A Randomised, Placebo-Controlled, Double- Blind, Crossover Study of Losartan and Enalapril in Patients with Essential Hypertension
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effective Dose Range of Enalapril in Mild to Moderate Essential Hypertension
Br. J. clin. Pharmac. (1985), 19, 605-611 Effective dose range of enalapril in mild to moderate essential hypertension R. BERGSTRAND', H. HERLITZ2, SAGA JOHANSSON', G. BERGLUND2, A. VEDIN', C. WILHELMSSON', H. J. GOMEZ3, V. J. CIRILLO3 & J. A. BOLOGNESE4 'Department of Medicine, Ostra Hospital and 2Department of Medicine I, Sahlgrenska Hospital, Goteborg, Sweden and Department of 3Cardiovascular Clinical Research and 4Clinical Biostatistics, Merck Sharp & Dohme Research Laboratories, Rahway, New Jersey, USA 1 The dose-response relationship of enalapril was evaluated in a double-blind, balanced, two-period, incomplete-block study in 91 patients with mild to moderate essential hyper- tension. 2 Patients were randomly assigned to two of six treatments: placebo, 2.5, 5, 10, 20 and 40 mg/day of enalapril maleate. There were two 3-week treatment periods, each preceded by a 4-week, single-blind placebo washout. 3 Each dose of enalapril produced significant decreases in standing and supine systolic and diastolic blood pressure after 2 and 3 weeks of treatment. There were no significant changes on placebo. 4 There was a significant linear dose response relationship for both mean blood pressure and mean change from baseline in blood pressure (P < 0.01 for systolic and mean arterial pressure, and P < 0.05 for diastolic pressure). 5 Enalapril was associated with an increasing dose-response relationship across the 2.5- 40 mg/day range. The 2.5 mg/dose is effective in some patients; however, doses ¢ 10 mg/ day may be necessary to achieve satisfactory blood pressure control. Keywords enalapril angiotensin converting enzyme inhibitor dose-response relationship Introduction In recent years much interest has been focused with renal impairment treated with high doses of on angiotensin converting enzyme (ACE) in- captopril. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -
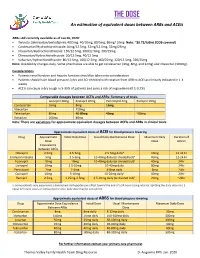
THE DOSE an Estimation of Equivalent Doses Between Arbs and Aceis
THE DOSE An estimation of equivalent doses between ARBs and ACEIs ARBs still currently available as of Jan 26, 2020: Twynsta (telmisartan/amlodipine): 40/5mg. 40/10mg, 80/5mg, 80mg/ 10mg Note: ~$0.73/tablet (ODB covered) Candesartan/Hydrochlorothiazide:16mg/12.5mg, 32mg/12.5mg, 32mg/25mg Irbesartan/Hydrochlorothiazide: 150/12.5mg, 300/12.5mg, 300/25mg Olmesartan/Hydrochlorothiaizde: 20/12.5mg, 40/12.5mg Valsartan/Hydrochlorothiazide: 80/12.5mg, 160/12.5mg, 160/25mg, 320/12.5mg, 320/25mg Note: Availability changes daily. Some pharmacies are able to get candesartan (4mg, 8mg, and 32mg) and irbesartan (300mg). Considerations Patients renal function and hepatic function should be taken into consideration Patients should have blood pressure, lytes and SCr checked with rotation from ARB to ACEI as clinically indicated in 1-4 weeks ACEIs can cause a dry cough in 5-35% of patients and carry a risk of angioedema (0.1-0.2%) Comparable dosages between ACEIs and ARBs- Summary of trials Lisinopril 20mg Enalapril 20mg Perindopril 4mg Ramipril 10mg Candesartan 16mg 8mg 16mg Irbesartan 150mg Telmisartan 80mg 40-80mg 40mg ~80mg Valsartan 160mg 80mg Note: There are variations for approximate equivalent dosages between ACEIs and ARBs in clinical trials. Approximate equivalent doses of ACEI for blood pressure lowering Drug Approximate Initial Daily Dose Usual Daily Maintenance Dose Maximum Daily Duration of Dose Dose Action Equivalence Between ACEIs Cilazapril 2.5mg 2.5-5mg 2.5-5mg dailya 10mg 12-24 hr Enalapril maleate 5mg 2.5-5mg 10-40mg daily (or divided bid)a 40mg 12-24 hr Fosinopril 10mg 10mg 10-40mg daily (or divided bid)a 40mg 24hr Lisinopril 10mg 2.5-10mg 10-40mg daily 80mg 24hr Perindopril 2mg 2-4mg 4-8mg daily 8mg 24hr Quinapril 10mg 5-10mg 10-20mg dailya 40mg 24hr Ramipril 2.5mg 1.25mg-2.5mg 2.5-10mg daily (or divided bid)a 20mg ~24hr a: Some patients may experience a diminished antihypertensive effect toward the end of a 24-hour dosing interval. -

Angiotensin-Converting Enzyme (ACE) Inhibitors
Angiotensin-Converting Enzyme (ACE) Inhibitors Summary Blood pressure reduction is similar for the ACE inhibitors class, with no clinically meaningful differences between agents. Side effects are infrequent with ACE inhibitors, and are usually mild in severity; the most commonly occurring include cough and hypotension. Captopril and lisinopril do not require hepatic conversion to active metabolites and may be preferred in patients with severe hepatic impairment. Captopril differs from other oral ACE inhibitors in its rapid onset and shorter duration of action, which requires it to be given 2-3 times per day; enalaprilat, an injectable ACE inhibitor also has a rapid onset and shorter duration of action. Pharmacology Angiotensin Converting Enzyme Inhibitors (ACE inhibitors) block the conversion of angiotensin I to angiotensin II through competitive inhibition of the angiotensin converting enzyme. Angiotensin is formed via the renin-angiotensin-aldosterone system (RAAS), an enzymatic cascade that leads to the proteolytic cleavage of angiotensin I by ACEs to angiotensin II. RAAS impacts cardiovascular, renal and adrenal functions via the regulation of systemic blood pressure and electrolyte and fluid balance. Reduction in plasma levels of angiotensin II, a potent vasoconstrictor and negative feedback mediator for renin activity, by ACE inhibitors leads to increased plasma renin activity and decreased blood pressure, vasopressin secretion, sympathetic activation and cell growth. Decreases in plasma angiotensin II levels also results in a reduction in aldosterone secretion, with a subsequent decrease in sodium and water retention.[51035][51036][50907][51037][24005] ACE is found in both the plasma and tissue, but the concentration appears to be greater in tissue (primarily vascular endothelial cells, but also present in other organs including the heart). -

Drugs for Primary Prevention of Atherosclerotic Cardiovascular Disease: an Overview of Systematic Reviews
Supplementary Online Content Karmali KN, Lloyd-Jones DM, Berendsen MA, et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. Published online April 27, 2016. doi:10.1001/jamacardio.2016.0218. eAppendix 1. Search Documentation Details eAppendix 2. Background, Methods, and Results of Systematic Review of Combination Drug Therapy to Evaluate for Potential Interaction of Effects eAppendix 3. PRISMA Flow Charts for Each Drug Class and Detailed Systematic Review Characteristics and Summary of Included Systematic Reviews and Meta-analyses eAppendix 4. List of Excluded Studies and Reasons for Exclusion This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. 1 Downloaded From: https://jamanetwork.com/ on 09/28/2021 eAppendix 1. Search Documentation Details. Database Organizing body Purpose Pros Cons Cochrane Cochrane Library in Database of all available -Curated by the Cochrane -Content is limited to Database of the United Kingdom systematic reviews and Collaboration reviews completed Systematic (UK) protocols published by by the Cochrane Reviews the Cochrane -Only systematic reviews Collaboration Collaboration and systematic review protocols Database of National Health Collection of structured -Curated by Centre for -Only provides Abstracts of Services (NHS) abstracts and Reviews and Dissemination structured abstracts Reviews of Centre for Reviews bibliographic -

Is Enalapril and Losartan Combination Irrational?Irrational?
Correspondence Is enalapril and losartan combination irrational?irrational? I read with great interest the editorial by C.S. Gautam and of exogenous angiotensin I pressor effects.[4] Therefore, the S. Aditya, which appeared in the Indian Journal of enalapril-losartan combinations are more potent at Pharmacology in June 2006 (vol, 38(3):167-70). A very achieving these goals than any of their constituents important topic was addressed in the editorial, and I individually. compliment the authors on this. On the other hand, I felt � Similarly synergistic efficacy of enalapril and losartan in confused when I found Enalapril + Losartan in the list of combination on exercise performance and oxygen irrational fixed dose combinations. I agree with the authors consumption at peak exercise in congestive heart failure that combining the two drugs affecting the same pathway is has been sugested.[5] irrational as it does not add to its efficacy, but I am not sure � The combination of an angiotensin-converting enzyme whether this combination should be categorised as irrational inhibitor and an angiotensin II receptor antagonist (AT1 or as rational. The results of ongoing research may answer receptor antagonist) in patients can significantly enhance this question in future. reduction in left ventricular hypertrophy. This can provide Apparently this combination may appear irrational, but greater protection to the heart against the overload caused actually rationality does exist for combining these two drugs. by persistent hypertension. Furthermore, the combination � From a physiological point of view, the general mechanism of these drugs did not increase the incidence of adverse of action of both angiotensin-converting enzyme inhibitor effects. -

Switching Ace-Inhibitors
Switching Ace-inhibitors http://www.ksdl.kamsc.org.au/dtp/switching_ace_inhibitors.html Change to → Enalapril Quinapril Ramipril Change from ↓ (Once daily dosing) (Once daily dosing) (Once daily dosing) Captopril Captopril 12.5mg daily Enalapril 2.5mg1 Quinapril 2.5mg Ramipril 1.25mg Captopril 25mg daily Enalapril 5mg1 Quinapril 5mg Ramipril 1.25-2.5mg Captopril 50mg daily Enalapril 7.5mg1 Quinapril 10mg Ramipril 2.5-5mg Captopril 100mg daily Enalapril 20mg1 Quinapril 20mg Ramipril 5-10mg2 Captopril 150mg daily Enalapril 40mg Quinapril 40mg Ramipril 10mg Fosinopril Fosinopril 5mg daily Enalapril 5mg Quinapril 5mg Ramipril 1.25mg Fosinopril 10mg daily Enalapril 10mg Quinapril 10mg Ramipril 2.5mg Fosinopril 20mg daily Enalapril 20mg Quinapril 20mg Ramipril 5mg Fosinopril 40mg daily Enalapril 40mg Quinapril 40mg Ramipril 10mg Lisinopril Lisinopril 5mg daily Enalapril 5mg Quinapril 5mg Ramipril 1.25mg Lisinopril 10mg daily Enalapril 10mg Quinapril 10mg Ramipril 2.5mg Lisinopril 20mg daily Enalapril 20mg Quinapril 20mg Ramipril 5mg Lisinopril 40mg Enalapril 40mg Quinapril 40mg Ramipril 10mg Perindopril Perindopril 2mg daily Enalapril 5-10mg Quinapril 5-10mg Ramipril 2.5mg Perindopril 4mg daily Enalapril 10mg-20mg Quinapril 10mg-20mg Ramipril 5mg Perindopril 8mg daily Enalapril 20-40mg Quinapril 20-40mg Ramipril 10mg Trandolapril Trandolapril 0.5mg d Enalapril 5mg Quinapril 5mg Ramipril 1.25mg Trandolapril 1mg daily Enalapril 10mg Quinapril 10mg Ramipril 2.5mg Trandolapril 2mg daily Enalapril 20mg Quinapril 20mg Ramipril 5mg Trandolapril 4mg daily Enalapril 40mg Quinapril 40mg Ramipril 10mg There are few studies comparing equivalent doses of ACE-inhibitors, for specific indications. Therefore, the above recommendations are based on clinical experiences and are not specific for any indication. -

(12) Patent Application Publication (10) Pub. No.: US 2007/0293552 A1 Gorczynski (43) Pub
US 20070293552A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2007/0293552 A1 Gorczynski (43) Pub. Date: Dec. 20, 2007 (54) ANTIHYPERTENSIVE THERAPY METHOD Publication Classification (76) Inventor: Richard J. Gorczynski, Westminster, (51) Int. Cl. CO (US) A6II 3/42 (2006.01) (52) U.S. Cl. .............................................................. S14/378 Correspondence Address: (57) ABSTRACT HARNESS, DICKEY, & PIERCE, P.L.C Methods and therapeutic combinations are provided for 7700 BONHOMME, STE 400 lowering blood pressure in a Subject exhibiting resistance to ST. LOUIS, MO 63105 (US) a baseline antihypertensive therapy with one or more drugs, or a subject having diabetes and/or chronic kidney disease. A method of the invention comprises administering, in some (21) Appl. No.: 11/761,499 embodiments adjunctively with a modified baseline therapy, a compound of formula (I) as defined herein. A therapeutic (22) Filed: Jun. 12, 2007 combination of the invention comprises a compound of formula (I); at least one diuretic; and at least one antihy pertensive drug selected from ACE inhibitors, angiotensin II Related U.S. Application Data receptor blockers, beta-adrenergic receptor blockers and calcium channel blockers; wherein the at least one diuretic (60) Provisional application No. 60/813.966, filed on Jun. and/or the at least one antihypertensive drug are present at 15, 2006. substantially less than a full dose. US 2007/0293552 A1 Dec. 20, 2007 ANTHYPERTENSIVE THERAPY METHOD signaling pathways. While antagonism of the ETA receptor is known to reduce endothelin-mediated vasoconstriction, 0001. This application claims the benefit of U.S. provi antagonism of the endothelin-B (ET) receptor can block sional application Ser. -

Valoración De La Terapia Combinada De Enalapril Con Irbesartán Sobre La Función Renal En Pacientes Diabéticos Tipo 2
Revista Médica de la Universidad de Costa Rica. Volumen 1, número 1, artículo 7, septiembre 2007. http://www.revistamedica.ucr.ac. Sección Estudiantil Valoración de la terapia combinada de Enalapril con Irbesartán sobre la función renal en pacientes diabéticos tipo 2 Rodríguez Hernández, Andrea.*, Rosenkrantz Amón, Shunit.*, Jiménez Loría, Federico**, Chaverri Fernández, José Miguel*** *Estudiantes de Farmacia. Universidad de Costa Rica, **Farmacéutico. Subdirector de Farmacia Hospital México, ***Farmacéutico. Centro Nacional de Información de Medicamentos. INIFAR. Facultad de Farmacia. Universidad de Costa Rica. Resumen: El presente trabajo pretende adicionar evidencia que respalde el uso concomitante de enalapril e irbersartán en los pacientes diabéticos del Hospital México. Métodos: Se seleccionó una muestra de pacientes diabéticos atendidos en el servicio de nefrología del Hospital México durante el periodo 2004-2006, valorándose en ellos, la función renal y la correlación existente con respecto al tratamiento recibido como nefroprotección, ya sea IECA o ARA II asociado a IECA. Resultados: La proporción de pacientes que utilizaron el tratamiento combinado y logran mejorar su función renal es mucho mayor que la proporción de pacientes que alcanzan esta mejoría dentro del grupo control o con monoterapia. Conclusiones: Los datos indican que existe una posible ventaja al utilizar el tratamiento combinado IECA – ARA II vs. la monoterapia con IECA como agentes renoprotectores. Palabras claves: Neuropatía diabética, ARA II, IECAS, diabetes, renoprotección. Recibido: Junio 2007. Aceptado: Septiembre. Publicado: Septiembre 2007. _____________________________________________________________________ 64 Revista electrónica publicada por la Escuela de Medicina de la Universidad de Costa Rica, 2060 San José, Costa Rica. ® All rights reserved. Revista Médica de la Universidad de Costa Rica. -
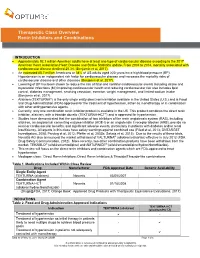
Therapeutic Class Overview Renin Inhibitors and Combinations
Therapeutic Class Overview Renin Inhibitors and Combinations INTRODUCTION Approximately 92.1 million American adults have at least one type of cardiovascular disease according to the 2017 American Heart Association Heart Disease and Stroke Statistics update. From 2004 to 2014, mortality associated with cardiovascular disease declined 25.3% (Benjamin et al, 2017). An estimated 85.7 million Americans or 34% of US adults aged ≥20 years have high blood pressure (BP). Hypertension is an independent risk factor for cardiovascular disease and increases the mortality risks of cardiovascular disease and other diseases (Benjamin et al, 2017). Lowering of BP has been shown to reduce the risk of fatal and nonfatal cardiovascular events including stroke and myocardial infarctions (MI) improving cardiovascular health and reducing cardiovascular risk also includes lipid control, diabetes management, smoking cessation, exercise, weight management, and limited sodium intake (Benjamin et al, 2017). Aliskiren (TEKTURNA®) is the only single entity direct renin inhibitor available in the United States (U.S.) and is Food and Drug Administration (FDA)-approved for the treatment of hypertension, either as monotherapy or in combination with other antihypertensive agents. Currently, only one combination renin inhibitor product is available in the US. This product combines the direct renin inhibitor, aliskiren, with a thiazide diuretic (TEKTURNA-HCT®) and is approved for hypertension. Studies have demonstrated that the combination of two inhibitors of the renin angiotensin system (RAS), including aliskiren, an angiotensin converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB), provide no renal or cardiovascular benefits, and significant adverse events, particularly in patients with diabetes and/or renal insufficiency. -

ACE2 As a Therapeutic Target for COVID-19; Its Role in Infectious Processes and Regulation by Modulators of the RAAS System
Journal of Clinical Medicine Review ACE2 as a Therapeutic Target for COVID-19; Its Role in Infectious Processes and Regulation by Modulators of the RAAS System Veronique Michaud 1,2, Malavika Deodhar 1, Meghan Arwood 1, Sweilem B Al Rihani 1, Pamela Dow 1 and Jacques Turgeon 1,2,* 1 Tabula Rasa HealthCare Precision Pharmacotherapy Research & Development Institute, Orlando, FL 32827, USA; [email protected] (V.M.); [email protected] (M.D.); [email protected] (M.A.); [email protected] (S.B.A.R.); [email protected] (P.D.) 2 Faculty of Pharmacy, Université de Montréal, Montreal, QC H3C 3J7, Canada * Correspondence: [email protected]; Tel.: +856-938-8793 Received: 11 June 2020; Accepted: 2 July 2020; Published: 3 July 2020 Abstract: Angiotensin converting enzyme 2 (ACE2) is the recognized host cell receptor responsible for mediating infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). ACE2 bound to tissue facilitates infectivity of SARS-CoV-2; thus, one could argue that decreasing ACE2 tissue expression would be beneficial. However, ACE2 catalytic activity towards angiotensin I (Ang I) and II (Ang II) mitigates deleterious effects associated with activation of the renin-angiotensin-aldosterone system (RAAS) on several organs, including a pro-inflammatory status. At the tissue level, SARS-CoV-2 (a) binds to ACE2, leading to its internalization, and (b) favors ACE2 cleavage to form soluble ACE2: these actions result in decreased ACE2 tissue levels. Preserving tissue ACE2 activity while preventing ACE2 shredding is expected to circumvent unrestrained inflammatory response. Concerns have been raised around RAAS modulators and their effects on ACE2 expression or catalytic activity. -

Comparative Study of an Angiotensin-II Analog and a Converting Enzyme Inhibitor
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 17 (1980), pp. 647-653 Comparative study of an angiotensin-JI analog and a converting enzyme inhibitor ROBERT H. FAGARD, ANTOON K. AMERY, PAUL J. LIJNEN, and TONY M. REYBROUCK Hypertension and Cardiovascular Rehabilitation Unit, Department of Pathophysiology, University of Leuven, Leuven, Belgium Comparative study of an angiotensin-Il analog and a converting The angiotensin-Il (All) analog sar1 ala8-angioten- enzyme inhibitor. The effects of an angiotensin-Il analog (sarala- sin II, a specific antagonist of the vascular effects of sin, iv.) and of a converting enzyme inhibitor (captopril, oral) were compared in 12 sodium-depleted patients with hyper- All [1], has been studied intensively in patients with tension. The decrease of the mean intraarterial pressure (MAP) hypertension, and is a powerful hypotensive agent with captopril (—21.5 [sEM] 4.3mm Hg) was more pronounced in sodium-volume-depleted hypertensive patients (P <0.001)than the change of MAP during saralasin (—10.5 4.0mm Hg). The pretreatment arterial plasma renin activity (log except in patients with low plasma renin values. Its PRA) was closely related to the change of MAP during saralasin effect to lower blood pressure is indeed closely re- (r =—0.94;P <0.001)and also to the captopril-induced change lated to the plasma levels of renin or All [2-5], and of MAP(r —0.82; P <0.001); similar results were obtained for the log plasma angiotensin (PA) I and II levels.