Predicting Initial Aftercare Appointment Adherence and Rehospitalization For
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Song Lyrics of the 1950S
Song Lyrics of the 1950s 1951 C’mon a my house by Rosemary Clooney Because of you by Tony Bennett Come on-a my house my house, I’m gonna give Because of you you candy Because of you, Come on-a my house, my house, I’m gonna give a There's a song in my heart. you Apple a plum and apricot-a too eh Because of you, Come on-a my house, my house a come on My romance had its start. Come on-a my house, my house a come on Come on-a my house, my house I’m gonna give a Because of you, you The sun will shine. Figs and dates and grapes and cakes eh The moon and stars will say you're Come on-a my house, my house a come on mine, Come on-a my house, my house a come on Come on-a my house, my house, I’m gonna give Forever and never to part. you candy Come on-a my house, my house, I’m gonna give I only live for your love and your kiss. you everything It's paradise to be near you like this. Because of you, (instrumental interlude) My life is now worthwhile, And I can smile, Come on-a my house my house, I’m gonna give you Christmas tree Because of you. Come on-a my house, my house, I’m gonna give you Because of you, Marriage ring and a pomegranate too ah There's a song in my heart. -
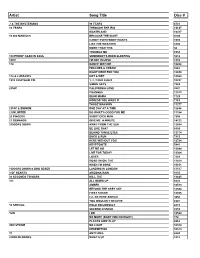
Copy UPDATED KAREOKE 2013
Artist Song Title Disc # ? & THE MYSTERIANS 96 TEARS 6781 10 YEARS THROUGH THE IRIS 13637 WASTELAND 13417 10,000 MANIACS BECAUSE THE NIGHT 9703 CANDY EVERYBODY WANTS 1693 LIKE THE WEATHER 6903 MORE THAN THIS 50 TROUBLE ME 6958 100 PROOF AGED IN SOUL SOMEBODY'S BEEN SLEEPING 5612 10CC I'M NOT IN LOVE 1910 112 DANCE WITH ME 10268 PEACHES & CREAM 9282 RIGHT HERE FOR YOU 12650 112 & LUDACRIS HOT & WET 12569 1910 FRUITGUM CO. 1, 2, 3 RED LIGHT 10237 SIMON SAYS 7083 2 PAC CALIFORNIA LOVE 3847 CHANGES 11513 DEAR MAMA 1729 HOW DO YOU WANT IT 7163 THUGZ MANSION 11277 2 PAC & EMINEM ONE DAY AT A TIME 12686 2 UNLIMITED DO WHAT'S GOOD FOR ME 11184 20 FINGERS SHORT DICK MAN 7505 21 DEMANDS GIVE ME A MINUTE 14122 3 DOORS DOWN AWAY FROM THE SUN 12664 BE LIKE THAT 8899 BEHIND THOSE EYES 13174 DUCK & RUN 7913 HERE WITHOUT YOU 12784 KRYPTONITE 5441 LET ME GO 13044 LIVE FOR TODAY 13364 LOSER 7609 ROAD I'M ON, THE 11419 WHEN I'M GONE 10651 3 DOORS DOWN & BOB SEGER LANDING IN LONDON 13517 3 OF HEARTS ARIZONA RAIN 9135 30 SECONDS TO MARS KILL, THE 13625 311 ALL MIXED UP 6641 AMBER 10513 BEYOND THE GREY SKY 12594 FIRST STRAW 12855 I'LL BE HERE AWHILE 9456 YOU WOULDN'T BELIEVE 8907 38 SPECIAL HOLD ON LOOSELY 2815 SECOND CHANCE 8559 3LW I DO 10524 NO MORE (BABY I'MA DO RIGHT) 178 PLAYAS GON' PLAY 8862 3RD STRIKE NO LIGHT 10310 REDEMPTION 10573 3T ANYTHING 6643 4 NON BLONDES WHAT'S UP 1412 4 P.M. -

Daughter Album If You Leave M4a Download Download Verschillende Artiesten - British Invasion (2017) Album
daughter album if you leave m4a download Download Verschillende artiesten - British Invasion (2017) Album. 1. It's My Life 2. From the Underworld 3. Bring a Little Lovin' 4. Do Wah Diddy Diddy 5. The Walls Fell Down 6. Summer Nights 7. Tuesday Afternoon 8. A World Without Love 9. Downtown 10. This Strange Effect 11. Homburg 12. Eloise 13. Tin Soldier 14. Somebody Help Me 15. I Can't Control Myself 16. Turquoise 17. For Your Love 18. It's Five O'Clock 19. Mrs. Brown You've Got a Lovely Daughter 20. Rain On the Roof 21. Mama 22. Can I Get There By Candlelight 23. You Were On My Mind 24. Mellow Yellow 25. Wishin' and Hopin' 26. Albatross 27. Seasons In the Sun 28. My Mind's Eye 29. Do You Want To Know a Secret? 30. Pretty Flamingo 31. Come and Stay With Me 32. Reflections of My Life 33. Question 34. The Legend of Xanadu 35. Bend It 36. Fire Brigade 37. Callow La Vita 38. Goodbye My Love 39. I'm Alive 40. Keep On Running 41. The Hippy Hippy Shake 42. It's Not Unusual 43. Love Is All Around 44. Don't Let Me Be Misunderstood 45. The Days of Pearly Spencer 46. The Pied Piper 47. With a Girl Like You 48. Zabadak! 49. I Only Want To Be With You 50. Here It Comes Again 51. Don't Let the Sun Catch You Crying 52. Have I the Right 53. Darling Be Home Soon 54. Only One Woman 55. -
Devotions for Lent 2021 Heather Roth Johnson, Editor
Devotions for Lent 2021 Heather Roth Johnson, Editor February 17 Sorry! “And forgive us our sins, as we forgive those who sin against us.” (Matthew 6:12) No matter what age, I always have loved games. Online gaming, cards, and board games - I will play anything. But the best game is Sorry! That feeling of squashing someone else’s pawn, sending them home, and claiming their spot while saying in a snotty voice, “SORRY!” is exhilarating. As a kid, I would follow the “sorry” with “not!” These days “sorry not sorry” is a common phrase used to express a lack of regret or repentance. Sometimes people say it to be funny, but sometimes when people are forced to apologize, you may hear “sorry...not sorry.” Today marks the first day in lent. We ash our foreheads, hear the call to repentance, and relearn about the forgiveness of sins. Isn’t that what we get in Christ Jesus? True forgiveness? No “sorry not sorry” from him, but instead everlasting life, love, and forgiveness. Who do you need to forgive today? Jesus, in the game of life, help us to love and say we are “sorry” to others. Amen. February 18 Crazy 8’s Jesus said, “Don’t store up treasures on earth! Moths and rust can destroy them, and thieves can break in and steal them. Instead, store up your treasures in heaven….Your heart will always be where your treasure is.” (Matthew 6:19-21) It’s been said, “the one who dies with the most toys wins.” In other words, life is all about accumulating stuff. -

9780718077396.Pdf
Pocket Payers for Moms 40 Simple Prayers that Bring Peace and Rest By Max Lucado, Andrea Lucado Thomas Nelson Copyright © 2015 Max Lucado All rights reserved. ISBN: 978-0-7180-7739-6 CHAPTER 1 Prayers for Time and Peace 1 Now may the Lord of peace Himself give you peace always in every way. The Lord be with you all. 2 Thessalonians 3:16 Father, you are wise and all-knowing. You allow all things to happen in your perfect timing. Please give me peace in the midst of a busy season with my family. I feel pulled in so many directions by my kids' needs, my husband's requests, and my life. Surround my family in this time. May your peace bring us all peace, and may you create a calm environment in our home. Thank you that you have gone before us in this hectic time and for bringing order to the chaos when we need it most. Thank you for giving me time to hug my kids and show them what a precious gift they are to me. In Jesus' name, amen. 2 The Lord will give strength to His people; the Lord will bless His people with peace. Psalm 29:11 God, you are my strength during the hard times. Your grace is sufficient for me, and your power is made perfect in my weakness. Today I feel spread thin and overcommitted. I don't have the strength in me to do what needs to be done. Give me the energy I need just for today. -
Messages to Families from the Class of 2019
‘Dear Mom & Dad’ Messages to families from the Class of 2019 Dear Mom and Nana, Another four years have come and gone, and it is safe to say that I would not have made it through without you two. Thank you for always loving and supporting me. I would not be where I am today if it weren’t for you. Love always, Ryannon Dear Mama & Dad, Thank you for everything. From all the late night calls in boarding school to the small gifts and support in college. You helped me become the person I am today and I am so lucky to be your daughter. I love you both very much and I can't wait to show you how far I'm going to go! Love, Fiona Dear Mom and Dad, Thank you for everything! Thank you for always getting me where I needed to be and for pushing me to always do my best! I wouldn't have been able to do this without all of your help and support. I appreciate every little thing you have done for me; from the cute care packages that never failed to put a smile on my face, to coming to my games to cheer me on, to helping to keep me relaxed when times got tough. I can't wait to see where life takes me from here! Thank you! Love you lots, Harleigh Dear Mom and Dad, I feel so honored and blessed to have you as my parents and want to express my gratitude for your care and support over the years. -

PDF Download When God Writes Your Life Story: Experience the Ultimate Adventure Ebook
WHEN GOD WRITES YOUR LIFE STORY: EXPERIENCE THE ULTIMATE ADVENTURE PDF, EPUB, EBOOK Eric Ludy,Leslie Ludy | 240 pages | 10 Sep 2004 | Multnomah Press | 9781590523391 | English | Sisters, United States When God Writes Your Life Story: Experience the Ultimate Adventure PDF Book In their most popular book, bestselling authors Eric and Leslie Ludy challenge singles to take a fresh approach to relationships in a culture where love has been replaced by cheap sensual passion. Tommy Barnett. Rather than building a love story the way the world does with a few Christian morals tacked on for good measure , this book introduces listeners to a far superior way of building a love story Anonymous User In their new book, bestselling authors Eric and Leslie Ludy reveal that the life God has called us. I love it because it got me excited about my faith. Nevertheless, seekers may benefit from the study guide, which recommends reading Christian biographies, setting goals in every area of life and developing good habits. Inspired by Your Browsing History. Nevertheless, seekers may benefit from the study guide, which recommends reading Christian biographies, setting goals in every area of life and developing good habits. They then urge readers to leave all that behind in favor of extreme faith, the ultimate adventure, which requires losing faith in oneself and trusting God completely. The Worn Out Woman. Will it make a difference? From the authors of When God Writes Your Love Story comes a refreshing challenge for young believers: Don't 'settle' for a humdrum, outwardly religious life. And while many of the embarrassingly outmoded phrases and illustrations have been altered to reflect our modern times, a few Eric-isms were left in just so you can enjoy a good laugh at his expense. -

New Skye Song List
New Skye Song List Americana Country Acony Bell Gillian Welch Act Naturally Buck Owens Across The Great Divide Kate Wolf Already Gone Eagles Blue and Lonesome Bill Monroe Amie Pure Prairie League Caleb Meyer Gillian Welch Boot Scooting Boogie Brooks & Dunn Crying Madison Violet Cold Day in July Suzy Bogguss Down by the River Neil Young Country Roads John Denver Further in the Hole Claire Lynch Crazy Patsy Cline Give Yourself to Love Kate Wolf Driving My Life Away Eddie Rabbit Harvest Moon Neil Young Family Tradition Hank Williams II High Sierra Trio Folsom Prison Blues Johnny Cash I Ain't Broke David Grisman Hey Good Lookin' Hank Williams I'll Fly Away Gillian Welch Hurt Me Bad Patty Loveless I’ll Be Waiting Just for You Junior Sisk Jackson Johnny Cash Man of Constant Sorrow Dan Tyminski Jambalaya Hank Williams Oh, Atlanta Allison Krauss Just Good Ol' Boys Moe & Joe Oklahoma Hills Hank Thompson Just One More George Jones Ophelia The Band Louisiana Saturday Night Mel McDaniel Orphan Girl Gillian Welch Pancho & Lefty Emmylou Harris Rag Mama Rag The Band Peaceful Easy Feeling Eagles Stealin' Arlo Guthrie San Antonio Rose Patsy Cline Tecumseh Valley Nanci Griffith Seminole Wind John Anderson This Land Is Your Land Woody Guthrie Silver Wings Merle Haggard Twilight Linda Williams Six Pack to Go Leon Russell Wagon Wheel Old Crow Med/Show Streets of Bakersfield Dwight Yoakam Wichita Gillian Welch Take It Easy Eagles Willin' Little Feat Tequila Sunrise Eagles You Ain't Going Nowhere Bob Dylan The Bottle Let Me Down Merle Haggard You Are My Sunshine -

YARDBIRDS, 10Cc, & Graham Gouldman
YARDBIRDS, 10CC, & GRAHAM GOULDMAN by Alan L. Chrisman The Yardbirds were a legendary British Blues-rock band in the 60’s. Especially because three well-known guitarists came out of one band at one point or another: Eric Clapton, Jeff Beck and Jimmy Page. They started out as a blues band, replacing The Stones at the Crawdaddy Club in Richmond, England. But Clapton left the band in ’65 because he didn’t like their commercial direction and he joined John Mayall’s Bluesbreakers, to be replaced by Page and later, Jeff Beck, who was known for first experimenting with guitar feedback. The Yardirds also make an appearance in Antonioni’s film, Blowup in 1966. Their first big commercial hits though, “ For Your Love” and “Heart Full of Soul’”were written by songwriter, Graham Gouldman. The still-teenage Gouldman, very influenced by The Beatles, had original planned to give them his song, “For Your Love” , but that night the Yardbirds were opening for The Beatles and he gave it to Jimmy Page instead and it became The Yardbirds’ first big hit. Gouldman also wrote several hits for The Hollies (“ Bus Stop”, “Look Through Any Window”), Herman’s Hermits ( “No Milk Today”) and many others. He briefly replaced, Wayne Fontana of The Mindbenders after their hit, “The Game of Love”, where he met his future 10cc bandmate, Eric Stewart. Kevin Godley and Lol Creme would then join Stewart and Gouldman under the name, Hotlegs and have an international single with “Neanderthal Man” in 1970. The four would then form the art-rock band 10cc. -
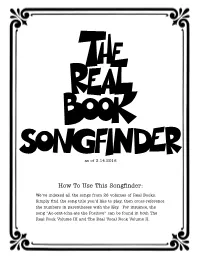
How to Use This Songfinder
as of 3.14.2016 How To Use This Songfinder: We’ve indexed all the songs from 26 volumes of Real Books. Simply find the song title you’d like to play, then cross-reference the numbers in parentheses with the Key. For instance, the song “Ac-cent-tchu-ate the Positive” can be found in both The Real Book Volume III and The Real Vocal Book Volume II. KEY Unless otherwise marked, books are for C instruments. For more product details, please visit www.halleonard.com/realbook. 01. The Real Book – Volume I 10. The Charlie Parker Real Book (The Bird Book)/00240358 C Instruments/00240221 11. The Duke Ellington Real Book/00240235 B Instruments/00240224 Eb Instruments/00240225 12. The Bud Powell Real Book/00240331 BCb Instruments/00240226 13. The Real Christmas Book – 2nd Edition Mini C Instruments/00240292 C Instruments/00240306 Mini B Instruments/00240339 B Instruments/00240345 CD-ROMb C Instruments/00451087 Eb Instruments/00240346 C Instruments with Play-Along Tracks BCb Instruments/00240347 Flash Drive/00110604 14. The Real Rock Book/00240313 02. The Real Book – Volume II 15. The Real Rock Book – Volume II/00240323 C Instruments/00240222 B Instruments/00240227 16. The Real Tab Book – Volume I/00240359 Eb Instruments/00240228 17. The Real Bluegrass Book/00310910 BCb Instruments/00240229 18. The Real Dixieland Book/00240355 Mini C Instruments/00240293 CD-ROM C Instruments/00451088 19. The Real Latin Book/00240348 03. The Real Book – Volume III 20. The Real Worship Book/00240317 C Instruments/00240233 21. The Real Blues Book/00240264 B Instruments/00240284 22. -

2016 Senior Class Litany of Thanks
2016 SENIOR CLASS LITANY OF THANKS #1= Mauricio Huertas, #2 = Maria Catherino Music = Victor Xiong Members of the graduating class would like to give thanks for the people and life experiences which brought us to this day. We’ve strung these statements together into one litany of thanks. It goes like this: #1 Thanks to everyone in the Chemistry Department who taught me how to exit the building safely in case of fire [pause for possible laughter]. Also a special thanks to Professor Tepper who taught me to question the existing body of knowledge at the very first day, because knowledge is not static but rather dynamic. Thank you to the Education department, who kept me going toward what I'd wanted since I was six years old. To the Thetas and the Gammas, you taught me lessons that school never could. And to my family, for supporting me with true love, or tough love, no matter what. __ #2 For the women who gave me a soft spot to land when I fell, courage to get back up again, and above all, the chance to pass it on to someone else who needed it. I’ve never been prouder to call myself an Arrow. Thanks to my best friend for being my buddy through four years of conniptions and "doing the most"; thanks to Ink Pond for moonlit nights of calm and the local fox family for reminding me that "all good things are wild and free". Also thanks to the Boundary Waters English lit. class for not ruining Thoreau for me, despite it's best effort. -
Every Memory Lingers with Me Yet
NEW ORLEANS NOSTALGIA Remembering New Orleans History, Culture and Traditions By Ned Hémard Every Memory Lingers With Me Yet I got it bad like I told you before, I’m so in love with you, Don’t leave me no more. Without ever having taken a puff, one has to be deeply moved by the haunting and romantic lyrics of Lipstick Traces (On a Cigarette) by Benny Spellman. In the canon of New Orleans’ all-time great songs, this one has the distinction of being part of one of those 45 singles that has two dynamite cuts (both sides A and B). The flip side classic is Benny’s uptempo Fortune Teller, both songs written (under the pseudonym Naomi Neville) by Allen Toussaint: Went to a fortune teller. Had my fortune read. I didn't know what to tell her. I had a dizzy feeling in my head. Then she took a look at my palm. She said "Sonny, you feel kinda warm." She looked into her crystal ball And said "You're in love." I said, “how could that be so?” I’m not tight with none o’ the girls I know. She said when the next one arrives. You’ll be looking in her eyes … Just as the unsuspecting visitor to Madame Ruth (you know that gypsy with the gold-capped tooth) in Leiber and Stoller’s 1959 hit Love Potion No. 9 falls in love, so does Toussaint’s victim in Fortune Teller. He ends up a “happy fella” who’s “married to the fortune teller”. In conclusion, Benny belts out, “We’re happy as we can be, and now I get my fortune told for free!” Lipstick Traces/Fortune Teller was on the Minit Label, number 644, entering the charts in May of 1962, but (after about six weeks) never going higher than number 80 on Billboard’s Hot 100 (yet 28 on the R&B charts).