A Case Report of Cure of Acromegaly After Pituitary Apoplexy Husain Taha Rhadi*, Ebtihal Yusuf and Eman Ebrahim
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GH/IGF-1 Abnormalities and Muscle Impairment: from Basic Research to Clinical Practice
International Journal of Molecular Sciences Review GH/IGF-1 Abnormalities and Muscle Impairment: From Basic Research to Clinical Practice Betina Biagetti * and Rafael Simó * Diabetes and Metabolism Research Unit, Vall d’Hebron Research Institute and CIBERDEM (ISCIII), Universidad Autónoma de Barcelona, 08193 Bellaterra, Spain * Correspondence: [email protected] (B.B.); [email protected] (R.S.); Tel.: +34-934894172 (B.B.); +34-934894172 (R.S.) Abstract: The impairment of skeletal muscle function is one of the most debilitating least understood co-morbidity that accompanies acromegaly (ACRO). Despite being one of the major determinants of these patients’ poor quality of life, there is limited evidence related to the underlying mechanisms and treatment options. Although growth hormone (GH) and insulin-like growth factor-1 (IGF-1) levels are associated, albeit not indisputable, with the presence and severity of ACRO myopathies the precise effects attributed to increased GH or IGF-1 levels are still unclear. Yet, cell lines and animal models can help us bridge these gaps. This review aims to describe the evidence regarding the role of GH and IGF-1 in muscle anabolism, from the basic to the clinical setting with special emphasis on ACRO. We also pinpoint future perspectives and research lines that should be considered for improving our knowledge in the field. Keywords: acromegaly; myopathy; review; growth hormone; IGF-1 1. Introduction Acromegaly (ACRO) is a rare chronic disfiguring and multisystem disease due to Citation: Biagetti, B.; Simó, R. non-suppressible growth hormone (GH) over-secretion, commonly caused by a pituitary GH/IGF-1 Abnormalities and Muscle tumour [1]. -

Acromegaly Remission, SIADH and Pituitary Function Recovery After Macroadenoma Apoplexy
ID: 19-0057 -19-0057 E Sanz-Sapera and others Apoplexy and remission of ID: 19-0057; July 2019 acromegaly DOI: 10.1530/EDM-19-0057 Acromegaly remission, SIADH and pituitary function recovery after macroadenoma apoplexy Correspondence should be addressed E Sanz-Sapera1, S Sarria-Estrada2, F Arikan3 and B Biagetti1 to B Biagetti Email 1Endocrinology, 2Radiology, and 3Neurosurgery, Vall d’Hebron Hospital, Barcelona, Spain [email protected] Summary Pituitary apoplexy is a rare but potentially life-threatening clinical syndrome characterised by ischaemic infarction or haemorrhage into a pituitary tumour that can lead to spontaneous remission of hormonal hypersecretion. We report the case of a 50-year-old man who attended the emergency department for sudden onset of headache. A computed tomography(CT)scanatadmissionrevealedpituitaryhaemorrhageandthebloodtestconfirmedtheclinicalsuspicionof acromegaly and an associated hypopituitarism. The T1-weighted magnetic resonance imaging (MRI) showed the classic pituitary ring sign on the right side of the pituitary. Following admission, he developed acute-onset hyponatraemia that required hypertonic saline administration, improving progressively. Surprisingly, during the follow-up, IGF1 levels became normal and he progressively recovered pituitary function. Learning points: • Patients with pituitary apoplexy may have spontaneous remission of hormonal hypersecretion. If it is not an emergency, we should delay a decision to undertake surgery following apoplexy and re-evaluate hormone secretion. • Hyponatraemia is an acute sign of hypocortisolism in pituitary apoplexy. However, SIADH although uncommon, could appear later as a consequence of direct hypothalamic insult and requires active and individualised treatment.Forthisreason,closelymonitoringsodiumatthebeginningoftheepisodeandthroughoutthefirst week is advisable to guard against SIADH. • Despite being less frequent, if pituitary apoplexy is limited to the tumour, the patient can recover pituitary function previously damaged by the undiagnosed macroadenoma. -

Acromegaly and the Surgical Treatment of Giant Nose
ARC Journal of Clinical Case Reports Volume 3, Issue 4, 2017, PP 19-21 ISSN No. (Online) 2455-9806 DOI: http://dx.doi.org/10.20431/2455-9806.0304005 www.arcjournals.org Acromegaly and the Surgical Treatment of Giant Nose Lorna Langstaff, MBBS*, Peter Prinsley, MB ChB James Paget University Hospital, Lowestoft Road, NR31 6LA, UK *Corresponding Author: Lorna Langstaff, MBBS, James Paget University Hospital, Lowestoft Road, NR31 6LA, UK, Email: [email protected] Abstract Introduction: The endocrinological changes caused by hyperpituitarism are well managed and reversed. However, the facial changes associated with acromegaly can be permanent and cause distress and concern to patients. Case History: We present the case of an acromegalic women, previously treated for hyperpituitarism, pre- senting with persistent facial changes and a large nose. This was successfully addressed with rhinoplasty, clinical photography is provided. Discussion: The nasal changes associated with acromegaly are challenging but can be successfully treated with rhinoplasty. We discuss the few cases previously mentioned in the literature and the pathophysiology involved in the changes of facial appearance found in acromegalic patients. Keywords: Acromegaly, Giant Nose, Rhinoplasty, Hyperpituitarism Search Strategy: exp “Nasal Bone” or “Nasal Cartilages” or “Nasal Septum” or “Nasal Surgical proce- dure” and Acromegaly or Gigantism or hyperpitu* 1. INTRODUCTION 2. CASE REPORT Acromegaly characteristically causes enlarge- The patient is a 54 year old lady who presented ment of the mandible, zygomatic arches and 10 years after successful treatment for hyperpi- supraorbital ridges, as well as an enlarged nose tuitarism caused by a pituitary adenoma. The and on occasion’s nasal obstruction. -

AACE Guidelines
AACE Guidelines Laurence Katznelson, MD; John L. D. Atkinson, MD; David M. Cook, MD, FACE; Shereen Z. Ezzat, MD, FRCPC; Amir H. Hamrahian, MD, FACE; Karen K. Miller, MD American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice are systematically developed statements to assist health care professionals in medical decision making for specific clinical conditions. Most of the content herein is based on literature reviews. In areas of uncertainty, professional judgment was applied. These guidelines are a working document that reflects the state of the field at the time of publication. Because rapid changes in this area are expected, periodic revisions are inevitable. We encourage medical professionals to use this information in conjunction with their best clinical judgment. The presented recommendations may not be appropriate in all situations. Any decision by practitioners to apply these guidelines must be made in light of local resources and individual patient circumstances. Copyright © 2011 AACE. 1 2 AACE Acromegaly Task Force Chair Laurence Katznelson, MD Departments of Medicine and Neurosurgery, Stanford University, Stanford, California Task Force Members John L. D. Atkinson, MD Department of Neurosurgery, Mayo Clinic, Rochester, Minnesota David M. Cook, MD, FACE Department of Medicine, Oregon Health & Science University, Portland, Oregon Shereen Z. Ezzat, MD, FRCPC Department of Medicine and Endocrinology, Toronto General Hospital, University of Toronto, Toronto, Ontario, Canada Amir H. Hamrahian, MD, FACE Department of Endocrinology, Diabetes and Metabolism, Cleveland Clinic, Cleveland, Ohio Karen K. Miller, MD Neuroendocrine Unit, Department of Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts Reviewers William H. Ludlam, MD, PhD Susan L. Samson, MD, PhD, FACE Steven G. -

Acromegaly Your Questions Answered Patient Information • Acromegaly
PATIENT INFORMATION ACROMEGALY YOUR QUESTIONS ANSWERED PATIENT INFORMATION • ACROMEGALY Contents What is acromegaly? 1 What does growth hormone do? 1 What causes acromegaly? 2 What is acromegaly? Acromegaly is a rare disease characterized by What are the signs and symptoms of acromegaly? 2 excessive secretion of growth hormone (GH) by a pituitary tumor into the bloodstream. How is acromegaly diagnosed? 5 What does growth hormone do? What are the treatment options for acromegaly? 6 Growth hormone (GH) is responsible for growth and development of the human body especially during childhood and adolescence. In addition, Will I need treatment with any other hormones? 9 GH has important functions during later life. It influences fat and glucose (sugar) metabolism, and muscle and bone strength. Growth hormone is How can I expect to feel after treatment? 9 produced in the pituitary gland which is a small bean-sized organ located just underneath the brain (Figure 1). The pituitary gland also secretes How should patients with acromegaly be followed after initial treatment? 9 other hormones into the bloodstream to regulate important functions including reproduction, energy, breast lactation, water balance control, and metabolism. What do I need to do if I have acromegaly? 10 Acromegaly Frequently Asked Questions (FAQs) 10 Glossary inside back cover Pituitary gland Funding was provided by Ipsen Group, Novo Nordisk, Inc. and Pfizer, Inc. through Figure 1. Location of the pituitary gland. unrestricted educational grants. This is the fourth of the series of informational pamphlets provided by The Pituitary Society. Supported by an unrestricted educational grant from Eli Lilly and Company. -

Growth Hormone and Prolactin-Staining Tumors Causing Acromegaly: a Retrospective Review of Clinical Presentations and Surgical Outcomes
CLINICAL ARTICLE J Neurosurg 131:147–153, 2019 Growth hormone and prolactin-staining tumors causing acromegaly: a retrospective review of clinical presentations and surgical outcomes *Jonathan Rick, BS,1 Arman Jahangiri, BS,1 Patrick M. Flanigan, BS,2 Ankush Chandra, MS,3 Sandeep Kunwar, MD,1 Lewis Blevins, MD,1 and Manish K. Aghi, MD, PhD1 1Department of Neurosurgery, University of California, San Francisco, California; 2Cleveland Clinic Lerner College of Medicine, Cleveland, Ohio; and 3Wayne State University School of Medicine, Detroit, Michigan OBJECTIVE Acromegaly results in disfiguring growth and numerous medical complications. This disease is typically caused by growth hormone (GH)–secreting pituitary adenomas, which are treated first by resection, followed by radiation and/or medical therapy if needed. A subset of acromegalics have dual-staining pituitary adenomas (DSPAs), which stain for GH and prolactin. Presentations and treatment outcomes for acromegalics with DSPAs are not well understood. METHODS The authors retrospectively reviewed the records of more than 5 years of pituitary adenomas resected at their institution. Data were collected on variables related to clinical presentation, tumor pathology, radiological size, and disease recurrence. The Fisher’s exact test, ANOVA, Student t-test, chi-square test, and Cox proportional hazards and multiple logistic regression were used to measure statistical significance. RESULTS Of 593 patients with pituitary adenoma, 91 presented with acromegaly. Of these 91 patients, 69 (76%) had tumors that stained for GH only (single-staining somatotrophic adenomas [SSAs]), while 22 (24%) had tumors that stained for GH and prolactin (DSPAs). Patients with DSPAs were more likely to present with decreased libido (p = 0.012), signs of acromegalic growth (p = 0.0001), hyperhidrosis (p = 0.0001), and headaches (p = 0.043) than patients with SSAs. -
Acromegaly with Empty Sella Syndrome
ID: 21-0049 -21-0049 R Daya and others Acromegaly with empty sella ID: 21-0049; July 2021 syndrome DOI: 10.1530/EDM-21-0049 Acromegaly with empty sella syndrome Reyna Daya1,2 , Faheem Seedat 1,2, Khushica Purbhoo3, Saajidah Bulbulia1,2 and Zaheer Bayat1,2 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Helen Joseph Hospital, Rossmore, Johannesburg, South Africa, 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Faculty of Correspondence Health Sciences, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa, and should be addressed 3Department of Nuclear Medicine and Molecular Imaging, Chris Hani Baragwanath Academic Hospital and Charlotte to F Seedat Maxeke Johannesburg Academic Hospital, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, Email South Africa [email protected] Summary Acromegaly is a rare, chronic progressive disorder with characteristic clinical features caused by persistent hypersecretion of growth hormone (GH), mostly from a pituitary adenoma (95%). Occasionally, ectopic production of GH or growth hormone-releasing hormone (GHRH) with resultant GH hypersecretion may lead to acromegaly. Sometimes localizing thesourceofGHhypersecretionmayprovedifficult.Rarely,acromegalyhasbeenfoundinpatientswithanemptysella (ES) secondary to prior pituitary radiation and/or surgery. However, acromegaly in patients with primary empty sella (PES) is exceeding rarely and has only been described in a few cases. We describe a 47-year-old male who presented with overt features of acromegaly (macroglossia, prognathism, increased hand and feet size). Biochemically, both the serum GH (21.6 μg/L) and insulin-like growth factor 1 (635 μg/L) were elevated. In addition, there was a paradoxical elevation of GH following a 75 g oral glucose load. -

Guidance on the Treatment of Antipsychotic Induced Hyperprolactinaemia in Adults
Guidance on the Treatment of Antipsychotic Induced Hyperprolactinaemia in Adults Version 1 GUIDELINE NO RATIFYING COMMITTEE DRUGS AND THERAPEUTICS GROUP DATE RATIFIED April 2014 DATE AVAILABLE ON INTRANET NEXT REVIEW DATE April 2016 POLICY AUTHORS Nana Tomova, Clinical Pharmacist Dr Richard Whale, Consultant Psychiatrist In association with: Dr Gordon Caldwell, Consultant Physician, WSHT . If you require this document in an alternative format, ie easy read, large text, audio, Braille or a community language, please contact the Pharmacy Team on 01243 623349 (Text Relay calls welcome). Contents Section Title Page Number 1. Introduction 2 2. Causes of Hyperprolactinaemia 2 3. Antipsychotics Associated with 3 Hyperprolactinaemia 4. Effects of Hyperprolactinaemia 4 5. Long-term Complications of Hyperprolactinaemia 4 5.1 Sexual Development in Adolescents 4 5.2 Osteoporosis 4 5.3 Breast Cancer 5 6. Monitoring & Baseline Prolactin Levels 5 7. Management of Hyperprolactinaemia 6 8. Pharmacological Treatment of 7 Hyperprolactinaemia 8.1 Aripiprazole 7 8.2 Dopamine Agonists 8 8.3 Oestrogen and Testosterone 9 8.4 Herbal Remedies 9 9. References 10 1 1.0 Introduction Prolactin is a hormone which is secreted from the lactotroph cells in the anterior pituitary gland under the influence of dopamine, which exerts an inhibitory effect on prolactin secretion1. A reduction in dopaminergic input to the lactotroph cells results in a rapid increase in prolactin secretion. Such a reduction in dopamine can occur through the administration of antipsychotics which act on dopamine receptors (specifically D2) in the tuberoinfundibular pathway of the brain2. The administration of antipsychotic medication is responsible for the high prevalence of hyperprolactinaemia in people with severe mental illness1. -
The First Case Report of a Patient with Coexisting Acromegaly with Adrenocorti- Cal Cushing and Pheochromocytoma
Central Journal of Endocrinology, Diabetes & Obesity Bringing Excellence in Open Access Case Report *Corresponding author Semin Fenkci, M.D. Mehmetcik M, 1298 Sok, No: 44, Laodikya Apt, A Blok, Daire: 4, 20100, Denizli, Turkey The First Case Report of A Patient Submitted: 04 January 2019 Accepted: 04 February 2019 with Coexisting Acromegaly Published: 06 February 2019 ISSN: 2333-6692 Copyright with Adrenocortical Cushing and © 2019 Fenkci et al. Pheochromocytoma OPEN ACCESS Keywords 1 2 3 1 Semin Fenkci , Nagehan Yalcin , Ergin Sagdas , Senay Topsakal , and • Acromegaly Guzin F. Yaylali1 • Cortical adenoma 1Departments of Endocrinology and Metabolism, Pamukkale University, School of Medicine, • Cushing Syndrome Denizli, Turkey • Pheochromocytoma 2Department of Pathology, Pamukkale University, School of Medicine, Denizli, Turkey 3Department of Radiology, Pamukkale University, School of Medicine, Denizli, Turkey Abstract Pheochromocytoma [PHEO] and Cushing syndrome [CS] may sometimes coexist and very rarely originate from the same adrenal gland. There were 12 cases in the literature in which corticomedullary involvement has been reported. A few cases of primary aldosteronism coexisting with Pheochromocytomahave been reported so far. Also there is very little information about pheochromocytoma associated with Cushing’s syndrome. Cushing’s syndrome secondary to ectopic adrenocorticotropic hormone [ACTH] secretion has been frequently reported nowadays. Our literature search revealed no previous reports of a patient with PHEO and CS originating from the same adrenal gland and coexistent with acromegaly. INTRODUCTION absent menstrual periods,easy bruising, purple striae, acne and hirsutism. BMI was calculated as 26.95kg/m2. Adrenal lesion composed of a mixture of different cell types derived from both pheochromocytes and cortical cells, which do The baseline C peptide level was 2.4 ng/mL, anti-gad and anti- not share a common embryological origin [1]. -
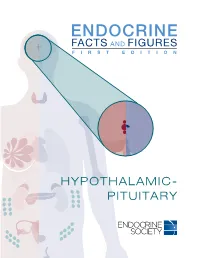
Hypothalamic- Pituitary Cost Burden Prevalence
HYPOTHALAMIC- PITUITARY COST BURDEN PREVALENCE ACROMEGALY AFFECTS $13,708 78 AMERICANS PER MILLION PER YEAR US ANNUAL COST OF NON-FUNCTIONING FOR EVERY 1,000,000 FOR EVERY 1,000,000 PITUITARY ADENOMAS OLDER ADULTS (≥65 YEARS) CHILDREN (0-17 YEARS) PER PATIENT IN 20083 $24,900 148-182 29-37 US AVERAGE CASES1 CASES1 ANNUAL COST OF ACROMEGALY PER PATIENT4 HYPOPITUITARISM AFFECTS <200,000 AMERICANS2 SEX DIFFERENCES PROLACTINOMAS Source: 1 Burton, T.; Le Nestour E.; Neary, M.; Ludlam, WH. Incidence and prevalence of acromegaly in a large US health plan database. Pituitary. 2016. 2 Corenblum B. Hypopituitarism. 2011; http://emedicine.medscape.com/article/122287- overview#a0101. Accessed June 3, 2015. 3 Swearingen, B.; Wu, N.; Chen, S.Y.; Bulgar S.; Biller, B.M. Health care resource use and costs among patients with cushing disease. Endocrine Practice: official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2011;17(5):681-690. 10x 4 Broder, M.S.; Neary M.P.; Chang, E.; Cherepanov, D.; Katznelson, L. Treatments, complications, MORE COMMON IN and healthcare utilization associated with acromegaly: a study in two large United States databases. Pituitary. 2014;17(4):333-341. FEMALES AGE 20-50 5 Casanueva, F.F.; Molitch, M.E.; Schlechte, J.A.; et al. Guidelines of the Pituitary Society for the YEARS THAN MALES5 diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006;65(2):265-273. © 2016 The Endocrine Society. All rights reserved. Endocrine Society 2055 L Street NW, Suite 600 -

Development of Acromegaly in Patients with Prolactinomas
European Journal of Endocrinology (2003) 149 17–22 ISSN 0804-4643 CLINICAL STUDY Development of acromegaly in patients with prolactinomas Marianne Andersen, Casper Hagen, Jan Frystyk1, Henrik Daa Schroeder2 and Claus Hagen Department of Endocrinology, Odense University Hospital, 5000 Odense C, Denmark, 1Medical Research Laboratory, Institute of Experimental and Clinical Research, University Hospital of Aarhus, DK-8000 Aarhus, Denmark and 2 Department of Pathology, Odense University Hospital, Denmark (Correspondence should be addressed to Marianne Andersen; Email: [email protected]) Abstract Objectives: Patients with prolactinomas and patients with acromegaly often have heterogenous adeno- mas. In this study we have focused on patients with prolactinomas who developed acromegaly and acromegalic patients with hyperprolactinaemia. Our hypothesis is that some patients with hyperpro- lactinaemia may develop clinical acromegaly. Methods: We have included patients examined at department M, Odense University Hospital between 1996 and 2001. Seventy-eight patients with prolactinomas, 65 females and 13 males, with a median age (range) of 30 years (14–74) and 47 years (20–66), respectively, were included in the study. Results: In females and males the median prolactin (PRL) levels were 90 mg/l (27–4700; normal values (NV) #23) and 1075 mg/l (24–6500; NV #14), respectively. The PRL levels were significantly higher in males compared with females (P , 0.002). Fifty-nine patients with acromegaly, 24 females and 35 males, with a median age (range) of 45 years (24–70) and 53 years (19–70), respectively, were included. Seven of the 24 females had hyperprolactinaemia, with PRL levels of 90 mg/l (27– 494). Thirteen of the 35 males had hyperprolactinaemia with PRL levels of 47 mg/l (17–251). -

GH Deficiency in Patients Irradiated for Acromegaly
European Journal of Endocrinology (2006) 154 851–858 ISSN 0804-4643 CLINICAL STUDY GH deficiency in patients irradiated for acromegaly: significance of GH stimulatory tests in relation to the 24 h GH secretion A A van der Klaauw1, A M Pereira1, S W van Thiel1, J W A Smit1, E P M Corssmit1, N R Biermasz1, M Frolich2, A Iranmanesh3, J D Veldhuis4, F Roelfsema1 and J A Romijn1 Departments of 1Endocrinology and Metabolism, C4-R, and 2Clinical Chemistry, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, The Netherlands, 3Endocrine Service, Research and Development, Salem Veterans Affairs Medical Center,Salem, Virginia 24153, USA and 4Endocrine Research Unit, Department of Internal Medicine, Mayo School of Graduate Medical Education, General Clinical Research Center, Mayo Clinic, Rochester, Minnesota 55905, USA (Correspondence should be addressed to F Roelfsema; Email: [email protected]) Abstract Background: Radiotherapy for pituitary adenomas frequently leads to GH deficiency (GHD). The characteristics of GH secretion in GHD induced by postoperative radiotherapy for acromegaly are not known. Hypothesis: In the long term, stimulated and spontaneous GH release is not different between patients with GHD treated by postoperative radiotherapy for acromegaly or for other pituitary adenomas. Design/subjects: We compared the characteristics of basal and stimulated GH secretion in patients with GHD, who had previously received adjunct radiotherapy after surgery for GH-producing adenomas (nZ10) vs for other pituitary adenomas (nZ10). All patients had a maximal GH concentration by insulin tolerance test (ITT) of 3 mg/l or less, compatible with severe GHD. Mean time after radiation was 17 and 18.7 years, respectively.