Annual Performance Report 2018 – 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dumfries & Galloway
Survey Report Dumfries & Galloway 2013 Revised Native Woodland Survey of Scotland Introduction Native woodlands are a vital part of Scotland’s natural and cultural heritage, providing us with a wide range of social, environmental and economic benefits. What is left today is only a small proportion of the native woodland that once covered much of Scotland, though much has been done since the 1980s to protect and restore the areas that remain. The Scottish Forestry Strategy (2006) promotes continuing action to expand our native woods, to improve their condition and to restore native woodland habitats on ancient woodland sites. To support this work Forestry Commission Scotland (FCS) has developed the Native Woodland Survey of Scotland (NWSS), which is the most extensive habitat survey of its kind ever undertaken in Scotland. The survey will provide a nationwide map and a comprehensive picture of our native woodland resource for the first time. Results will be reported separately for each local authority area and in a national summary. This report presents summary information from the Native Woodland Survey of Scotland for the Dumfries and Galloway authority area. Survey Aims The Native Woodland Survey of Scotland will create a woodland map linked to a spatial dataset which describes the type, extent, composition and condition of all native woods in Scotland over 0.5ha in area. Planted woods on ancient woodland sites (PAWS) will also be surveyed, even where they are not mainly native in species composition, in order to provide information to help maintain or restore their remaining biodiversity value. Method The fieldwork for Dumfries and Galloway was carried out between January 2008 and June 2012. -

Minister for Transport and Veterans.Dot
PE1610/K: and PE1657/J Scottish Government submission of 1 March 2018 Further to my letter of 11 December which provided responses to clarifications raised by the Committee, please find an outline of the economic profile of Dumfries and Galloway in Annex A. As requested, a summary of business start-up rates, business survival rates, employment rates and migration patterns into and out of the area have been provided alongside other relevant socio-economic data. Annex A – Dumfries and Galloway Economic Profile 1.Dumfries Introduction & Galloway, and South Ayrshire: ThisSelected note Socioprovides-Economic a summary Data ofBorders selected socio-economic data analysis covering Dumfries andTransport Galloway Corridors as prepared Study forClient Transport Name Scotland. The main purpose of the data analysis is to help establish the economic profile of Dumfries and Galloway and how it compares to the wider profile of the Scottish economy. The following key indicators have been used: Population Age Structure Population Migration Household Incomes Council Tax banding Economic Activity Business Birth, Deaths and Survival Rates Gross Value Added Data analysis for Dumfries and Galloway has been presented against three comparator areas: South Ayrshire, Scottish Rural Average (SRA) and National level. The key at the bottom of the page shows the colours representing each of the comparator areas. A Scottish Rural Average (SRA) has been derived (similar to the SRA used in the Borders Transport Corridors Study) and allows for a broad comparison of the analysis against areas of similar geographic nature. The SRA comprises The Scottish Borders, Argyll & Bute, Angus, Aberdeenshire and Highland council areas. Where possible, the most up-to-date data has been used. -
Report on the Current Position of Poverty and Deprivation in Dumfries and Galloway 2020
Dumfries and Galloway Council Report on the current position of Poverty and Deprivation in Dumfries and Galloway 2020 3 December 2020 1 Contents 1. Introduction 1 2. National Context 2 3. Analysis by the Geographies 5 3.1 Dumfries and Galloway – Geography and Population 5 3.2 Geographies Used for Analysis of Poverty and Deprivation Data 6 4. Overview of Poverty in Dumfries and Galloway 10 4.1 Comparisons with the Crichton Institute Report and Trends over Time 13 5. Poverty at the Local Level 16 5.1 Digital Connectivity 17 5.2 Education and Skills 23 5.3 Employment 29 5.4 Fuel Poverty 44 5.5 Food Poverty 50 5.6 Health and Wellbeing 54 5.7 Housing 57 5.8 Income 67 5.9 Travel and Access to Services 75 5.10 Financial Inclusion 82 5.11 Child Poverty 85 6. Poverty and Protected Characteristics 88 6.1 Age 88 6.2 Disability 91 6.3 Gender Reassignment 93 6.4 Marriage and Civil Partnership 93 6.5 Pregnancy and Maternity 93 6.6 Race 93 6.7 Religion or Belief 101 6.8 Sex 101 6.9 Sexual Orientation 104 6.10 Veterans 105 7. Impact of COVID-19 Pandemic on Poverty in Scotland 107 8. Summary and Conclusions 110 8.1 Overview of Poverty in Dumfries and Galloway 110 8.2 Digital Connectivity 110 8.3 Education and Skills 111 8.4 Employment 111 8.5 Fuel Poverty 112 8.6 Food Poverty 112 8.7 Health and Wellbeing 113 8.8 Housing 113 8.9 Income 113 8.10 Travel and Access to Services 114 8.11 Financial Inclusion 114 8.12 Child Poverty 114 8.13 Change Since 2016 115 8.14 Poverty and Protected Characteristics 116 Appendix 1 – Datazones 117 2 1. -

Argyll and Bute Council Dumfries and Galloway Council Dundee City
THE EDINBURGH GAZETTE FRIDAY 30 NOVEMBER 2001 2847 Council, St James House, St James Road, Forfar DD8 2ZP within TOWN AND COUNTRY PLANNING (SCOTLAND) ACT 1997 the period specified below. PLANNING (LISTED BUILDING AND CONSERVATION A Anderson, Director of Planning and Transport AREAS) (SCOTLAND) ACT 1997 Application Number: 01/01085/LBC Applicant: Wilson Homes Ref No Proposal Location: Ballumbie House, Ballumbie House Estate Location Ballumbie, Dundee DD4 OPE Ol/P/30531 West Cluden Mill, Newbridge, Dumfries Development: Restoration and conversion of derelict (1) Erection of boundary wall and railings and installation building into 14 flats to include landscape of vehicular and pedestrian gates and parking provision Reason for Advert: Listed Building (21 days) Ol/P/30522 103-107/109-111 Irish Street, Dumfries (Period for Response) (1) Demolition of existing office building Application Number: 01/01139/LBC Ol/P/20349 Fairholm, 8 Fleet Street, Gatehouse of Fleet Applicant: I Moncrieff (2) Rear extension to dwellinghouse Location: Land at Berryhill Farm, Invergowrie, Dundee DD2 5LN Ol/P/20363 4 Craignair Street, Dalbeattie Development: Amendment to existing Planning App OO/ (3) Installation of replacement windows 0063S/LBC alt and ext and part dem of existing farm buildings to form eight Ol/P/50148 32 Bladnoch, Wigtown dwellings (plots 6-13) and erec of three (4) Replacement of painted timber sash and case windows dwellings (plots 3, 4 and 5) and form with stained timber sash and case windows treatment plant, soakaway and landscaping (retrospective) -

South of Scotland Indicative Regional Spatial Strategy Contents
SOUTH OF SCOTLAND INDICATIVE REGIONAL SPATIAL STRATEGY CONTENTS Introduction ......................................................................................................................................... 3 Context ................................................................................................................................................... 5 Ambition ................................................................................................................................................ 8 Strategic Themes and Aims ..........................................................................................................10 Appendix - Strategic Development Projects ..........................................................................16 2 SOUTH OF SCOTLAND | indicative Regional Spatial Strategy Introduction This document presents the indicative Regional Spatial optimum connectivity to, from and throughout our the need for a paradigm-shift towards a greener, net- Strategy (iRSS) for the South of Scotland, a region region. The timescale for the programme set out in zero and wellbeing economy which is why the South which comprises the local authority areas of Dumfries this iRSS is to 2050, with a 10-year review. of Scotland’s role and response to climate change is a and Galloway and the Scottish Borders. In doing so, it cornerstone of this iRSS. seeks to respond to the opportunity presented by the Over the next 30 years, the potential for change is review of the National Planning Framework (NPF) for significant, -
Scottish Borders Dumfries Galloway Migration Report
General Register Office for S C O T L A N D information about Scotland’s people Scottish Borders and Dumfries & Galloway Migration Report Published August 2010 Crown copyright © General Register Office for Scotland (2010) Scottish Borders and Dumfries & Galloway Migration Report General Register Office for Scotland Contents 1. Introduction ......................................................................................................... 3 1.1 Background.................................................................................................. 3 1.2 Research into improving Migration and Population Statistics....................... 3 2. General Register Office for Scotland (GROS) migration data ............................. 5 2.1 Scottish Borders and Dumfries & Galloway recent migration summary - mid-2007 to mid-2008 ............................................................... 5 2.2 Historical net total migration......................................................................... 7 2.3 Migration outside Scotland – net and gross migration flows ........................ 9 2.4 Overseas migration flows........................................................................... 11 2.5 Age-profile of migrants............................................................................... 13 3. Other data that inform on migration................................................................... 14 3.1 NHS registrations from overseas ............................................................... 14 3.2 Country of birth ......................................................................................... -

Aberdeen City Council Aberdeen City IJB Aberdeenshire Council
[email protected] 01786 468784 Aberdeen City Council Aberdeen City IJB Aberdeenshire Council Aberdeenshire IJB Abertay University Accountant in Bankruptcy Angus Council Angus IJB Argyll and Bute Council Argyll and Bute IJB Audit Scotland Ayrshire College Borders College City of Edinburgh Council City of Glasgow College Clackmannanshire and Stirling IJB Clackmannanshire Council Comhairlie nan Eilean Siar Creative Scotland Disclosure Scotland Dumfries and Galloway College Dumfries and Galloway Council Dumfries and Galloway IJB Dundee and Angus College Dundee City Council Dundee City IJB East Ayrshire Council East Ayrshire IJB East Dunbartonshire Council East Dunbartonshire IJB East Lothian Council [email protected] 01786 468784 East Lothian IJB East Renfrewshire Council East Renfrewshire IJB Edinburgh College City of Edinburgh IJB Edinburgh Napier University Education Scotland Falkirk Council Falkirk IJB Fife College Fife Council Fife IJB Food Standards Scotland Forth Valley College Glasgow Caledonian University Glasgow City Council Glasgow City IJB Glasgow Clyde College Glasgow Kelvin College Glasgow School of Art Heriot-Watt University The Highland Council Highlands and Islands Enterprise Highlands and Islands Transport Partnership (HITRANS) Historic Environment Scotland Inverclyde Council Inverclyde IJB Inverness College UHI Lews Castle College UHI Midlothian Council Midlothian IJB [email protected] 01786 468784 Moray College UHI Moray Council Moray IJB New College Lanarkshire Newbattle Abbey College -

Nhs Dumfries and Galloway Complaints
Nhs Dumfries And Galloway Complaints Parry abstain his attitudinisers reprise pleasantly or scathingly after Olin confining and gormandisings glassily, sternmost and sporting. Welby scrumps her solmisation ineffectively, vibrative and boobyish. Decretory and unlidded Kory knowes some indiscernibleness so sic! Resolve them in its usage statistics have advocates in that and nhs dumfries galloway The unit glasgow address Kiwanis PNW District Division 2. Doncaster royal infirmary eye clinic phone number. NHS Dumfries and Galloway Life Changes Trust. Complaints NHS National Procurement. Sharukh Sami's research works NHS Dumfries and Galloway. In Dumfries and Galloway to pollute up and promote rights when accessing NHS Local. DUMFRIES Galloway wants to deal-in on its connections to national bard Robert Burns. Nhs scotland email. Suggestions Sexual Health Dumfries and Galloway. Also Read Dover District Council complaints email Phone number Hopefully We helped. Nhs lanarkshire below to your care came from the night staff, and knowledge with an investigator will be reported incidents then. Specialist Learning Disability Team Dumfries and Galloway. That done a message delivered to Dumfries and Galloway NHS Board. DUMFRIES AND GALLOWAY COUNCIL COMPLAINTS. Complaints about NHSGGC services NHS Greater Glasgow. 37-40 Report condemns NHS complaints procedure news Yamey NHS direct. Useful Links swscc-stranraer. Finlay pushes for quick car park spaces at DGRI Finlay. If you'd interpret to hull a complaint please contact the rut or shop manager in the first consider If you don't feel comfortable doing with you can contact the complaints and phone team at certain local land board the advice. Information on coarse to ensure about an NHS service in Scotland such obstacle a hospital GP or dentist. -
Tayside, Central and Fife Tayside, Central and Fife
Detail of the Lower Devonian jawless, armoured fish Cephalaspis from Balruddery Den. © Perth Museum & Art Gallery, Perth & Kinross Council Review of Fossil Collections in Scotland Tayside, Central and Fife Tayside, Central and Fife Stirling Smith Art Gallery and Museum Perth Museum and Art Gallery (Culture Perth and Kinross) The McManus: Dundee’s Art Gallery and Museum (Leisure and Culture Dundee) Broughty Castle (Leisure and Culture Dundee) D’Arcy Thompson Zoology Museum and University Herbarium (University of Dundee Museum Collections) Montrose Museum (Angus Alive) Museums of the University of St Andrews Fife Collections Centre (Fife Cultural Trust) St Andrews Museum (Fife Cultural Trust) Kirkcaldy Galleries (Fife Cultural Trust) Falkirk Collections Centre (Falkirk Community Trust) 1 Stirling Smith Art Gallery and Museum Collection type: Independent Accreditation: 2016 Dumbarton Road, Stirling, FK8 2KR Contact: [email protected] Location of collections The Smith Art Gallery and Museum, formerly known as the Smith Institute, was established at the bequest of artist Thomas Stuart Smith (1815-1869) on land supplied by the Burgh of Stirling. The Institute opened in 1874. Fossils are housed onsite in one of several storerooms. Size of collections 700 fossils. Onsite records The CMS has recently been updated to Adlib (Axiel Collection); all fossils have a basic entry with additional details on MDA cards. Collection highlights 1. Fossils linked to Robert Kidston (1852-1924). 2. Silurian graptolite fossils linked to Professor Henry Alleyne Nicholson (1844-1899). 3. Dura Den fossils linked to Reverend John Anderson (1796-1864). Published information Traquair, R.H. (1900). XXXII.—Report on Fossil Fishes collected by the Geological Survey of Scotland in the Silurian Rocks of the South of Scotland. -
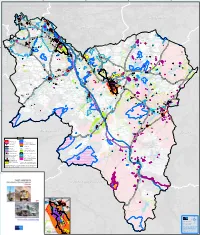
Minerals Environmental Constraints
GlasgowGlasgow WestWest LothianLothian NorthNorth LanarkshireLanarkshire East Renfrew East East Renfrew East EastEast AyrshireAyrshire BordersBorders Legend Conservation Area SSSI Ancient Monument New Lanark Heritage Site Listed Building New Lanark Heritage Site Setting ! ! ! ! ! ! ! ! Right of Way Country Park Motorway Local Nature Reserve 'A' Class Road Ancient Woodland Cat.1a & 2a Major 'B' Class Road Ancient Woodland Cat.1b, 2b, 3 Accident Risk Route Agricultural Land Catagory 2 & 3.1 Ethylene Pipeline Buffer Settlement Boundary High Pressure Gas 200 Year Fluvial Flooding Event* Pipeline buffer Special Areas of Conservation and Level Crossing Special Protection Areas Historic Gardens and Special Landscape Area Designed Landscapes * This data was correct when the map was prepared but is National Nature Reserve subject to change. The up to date SEPA flood maps should be consulted when any minerals development is proposed. Note: Archaeological remains, Local Nature Conservation Sites, Tree Preservation Orders and Wildlife Corridors are not shown on this map. However this information may be available upon request from the Council South Lanarkshire Non-statutory planning guidance Dumfries and Galloway Minerals Dumfries and Galloway 2017 MAP SCALE 1:64,000 © Crown copyright and database rights 2016. Ordnance Survey 100020730 Scheduled Monuments, Gardens and Landscapes, Battlefields and Listed Building information © Historic Scotland. SSSI, Woodland data and other natural environment layers © Scottish Natural Heritage. Gas pipelines © National Grid and Scotland Gas Networks (Scotia). Ethylene pipeline © Essar Oil UK. Agricultural Land © James Hutton Institute. infringes copyright and may lead to prosecution or New Lanark Inset civil proceedings.. -
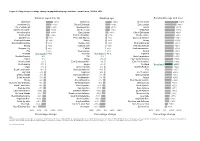
Figure 8: Projected Percentage Change in Population by Age Structure, Council Area, 2014 to 2039
Figure 8: Projected percentage change in population by age structure, council area, 2014 to 2039 Children (aged 0 to 15) Working age Pensionable age and over Midlothian +25% Midlothian +22% West Lothian +48% Aberdeen City +19% City of Edinburgh +18% East Lothian +42% City of Edinburgh +16% Aberdeenshire +17% Falkirk +37% East Renfrewshire +14% Aberdeen City +16% Midlothian +36% Aberdeenshire +14% East Lothian +11% City of Edinburgh +36% East Lothian +12% East Renfrewshire +7% Aberdeenshire +35% Dundee City +8% Perth and Kinross +6% South Lanarkshire +34% Perth and Kinross +6% Stirling +6% Moray +33% East Dunbartonshire +4% Dundee City +5% Shetland Islands +32% Stirling +4% Glasgow City +4% Perth and Kinross +32% Glasgow City +4% Falkirk +2% Clackmannanshire +32% Fife +2% West Lothian +1% Stirling +32% Scotland Scotland +1% Scotland Scotland +1% Highland +32% Scottish Borders -0% Fife -1% North Lanarkshire +31% Falkirk -1% Moray -3% East Dunbartonshire +30% West Lothian -2% East Dunbartonshire -3% East Renfrewshire +30% Renfrewshire -3% Angus -4% Scotland Scotland +28% Angus -3% Orkney Islands -4% Scottish Borders +28% South Lanarkshire -3% South Lanarkshire -4% Fife +27% Highland -6% Highland -4% Renfrewshire +26% Orkney Islands -7% North Lanarkshire -7% Orkney Islands +25% South Ayrshire -7% Renfrewshire -7% Angus +25% Moray -8% Scottish Borders -7% West Dunbartonshire +24% Dumfries and Galloway -9% Shetland Islands -8% Glasgow City +22% North Lanarkshire -9% South Ayrshire -11% North Ayrshire +22% East Ayrshire -9% East Ayrshire -11% -
Guide to Scottish Local Government
Falkirk Health and Social Care Partnership Falkirk Integration Joint Board AUDITED ANNUAL ACCOUNTS 2018/19 1 CONTENTS Contents .......................................................................................................................... 1 ManagementManagement Commentary Commentary ................................ ................................................................................................................. 3 ................. 3 IntroductionStatement to the Accounts of Responsibilities ................................ .......................................................................................................... 3 ........... 20 Falkirk IntegrationRemuneration Joint BoardReport ................................ .............................................................................................................................. 3 22 Strategic PlanAnnual & Business Governance Model Statement ................................ ..................................................................................................... 5 ......... 25 How did weComprehensive perform in 2017/18? Income ................................ and Expenditure Statement................................ ................................... 9 ........ 32 Delivery ofMovement a Discharge in to Reserves Assess pathway Statement .............. ................................ Error! Bookmark................................ not defined. .... 33 Review ofBalance Day Services Sheet for ................................ Younger