MINUTES from the MEETING of the STATE EMPLOYEE BENEFITS COMMITTEE August 17, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Informational Brochure
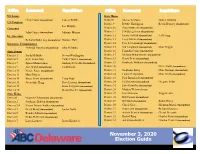
US Senate State House Chris Coons (incumbent) Lauren Witzke District8 Sherae’A Moore Daniel Zitofsky US Congress District 9 Debbie Harrington Kevin Hensley (incumbent) Lee Murphy Governor District 10 Sean Matthews (incumbent) John Carney (incumbent) Julianne Murray District 11 Jeff Spiegelman (incumbent) Lt. Governor District 12 Krista Griffith (incumbent) Jeff Cragg Bethany Hall-Long (incumbent) Donyale Hall District 13 Larry Mitchell (incumbent) Insurance Commissioner District 14 Pete Schwartzkopf (incumbent) Trinidad Navarro (incumbent) Julia Pillsbury District 15 Val Longhurst (incumbent) Mike Higgin State Senate District 16 Franklin Cooke (incumbent) District 1 Sarah McBride Steven Washington District 17 Melissa Minor-Brown (incumbent) District 5 Kyle Evans Gay Cathy Cloutier (incumbent) District 18 David Benz (incumbent) District 7 Spiros Mantzavinos Anthony Delcollo (incumbent) District 19 Kimberly Williams (incumbent) District 9 Jack Walsh (incumbent) Todd Ruckle District 20 Steve Smyk (incumbent) District 12 Nicole Poore (incumbent) District 21 Stephanie Barry Mike Ramone (incumbent) District 13 Mary Pinkey District 22 Luann D’Agostino Mike Smith (incumbent) District 14 Bruce Ennis (incumbent) Craig Pugh District 23 Paul Baumbach (incumbent) District 15 Jacqueline Hugg Dave Lawson (incumbent) District 24 Ed Osienski (incumbent) Gregory Wilps District 19 Brian Pettyjohn (incumbent) District 25 John Kowalko (incumbent) District 20 Gerald Hocker (incumbent) District 26 Madina Wilson-Anton State House District 27 Eric Morrison Tripp -

Insurance and Workers' Compensation Department
Insurance and Workers’ Compensation Department Information State Chart This Insurance and Workers’ Compensation Department Information State Chart provides contact information for insurance and workers’ compensation departments for all 50 states and the District of Columbia. For state rate and form filing requirements, see Rate and Form Filing Requirements State Chart. State Insurance Department Worker’s Compensation Department Alabama Alabama Department of Insurance Alabama Department of Labor, Workers’ Compensation Division Contact Information Contact Information Commissioner: Jim L. Ridling Workers’ Compensation Division Directory Alaska Alaska Division of Insurance Alaska Department of Labor and Workforce Development, Division of Workers’ Contact Information Compensation Director: Lori Wing-Heier Contact Information Workers’ Compensation Board Arizona Arizona Department of Insurance Industrial Commission of Arizona, Claims Division Contact Information Contact Information Interim Director: Keith A. Schraad Claims Manager Arkansas Arkansas Insurance Department Arkansas Workers’ Compensation Commission Contact Information Contact Information Commissioner: Alan Kerr Commissioners California California Department of Insurance California Department of Industrial Relations, Division of Workers' Compensation Contact Information Contact Information Commissioner: Dave Jones Commission on Health and Safety and Workers' Compensation Colorado Colorado Department of Regulatory Colorado Department of Labor and Agencies, Division of Insurance Employment, -

Bank Breaks Election Ground Profiles Organization Meet the Candidates Looks to Expand in Tuesday's Election Mission with New Pg
, : POliTICS Food bank breaks Election ground profiles Organization Meet the candidates looks to expand in Tuesday's election mission with new Pg. 10 13 headquarters By JOSH SHANNON FIRE [email protected] When the Food Bank of Delaware opens its new warehouse around this time next year, its goal goes far beyond just having more storage space. Instead, President and CEO Patricia NEWARK POST PHOTO BY KARlE SIMMONS Beebe seeks a fundamen Dominic Lalite, 7, and 4-year-old Charles Simmons IV, of Newark, gaze into the mirrored sphere at the entrance to H!gh Five Park tal shift in the way the state in Glasgow Park. The new playground is geared toward children with autism, but anyone is welcome to play there. deals with hunger. "We're going to be advocat ing systemic change," Beebe Glasgow Par~ playground geared toward kids with autism said during a groundbreak ing ceremony at the new fa On hurt By KARlE SIMMONS sive park tailored to the needs of autis their daughter Delia, could play. cility in Pencader Corporate [email protected] tic children. They pitched the idea to County Center on Oct 20. The playground, which lies within Councilman David Tackett, who then "1his 25-acre campus will in blaze What started as a father's phone call Glasgow Park behind the main pavilion, brought it to County Executive Tom become part of the solution to two years ago, ended last week with is the brainchild of Glasgow parents Gordon. ending hunger in Delaware." RobscoH Manor home his daughter's smile as she watched Elizabeth and Rob Scheinberg, who no New Castle County leaders open ticed the county lacked a place where See PLAYGROUND See FOOD BANK damaged by fire H!GH 5 Park - Delaware's first inclu- children on the autism spectrum, like Page A15 Page A6 Pg. -

State of Delaware Statewide Benefits Office
MINUTES FROM THE MEETING OF THE STATE EMPLOYEE BENEFITS COMMITTEE DECEMBER 14, 2020 The State Employee Benefits Committee (the “Committee”) met at 2:00 p.m. on December 14, 2020. In accordance with the Proclamation Authorizing Public Bodies to Meet Electronically and in the interests of protecting the citizens of this State from the public health threat caused by COVID-19, this meeting was conducted via WebEx, without a physical location. Committee Members Represented or in Attendance: Director Michael Jackson, Office of Management & Budget (“OMB”), (Co-Chair) Secretary Saundra Johnson, Department of Human Resources (“DHR”), Co-Chair The Honorable Bethany Hall-Long, Lieutenant Governor The Honorable Trinidad Navarro, Insurance Commissioner Secretary Molly Magarik, Department of Health & Social Services (“DHSS”) Ms. Victoria Brennan, Senior Legislative Analyst, Office of the Controller General Mr. Steven Costantino, Dir. Of Health Care Reform, DHSS Mr. Jeff Taschner, Executive Director, Delaware State Education Association (Appointee of the Governor) Ms. Ashley Tucker, Staff Attorney, Administrative Office of the Courts (Designee OBO The Honorable Collins Seitz, Chief Justice, Delaware Supreme Court) Committee Members Represented or in Attendance: The Honorable Colleen Davis, State Treasurer, Office of the State Treasurer Others in Attendance: Dir. Faith Rentz, Statewide Benefits Office (“SBO”), DHR Ms. Nina Figueroa, Health Policy Advisor, SBO, DHR Deputy Director Leighann Hinkle, SBO, DHR Mr. Bryan Hammons, ESI Deputy Attorney General, Andrew Kerber, Dept. of Ms. Sandy Hart, IBM Watson Health Justice, SEBC Legal Counsel Ms. Marie Hartigan, SBO, DHR Mr. Chris Giovannello, Willis Towers Watson (“WTW”) Ms. Charlene Hrivnak, CVS Health Ms. Jaclyn Iglesias, WTW Ms. Katherine Impellizzeri, Aetna Ms. -

State Insurance Commissioner Contact Information
State Insurance Commissioner Contact Information State insurance commissioners play an important role in guiding state-based insurance regulation and overseeing insurer pricing and activities in their states. While each state’s process is different, reporting health insurance-related issues to your state insurance commissioner is a useful tool in patients’ arsenal. Alabama Delaware Jim L. Ridling Trinidad Navarro 334-241-4141 800-282-8611 Online Form [email protected] Alaska Florida Lori Wing-Heier David Altmaier 907-269-7900 850-413-3140 [email protected] [email protected] Arizona Georgia Keith A. Schraad, J.D. John F. King 602-364-2499 800-656-2298 [email protected] [email protected] Arkansas Hawaii Allen Kerr Colin M. Hayashida 501-371-2600 808-586-2790 [email protected] [email protected] California Idaho Ricardo Lara Dean Cameron 800-927-4357 800-721-3272 Online Form Online Form Colorado Illinois Michael Conway Robert H. Muriel 303-894-7499 217-782-4515 Online Form [email protected] Connecticut Indiana Andrew N. Mais Steve Robertson 800-203-3447 317-232-2385 Online Form [email protected] 1 Iowa Doug Ommen Mississippi 877-955-1212 Mike Chaney Online Form 601-359-1077 [email protected] Kansas Vicki Schmidt Missouri 800-432-2484 Chlora Lindley-Myer [email protected] 800-726-7390 [email protected] Kentucky Nancy G. Atkins Montana 502-564-6034 Matt Rosendale Online Form 800-332-6148 Online Form Louisiana Jim Donelon Nebraska 800-259-5300 Bruce R. Ramge Online Form 402-471-2201 [email protected] Maine Eric Cioppa Nevada 800-300-5000 Barbara Richardson [email protected] 888-872-3234 Online Form Maryland Al Redmer New Hampshire 800-492-6116 John R. -

A Listing of Delaware Elected Officials Compiled by the League of Women Voters As a Public Service (302) 571-8948
(Subject to change 6/17/2021) They Represent You 2020-2022 (Revision III) A listing of Delaware elected officials compiled by the League of Women Voters of Delaware, Inc. as a public service (302) 571-8948 United States Party/ Name Address Office Telephone E-mail Address Term Expires President (D) Joseph R. Biden, Jr. The White House (202) 456-6213 Comment line (4 Yrs.) 2024 1600 Pennsylvania Ave. NW (202) 456-1414 www.whitehouse.gov/contact Vice President (D) Kamala Harris Washington, DC 20500 (202) 456-1414 (4 Yrs.) 2024 www.whitehouse.gov/administration/vice-president-harris Senators (D) Thomas R. Carper 513 Hart Senate Office Bldg. (202) 224-2441 DC (6 Yrs.) 2024 Washington, DC 20510 (302) 573-6291 NC Carper.Senate.gov (contact via web page) (302) 674-3308 K (302) 856-7690 S (D) Christopher A. Coons 127 A Russell Senate Office Bldg. (202) 224-5042 DC (6 Yrs.) 2026 Washington, DC 20510 (302) 573-6345 NC Coons.Senate.gov/contact (302) 736-5601 K &S chriscoons.com Representative (D) Lisa Blunt Rochester 1519 Longworth House Office Bldg. (202) 225-4165 DC bluntrochester.house.gov (2 Yrs.) 2022 Washington, DC 20515 (302) 830-2330 NC (contact via web page) (302) 858-4773 SC State Party/Name Address (Area code for DE is 302) Office Telephone E-mail Address Term Expires Governor (D) John C. Carney, Jr. 150 Martin Luther King Jr., Blvd. South 1-800 292-9570 [email protected] (4 Years) 2024 Dover, DE 19901 744-4101 K 577-3210 NC Lt. Governor (D) Bethany A. -

ALABAMA - DEPARTMENT of INSURANCE 201 Monroe Street, Suite 502
ALABAMA - DEPARTMENT OF INSURANCE 201 Monroe Street, Suite 502 Montgomery Alabama 36104 United States Phone: 334-269-3550 Web: http://www.aldoi.gov Description: Jim L. Ridling, Commissioner of Insurance ALASKA - DEPARTMENT OF INSURANCE 550 West 7th Avenue, Suite 1560 Anchorage Alaska 99501-3567 United States Phone: 907-269-7900 Web: https://www.commerce.alaska.gov/web/ins/ Description: Lori K. Wing-Heier, Director of Insurance ARIZONA - DEPARTMENT OF INSURANCE 100 N. 15th Avenue, Suite 261 Phoenix Arizona 85007-2630 United States Phone: 602-364-3100 Web: https://insurance.az.gov/ Description: Evan G. Daniels, Director of Insurance and Financial Institutions ARKANSAS - DEPARTMENT OF INSURANCE 1 Commerce Way Little Rock Arkansas 72202 United States Phone: 501-371-2600 Web: https://insurance.arkansas.gov/ Description: Alan McClain, Commissioner of Insurance CALIFORNIA - DEPARTMENT OF INSURANCE 300 South Spring Street, South Tower Los Angeles California 90013 United States Phone: 800-927-4357 Web: http://www.insurance.ca.gov Description: Ricardo Lara, Commissioner of Insurance COLORADO - DEPARTMENT OF INSURANCE 1560 Broadway, Suite 850 Denver Colorado 80202 United States Phone: 303-894-7499 Web: https://doi.colorado.gov/ Description: Michael Conway, Commissioner of Insurance CONNECTICUT - DEPARTMENT OF INSURANCE 153 Market Street, 7th Floor Hartford Connecticut 06103 United States Phone: 860-297-3900 Web: https://portal.ct.gov/cid Description: Andrew N. Mais, Commissioner of Insurance DELAWARE - DEPARTMENT OF INSURANCE 1351 West North Street, Suite 101 Dover Delaware 19904 United States Phone: 302-674-7300 Web: https://insurance.delaware.gov/ Description: Trinidad Navarro, Commissioner of Insurance DISTRICT OF COLUMBIA - DEPARTMENT OF INSURANCE 1050 First Street, NE, 801 Washington District Of Columbia 20002 United States Phone: 202-727-8000 Web: http://www.disb.dc.gov Description: Karima M. -

Insurance Commissioner's Consumer Services Division
State Insurance Commissioner Contact Information State insurance commissioners play an important role in guiding state-based insurance regulation and overseeing insurer pricing and activities in their states. While each state’s process is different, reporting health insurance-related issues to your state insurance commissioner is a useful tool in patients’ arsenal. Alabama Delaware Jim L. Ridling Trinidad Navarro 334-241-4141/ 1-800-433-3966 (302) 674-7310/800-282-8611 [email protected] [email protected] Alaska Florida Lori Wing-Heier David Altmaier 907-269-7900/1-800-INSURAK 850-413-3140 [email protected] [email protected] Arizona Georgia Evan G. Daniels John F. King 602-364-2499 (404) 656-2070/800-656-2298 [email protected] Online Form Arkansas Hawaii Alan McClain Colin M. Hayashida 501-371-2640/800-852-5494 808-586-2790 [email protected] [email protected] California Idaho Ricardo Lara Dean Cameron 800-927-4357 800-721-3272 Online Form Online Form Colorado Illinois Michael Conway Dana Popish Severinghaus 303-894-7499 866-445-5364 [email protected] [email protected] Connecticut Indiana Andrew N. Mais Steve Robertson 800-203-3447 317-232-2395 [email protected] [email protected] 1 Iowa Doug Ommen Mississippi 515-654-6600/877-955-1212 Mike Chaney Online Form 601-359-3569/800-562-2957 [email protected] Kansas Vicki Schmidt Missouri 800-432-2484 Chlora Lindley-Myer [email protected] 800-726-7390 [email protected] Kentucky Sharon P. Clark Montana 502-564-6034/800-595-6053 Troy Downing [email protected] 800-332-6148 Online Form Louisiana Jim Donelon Nebraska (225) 342-5900/800-259-5300 Eric Dunning Online Form 402-471-0888/877-564-7323 [email protected] Maine Eric Cioppa Nevada 207-624-8475/800-300-5000 Barbara Richardson [email protected] 888-872-3234 Online Form Maryland Kathleen A. -

Election Guide Was Created President-Elect RON MACARTHUR PHOTO Day
A special publication by 2 DATEOCTOBER 28 - NOVEMBER 8, 2016 ELECTION #GUIDE 2016 Cape Gazette DELAWARE PUBLIC ARCHIVES PHOTO A RARE DOCUMENT shows coun- ty election returns from 1811. Until 1812, all voting took place in the coun- ty seat Georgetown. Return Day trivia • John M. Clayton of Dags- boro, a U.S. senator and U.S. secretary of state in President Zachery Taylor’s administra- MANY HAPPY tion, put Return Day in per- spective in the mid-1800s. He said “that the man who had been to a political meeting in RETURNS Dagsboro, seen Return Day in Georgetown and visited Paris had witnessed the three most interesting sights in the world” • While there are no records of a president participating in the parade, in 2008 then Vice President-Elect Joe Biden rode in a carriage with his wife, Jill, on the rain soaked streets of Georgetown. That year’s event CLOCKWISE, FROM TOP: Town crier Kirk Lawson reads re- was like no other in history, turns from the 2014 election; Sussex County party leaders, in a complete with metal-detector photo from 1988, Republican J. Everett Moore, Libertarian Bob security checks, Secret Service Sigler and Democrat Ken McDowell prepare to bury the hatch- and sharpshooters et; a historical marker on The Circle explains the unique histo- ry of the one-of-a-kind event in the country; and each Return Day, officials of each political party gather to bury the hatchet • In 1965, the Delaware Gen- in Lewes Beach sand. eral Assembly declared Return PHOTOS: DELAWARE PUBLIC ARCHIVES AND RON MACARTHUR Day as a legal half-day holiday in Sussex County • W. -

State Title Name Phone Number Email Address Alabama Commissioner Jim L
State Title Name Phone Number Email Address Alabama Commissioner Jim L. Ridling 334-269-3550 [email protected] Alaska Director Lori K. Wing-Heier 907-269-7900 [email protected] Arizona Interim Director Leslie R. Hess 602-364-3100 [email protected] Arkansas Commissioner Allen W. Kerr 501-371-2600 [email protected] California Commissioner Dave Jones 916-492-3500 [email protected] Colorado Commissioner Marguerite Salazar 303-894-7499 [email protected] Connecticut Commissioner Katharine L. Wade 860-297-3800 [email protected] Delaware Commissioner Trinidad Navarro 302-674-7300 [email protected] D.C. Commissioner Stephen C. Taylor 202-727-8000 [email protected] Florida Commissioner David Altmaier 850-413-5914 [email protected] Georgia Commissioner Ralph T. Hudgens 404-656-2070 [email protected] Hawaii Commissioner Gordon I. Ito 808-586-2790 [email protected] Idaho Director Dean L. Cameron 208-334-4250 [email protected] Illinois Director Jennifer Hammer 217-782-4515 [email protected] Indiana Commissioner Stephen W. Robertson 317-232-2385 [email protected] Iowa Commissioner Doug Ommen 515-281-5575 [email protected] Kansas Commissioner Ken Selzer 785-296-3071 [email protected] Kentucky Commissioner Nancy G. Atkins 502-564-3630 [email protected] Louisiana Commissioner James J. Donelon 225-342-5900 [email protected] Maine Superintendent Eric A. Cioppa 207-624-8475 [email protected] Maryland Commissioner Al Redmer Jr. 410-468-2090 [email protected] Massachusetts Commissioner Gary Anderson 617-521-7794 [email protected] Michigan Director Patrick M. -

Commission Member States
Commission Member States Alabama, Commissioner Jim L. Ridling Alaska, Director Lori K. Wing-Heier Arizona, Director Evan G. Daniels Arkansas, Commissioner Alan McClain Colorado, Commissioner Michael Conway Connecticut, Commissioner Andrew N. Mais Delaware, Commissioner Trinidad Navarro District of Columbia, Commissioner Karima Woods Georgia, Commissioner John F. King Hawaii, Commissioner Colin M. Hayashida Idaho, Director Dean L. Cameron Illinois, Director Dana Popish Severinghaus Indiana, Commissioner Amy Beard Iowa, Commissioner Doug Ommen Kansas, Commissioner Vicki Schmidt Kentucky, Commissioner Sharon P. Clark Louisiana, Commissioner James J. Donelon Maine, Superintendent Eric A. Cioppa Maryland, Commissioner Kathleen A. Birrane Massachusetts, Commissioner Gary D. Anderson Michigan, Director Anita Fox Minnesota, Commissioner Grace Arnold Mississippi, Commissioner Mike Chaney Missouri, Director Chlora Lindley-Myers Montana, Commissioner Troy Downing Nebraska, Director Eric Dunning Nevada, Commissioner Barbara Richardson New Hampshire, Commissioner Chris Nicolopoulos New Jersey, Commissioner Marlene Caride New Mexico, Superintendent Russell Toal North Carolina, Commissioner Mike Causey Ohio, Director Judith French Oklahoma, Commissioner Glen Mulready Oregon, Commissioner Andrew Stolfi Pennsylvania, Commissioner Jessica K. Altman Puerto Rico, Commissioner Mariano A. Mier Romeu Rhode Island, Superintendent Elizabeth Kelleher Dwyer South Carolina, Director Raymond G. Farmer Tennessee, Commissioner Carter Lawrence Texas, Chief Deputy Commissioner Doug Slape Utah, Commissioner Jonathan Pike Vermont, Commissioner Michael S. Pieciak Virginia, Commissioner Scott A. White Washington, Commissioner Mike Kreidler West Virginia, Commissioner James A. Dodrill Wisconsin, Commissioner Mark Afable Wyoming, Commissioner Jeff Rude . -

Chamber Connections, October 2016Chamber Connections, October 2016
onnectionsChamber CVol. 40, No. 10 October 2016 The CDCC Annual Holiday Gift Auction The 13th Annual Holiday Gift Auc- tion is presenting our members’ fin- est services and products! This is the largest fundraiser for the Central Del- aware Chamber of Commerce (CDCC), and we want to open the doors on Wednesday October 26, 2016 at Maple Dale Country Club (5:00pm-9:00pm) to Heather YOU, our members and your guests to Pleasants joins an evening of premier, unique and ex- clusive offerings! Join us for an evening the CDCC staff of... Holiday Gift Shopping Military Affairs Chair Lynne Schaefer introduces Senator Tom Carper at the 2015 MilCon Breakfast. .................................Pages 3 Networking Appetizers & Cash Bar MilCon Breakfast at Dover AFB IN THIS ISSUE... to be held in November Candidate Interviews The Central Delaware Chamber of ..........................................6-12 Commerce Military Affairs Commit- tee and Dover Air Force Base invite you to attend the MilCon Breakfast LCD Retreat brought to you by Signature Spon- .............................................13 sor Delaware Technical Communi- ty College in partnership with Dis- Who is invited? All CDCC mem- cover. The breakfast will be held on bers and your guests! This is a premier Monday, November 21st from 7:30 member & guest event. – 9:30am at The Landings on Dover Why should you attend? This is a Air Force Base. premier networking event for all in You can learn about the Dover attendance; and a one-stop-shop for Air Force Base’s activities and con- your holiday shopping! Not to mention struction projects that have been it’s FUN! completed over the past decade to What does the evening bring? The prepare the Base for long term via- Annual Holiday Gift Auction is com- bility as well as future projects being prised of a 2-part silent auction, live planned.