FOREST HILL PLACE R.R.-REVERA 22 22 2 2 04-Nov-20 3895-2020-01825 HAROLD AND GRACE BAKER CENTRE 2 2 0 0 13-Nov-20 3895-2020-01830 LEASIDE 8 3 0 0 14-Nov-20 3895-2020-02004 MCCALL CENTRE FOR CONTINUING CARE 5 2 0 0 23-Nov-20 3895-2020-02239 MOUNT SINAI HOSPITAL - SINAI HEALTH SYSTEM 6 0 1 4 30-Nov-20 3895-2020-01395 SAGE CARE 44 48 11 0 23-Oct-20 3895-2020-02140 SCARBOROUGH HEALTH NETWORK - BIRCHMOUNT HOSPITAL 3 0 1 1 27-Nov-20 3895-2020-02153 SCARBOROUGH HEALTH NETWORK - CENTENARY HOSPITAL 4 0 0 2 27-Nov-20 3895-2020-02066 SCARBOROUGH HEALTH NETWORK - GENERAL HOSPITAL 6 1 0 3 24-Nov-20 3895-2020-02350 SCARBOROUGH HEALTH NETWORK - GENERAL HOSPITAL 2 0 0 2 04-Dec-20 3895-2020-02100 ST. -

The Facts of COVID in Ontario Claim Correction Hospital Occupancy Is
The Facts of COVID in Ontario Claim Correction Hospital Capacity challenges exist in hospitals across Ontario, with over 40 hospital corporations reporting occupancy rates in excess of 90% on occupancy is January 7, 2021. better than pre- pandemic. Dr. Brown presented alarming trends mere days ago, which Mr. Baber would have been briefed on. Over the last four weeks, there has been a 72 per cent increase in hospitalizations and a 61 per cent increase in ICU patients. Further, more than half of the provincial ICUs are full or only have one or two beds left. Dr. Brown notes that if we stay on our current trajectory, there will be more than 1,000 COVID-19 patients in ICU by early February. That would be catastrophic. COVID patients in hospital: • Outbreaks have closed beds in key centres like Trillium Health Partners, William Osler Health System and Greater Niagara General. • Key hospitals experiencing significant increases in capacity pressures (as of January 3, 2021): • Trillium Health Partners – 96% total ICU occupancy • Windsor Regional Hospital – 90.2% total ICU occupancy • Humber River Hospital – 97.8% total ICU occupancy • Halton Healthcare Services – 93.8% total ICU occupancy • Markham Stouffville Hospital – 120% total ICU occupancy • Mackenzie Health – 94.7% Total ICU occupancy As you may know, Mr. Baber represents a Toronto riding. Below you’ll find the ICU occupancy for the Toronto and surrounding areas as of January 15, 2021: PHU CORPORATION NAME SITE NAME OCCUPANCY TORONTO Humber River Regional Hospital Wilson Site 95.7% TORONTO North York General Hospital North York General Hospital 82.6% TORONTO Scarborough Health Network Birchmount 86.7% TORONTO Scarborough Health Network Centenary 106.7% TORONTO Scarborough Health Network General 88.6% TORONTO Sinai Health System Mount Sinai Hospital 93.5% TORONTO Sunnybrook Health Sciences Centre Bayview Campus 96.8% TORONTO Toronto East Health Network Michael Garron Hospital 87.0% TORONTO Unity Health Toronto St. -

Mount Sinai Hospital
Toronto Invasive Bacterial Diseases Network INFORMATION ABOUT A RESEARCH STUDY – STAFF and CAREGIVERS TIBDN CO-ORDINATING INVESTIGATOR: Dr. Allison McGeer Study Title: Immunogenicity of COVID-19 Vaccines in Long Term Care (CovidAB) 416-586-3123 Study Doctors: Dr. Anne Claude Gingras, Sinai Health System COVIDAB RESEARCH COORDINATOR: Dr. Allison McGeer, Sinai Health System Ms. Lois Gilbert Dr. Jen Gommerman, University of Toronto 416-586-4800, 2767 Dr. Sharon Straus, Unity Health Toronto Dr. Mario Ostrowski, Unity Health RESEARCH ASSOCIATES: Mr. Agron Plevneshi Ms. Nadia Malik What is the purpose of this study? Ms. Mare Pejkovska Ms. Asfia Sultana The purpose of this study is to better understand how vaccines work against COVID-19. We Ms. Amna Faheem wish to describe: Ms. Saman Khan 1. how much antibody people make when they are vaccinated against the virus that Mr. Kazi Hassan Ms. Tamara Vikulova causes COVID-19 Ms. Gloria Crowl 2. how long the antibody lasts Ms. Zoe Zhong Ms. Lubna Farooqi 3. whether people who have had COVID-19 before make more antibody, or have antibody that lasts longer RESEARCH TECHNOLOGISTS: 4. whether residents of long term care homes make less antibody than other adults Ms. Aimee Paterson 5. whether antibodies can be detected in saliva of individuals vaccinated against Ms. Angel Xin Liu COVID19 , how it compares to antibody levels detected in blood, and how long does it last in the saliva MAIN OFFICE: Mount Sinai Hospital Who can participate? Anyone who works, or is an essential caregiver at a long term care 600 University Avenue home in south central Ontario, and who is planning to be vaccinated against COVID-19. -

Academic Hepatologist - Clinician Investigator University Health Network and University of Toronto
Academic Hepatologist - Clinician Investigator University Health Network and University of Toronto The Department of Medicine, Faculty of Medicine at the University of Toronto and the Division of Gastroenterology of the University Health Network and Sinai Health System is seeking to recruit an Academic Clinical Investigator for The Toronto Centre for Liver Disease, University Health Network. The successful candidate must be eligible for a full-time clinical academic appointment at the rank of Assistant or Associate Professor at the University of Toronto. The anticipated start date is August 1, 2017, or shortly thereafter. The successful candidate must hold MD and FRCPC qualifications or equivalent, be eligible for certification by the Royal College of Physicians and Surgeons of Canada in gastroenterology and hepatology and have, or be eligible for licensure in Ontario. In addition, they will have completed an MSc, PhD or equivalent training in clinical gastroenterology and hepatology. The ideal candidate will have demonstrated excellence in the field of hepatology and a particular interest in liver tumors. S/he will work alongside a vibrant multidisciplinary research and clinical team and will contribute in all aspects to perpetuate the vision to provide excellence in patient care, research and teaching. The successful applicant should also have the vision and organizational skills necessary to further grow the Liver Research Program. S/he will focus on hepatoma -related clinical care and research such that approximately 50% of their time will be allocated to research. The combined Division of Gastroenterology of the University Health Network and Sinai Health System in Toronto is a group of 28 gastroenterologists and hepatologists. -

Sinai-Health-System-2019.Pdf
Financial statements of Sinai Health System March 31, 2019 Sinai Health System For the year ended March 31, 2019 Table of contents Independent auditor’s report ...................................................................................................................... 1-3 Statement of financial position ...................................................................................................................... 4 Statement of operations ................................................................................................................................ 5 Statement of changes in net (deficit) assets ................................................................................................. 6 Statement of remeasurement gains and losses .......................................................................................... 7 Statement of cash flows ................................................................................................................................ 8 Notes to the financial statements ............................................................................................................. 9-27 Independent auditor’s report To the Board of Directors of Sinai Health System Our opinion In our opinion, the accompanying financial statements present fairly, in all material respects, the financial position of Sinai Health System (the Organization) as at March 31, 2019 and the results of its operations, its remeasurement gains and losses and its cash flows for the year then ended -

017F HAND V2.Indd
Legc Sini IMPORTANT PLANNING INFORMATION FOR GIFTS IN YOUR WILL If you are considering making a legacy gift, it is important to discuss your plans with your financial or legal advisor as well as with family or loved ones. You are always welcome to contact Sinai Health Foundation, in confidence, so we can ensure your intentions are fulfilled exactly as you wish. When wording your bequest, please note our legal name is: Sinai Health System Foundation. Our charitable registration number is: 119048106 RR0001. SAMPLE WORDING FOR A CHARITABLE BEQUEST Specific Gift to Support Areas of Greatest Need “I give, devise and bequeath to Sinai Health System Foundation, presently located at 1001-522 University Avenue, Toronto, ON M5G 1W7, the sum of $ from my estate to the areas of greatest need.” Residual Gift to Support Areas of Greatest Need “I give, devise and bequeath to Sinai Health System Foundation, presently located at 1001-522 University Avenue, Toronto, ON M5G 1W7, all <OR> % of the rest, residue, and remainder of my estate to the areas of greatest need.” Specific or Residual Gift to Support a Particular Area of Sinai Health System “I give, devise and bequeath to Sinai Health System Foundation, presently located at 1001-522 University Avenue, Toronto, ON M5G 1W7, the sum of $ <OR> %, of my estate <OR> the rest, residue, and remainder of my estate to be used for the following purposes (please choose one): Lunenfeld-Tanenbaum Research Institute; or Specific department or program of Sinai Health System ie: . For more information, please contact: Joy Davidson Executive Director, Gift Planning Sinai Health Foundation Mount Sinai Hospital, Joseph and Wolf Lebovic Health Complex 1001-522 University Avenue, Toronto, ON M5G 1W7 T 416-586-8203 x 5247 F 416-586-8639 [email protected]. -

Memo Template
Today marks the official launch of the new Sinai Health System! Through a voluntary amalgamation that took effect January 1, 2015, Sinai Health System brings together Mount Sinai Hospital and Bridgepoint Active Healthcare. Joining as an affiliate is leading home care and community services provider Circle of Care, extending Sinai Health System’s continuum of care into home and community programs. Together, our vision is to create a premier exemplar of an integrated health system for the future. The Sinai Health System will focus on innovation and integration to address the challenges and opportunities arising from a rapidly aging population and the growing number of people living today with complex health conditions. The new Sinai Health System will combine acute care, complex and rehabilitative care, primary care, home care, and other community-based services to create an integrated continuum of care across the life course, from healthy beginnings to healthy aging. Mount Sinai, Bridgepoint and Circle of Care will work together to create care models for patients who require care from all segments of the system enabling seamless transitions, an improved patient experience and improved outcomes. Bridgepoint and Mount Sinai will operate as one corporation with one board, one management team, one medical staff. We will work as an open system, strengthening existing partnerships, and seeking out new partners to deliver better access to care. While working together as a system, Bridgepoint and Mount Sinai will continue to deliver their excellent programs and services, and retain their names and unique identities. Circle of Care will operate as an affiliate organization, linked into the Sinai Health System at the governance, planning, and system development level.