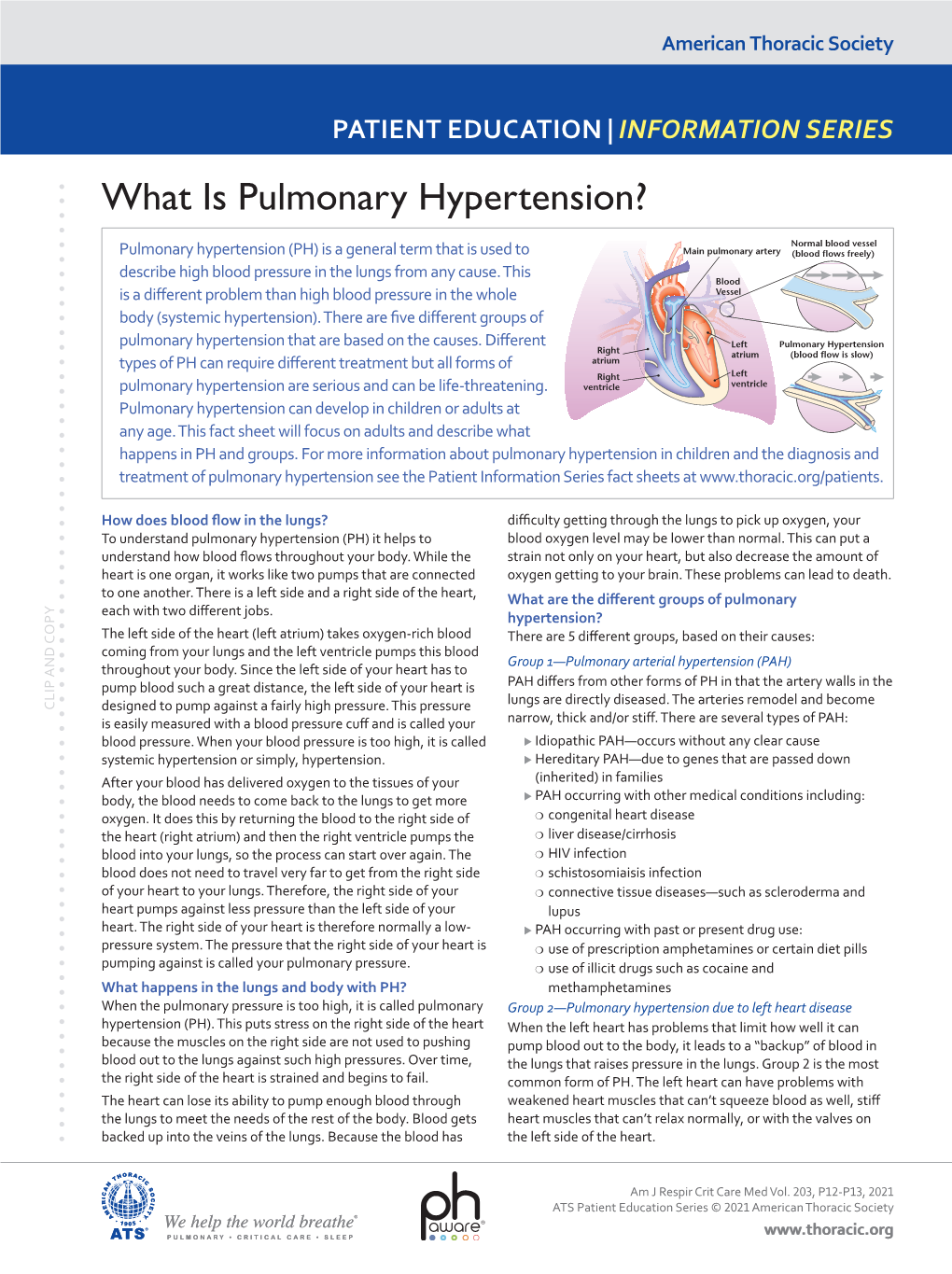
What Is Pulmonary Hypertension?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prep for Practical II
Images for Practical II BSC 2086L "Endocrine" A A B C A. Hypothalamus B. Pineal Gland (Body) C. Pituitary Gland "Endocrine" 1.Thyroid 2.Adrenal Gland 3.Pancreas "The Pancreas" "The Adrenal Glands" "The Ovary" "The Testes" Erythrocyte Neutrophil Eosinophil Basophil Lymphocyte Monocyte Platelet Figure 29-3 Photomicrograph of a human blood smear stained with Wright’s stain (765). Eosinophil Lymphocyte Monocyte Platelets Neutrophils Erythrocytes "Blood Typing" "Heart Coronal" 1.Right Atrium 3 4 2.Superior Vena Cava 5 2 3.Aortic Arch 6 4.Pulmonary Trunk 1 5.Left Atrium 12 9 6.Bicuspid Valve 10 7.Interventricular Septum 11 8.Apex of The Heart 9. Chordae tendineae 10.Papillary Muscle 7 11.Tricuspid Valve 12. Fossa Ovalis "Heart Coronal Section" Coronal Section of the Heart to show valves 1. Bicuspid 2. Pulmonary Semilunar 3. Tricuspid 4. Aortic Semilunar 5. Left Ventricle 6. Right Ventricle "Heart Coronal" 1.Pulmonary trunk 2.Right Atrium 3.Tricuspid Valve 4.Pulmonary Semilunar Valve 5.Myocardium 6.Interventricular Septum 7.Trabeculae Carneae 8.Papillary Muscle 9.Chordae Tendineae 10.Bicuspid Valve "Heart Anterior" 1. Brachiocephalic Artery 2. Left Common Carotid Artery 3. Ligamentum Arteriosum 4. Left Coronary Artery 5. Circumflex Artery 6. Great Cardiac Vein 7. Myocardium 8. Apex of The Heart 9. Pericardium (Visceral) 10. Right Coronary Artery 11. Auricle of Right Atrium 12. Pulmonary Trunk 13. Superior Vena Cava 14. Aortic Arch 15. Brachiocephalic vein "Heart Posterolateral" 1. Left Brachiocephalic vein 2. Right Brachiocephalic vein 3. Brachiocephalic Artery 4. Left Common Carotid Artery 5. Left Subclavian Artery 6. Aortic Arch 7. -

In the Pulmonary Arteries, Capillaries, and Veins
Longitudinal Distribution of Vascular Resistance in the Pulmonary Arteries, Capillaries, and Veins JEROME S. BRODY, EDWARD J. STEMMLER, and ARTHu B. DuBois From the Department of Physiology, Division of Graduate Medicine, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 A B S T R A C T A new method has been described monary artery pressure averaged 20.4 cm H2O, for measuring the pressure and resistance to blood and pulmonary vein pressure averaged 9.2 cm flow in the pulmonary arteries, capillaries, and H2O. These techniques also provide a way of ana- veins. Studies were performed in dog isolated lyzing arterial, capillary, and venous responses to lung lobes perfused at constant flow with blood various pharmacologic and physiologic stimuli. from a donor dog. Pulmonary artery and vein volume and total lobar blood volume were mea- INTRODUCTION sured by the ether plethysmograph and dye- dilution techniques. The longitudinal distribution The arterioles are the major resistance vessels in of vascular resistance was determined by analyzing the systemic vascular bed (1, 2), but it is uncer- the decrease in perfusion pressure caused by a tain whether the greatest resistance to blood flow bolus of low viscosity liquid introduced into the in the lungs is in the arteries, capillaries, or veins vascular inflow of the lobe. (1, 3, 4). The pulmonary arteries were responsible for Piiper (5), in 1958, reasoned from Poiseuille's 46% of total lobar vascular resistance, whereas law that, during constant perfusion, injection into the pulmonary capillaries and veins accounted for the bloodstream of a bolus of fluid with viscosity 34 and 20% of total lobar vascular resistance different from that of blood would cause a per- respectively. -

Hypertension: Putting the Pressure on the Silent Killer
HYPERTENSION: PUTTING THE PRESSURE ON THE SILENT KILLER MAY 2016 TABLEHypertension: putting OF the CONTENTS pressure on the silent killer Table of contents UNDERSTANDING HYPERTENSION AND THE LINK TO CARDIOVASCULAR DISEASE 2 Understanding hypertension and the link to cardiovascular disease THEThe social SOCIAL and economic AND impact ECONOMIC of hypertension IMPACT OF HYPERTENSION 3 Diagnosing and treating hypertension – what is out there? DIAGNOSINGChallenges to tackling hypertension AND TREATING HYPERTENSION – WHAT IS OUT THERE? 6 Opportunities and focus areas for policymakers CHALLENGES TO TACKLING HYPERTENSION 9 OPPORTUNITIES AND FOCUS AREAS FOR POLICYMAKERS 15 HYPERTENSION: PUTTING THE PRESSURE ON THE SILENT KILLER UNDERSTANDING HYPERTENSION AND THE LINK TO CARDIOVASCULAR DISEASE Cardiovascular disease (CVD), or heart disease, is the number one cause of death in the world. 80% of deaths due to CVD occur in countries and poor communities where health systems are weak, and CVD accounts for nearly half of the estimated US$500 billion annual lost economic output associated with noncommunicable diseases (NCDs) in low-income and middle-income countries. In 2012, CVD killed 17.5 million people – the equivalent of every 3 in 10 deaths.1 Of these 17 million deaths a year, over half – 9.4 million - are caused by complications in hypertension, also commonly referred to as raised or high blood pressure2. Hypertension is a risk factor for coronary heart disease and the single most important risk factor for stroke - it is responsible for at least 45% of deaths due to heart disease, and at least 51% of deaths due to stroke. High blood pressure is defined as a systolic blood pressure at or above 140 mmHg and/or a diastolic blood pressure at or above 90 mmHg. -

Hypertension and Coronary Heart Disease
Journal of Human Hypertension (2002) 16 (Suppl 1), S61–S63 2002 Nature Publishing Group All rights reserved 0950-9240/02 $25.00 www.nature.com/jhh Hypertension and coronary heart disease E Escobar University of Chile, Santiago, Chile The association of hypertension and coronary heart atherosclerosis, damage of arterial territories other than disease is a frequent one. There are several patho- the coronary one, and of the extension and severity of physiologic mechanisms which link both diseases. coronary artery involvement. It is important to empha- Hypertension induces endothelial dysfunction, exacer- sise that complications and mortality of patients suffer- bates the atherosclerotic process and it contributes to ing a myocardial infarction are greater in hypertensive make the atherosclerotic plaque more unstable. Left patients. Treatment should be aimed to achieve optimal ventricular hypertrophy, which is the usual complication values of blood pressure, and all the strategies to treat of hypertension, promotes a decrease of ‘coronary coronary heart disease should be considered on an indi- reserve’ and increases myocardial oxygen demand, vidual basis. both mechanisms contributing to myocardial ischaemia. Journal of Human Hypertension (2002) 16 (Suppl 1), S61– From a clinical point of view hypertensive patients S63. DOI: 10.1038/sj/jhh/1001345 should have a complete evaluation of risk factors for Keywords: hypertension; hypertrophy; coronary heart disease There is a strong and frequent association between arterial hypertension.8 Hypertension is frequently arterial hypertension and coronary heart disease associated to metabolic disorders, such as insulin (CHD). In the PROCAM study, in men between 40 resistance with hyperinsulinaemia and dyslipidae- and 66 years of age, the prevalence of hypertension mia, which are additional risk factors of atheroscler- in patients who had a myocardial infarction was osis.9 14/1000 men in a follow-up of 4 years. -

Hypertension, Cholesterol, and Aspirin with Cost Info
Diabetes & Your Health High Blood Pressure & Diabetes Aspirin & Did you know as many as two out of three adults with Heart Health diabetes have high blood pressure? High blood pressure Studies have shown is a serious problem. It can raise your chances of stroke, that taking a low- heart attack, eye problems, and kidney disease. dose aspirin every Many people do not know they have high blood pressure day can lower the because they do not have any symptoms. That is why it risk for heart attack is often called “the silent killer.” and stroke. The only way to know if you have high blood pressure is Aspirin can help to have it checked. If you have diabetes, you should those who are at high have your blood pressure checked every time you see risk of heart attack, the doctor. People with diabetes should try to keep their such as people who blood pressure lower than 130 over 80. have diabetes or high blood pressure. Cholesterol & Diabetes Aspirin can also help Keeping your cholesterol and other blood fats, called lipids, under control can people with diabetes help you prevent diabetes problems. Cholesterol and blood lipids that are too who have already high can lead to heart attack and stroke. Many people with diabetes have had a heart attack or problems with their cholesterol and other lipid levels. a stroke, or who have heart disease. You will not know that your cholesterol and blood lipids are at dangerous levels unless you have a blood test to have them checked. Everyone with diabetes Taking an aspirin a should have cholesterol and other lipid levels checked at least once per year. -

Right Heart Pressures in Bronchial Asthma
Thorax: first published as 10.1136/thx.26.1.39 on 1 January 1971. Downloaded from Thorax (1971), 26, 39. Right heart pressures in bronchial asthma R. F. GUNSTONE St. George's Hospital, London S.W.1 Right heart pressures, electrocardiograms, blood gases, and peak expiratory flow rates were measured in nine patients admitted to hospital with severe bronchial asthma. Low or normal right heart pressures were found despite electrocardiographic changes in five patients consisting of right atrial P waves, abnormal right axis deviation, and in one patient T-wave changes in pre- cordial leads. These electrocardiographic changes reverted towards normal on recovery of the patient from the asthmatic attack. Electrocardiographic changes suggestive of right The procedure was carried out in the general ward heart embarrassment have been noted in acute with the patient in the sitting position supported at 60 bronchial asthma, particularly right atrial P waves to 90 degrees to the horizontal because orthopnoea (P and abnormal right axis deviation was always present. Immediately after catheterization pulmonale) the peak expiratory flow rate was measured with a (Harkavy and Romanoff, 1942; Miyamato, Wright peak flow meter (Wright and McKerrow, Bastaroli, and Hoffman, 1961; Ambiavagar, 1959) and blood (capillary or arterial) was taken for Jones and Roberts, 1967). These observations measurement of pH, Pco2, and standard bicarbonate raise the possibility that death in bronchial asthma by the Astrup method (Astrup, J0rgensen, Andersen, may be due to acute cor pulmonale although and Engel, 1960). The peak flow rate and electro- copyright. necropsy evidence is against this suggestion (Earle, cardiogram were repeated after recovery. -

Severe Asthma Is Associated with a Remodeling of the Pulmonary Arteries in Horses
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Severe asthma is associated with a remodeling of the pulmonary arteries in horses Remodeling of pulmonary arteries in severe equine asthma Serena Ceriotti1,2, Michela Bullone1, Mathilde Leclere1, Francesco Ferrucci2, Jean-Pierre Lavoie1* 1 Department of Clinical Sciences, Faculty of Veterinary Medicine, University of Montreal, Saint- Hyacinthe, Quebec, Canada 2 Department of Health, Animal Science and Food Safety, Università degli Studi di Milano, Milano, Italy Dr. Ceriotti current address is Department of Clinical Sciences, College of Veterinary Medicine, Auburn University, Auburn, Alabama, USA Dr. Bullone current address is Department of Veterinary Science, Università degli Studi di Torino, Grugliasco, Italy *Corresponding author: [email protected] Serena Ceriotti and Jean-Pierre Lavoie conceived and designed the work. Serena Ceriotti, Michela Bullone and Mathilde Leclere acquired clinical data, collected, processed and prepared histological and immunostained samples. Serena Ceriotti performed histomorphometric studies and statistical analysis. Serena Ceriotti, Jean-Pierre Lavoie and Francesco Ferrucci prepared and edited the manuscript prior to submission. Michela Bullone and Mathilde Leclere edited the manuscript prior to submission. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Major Clinical Considerations for Secondary Hypertension And
& Experim l e ca n i t in a l l C Journal of Clinical and Experimental C f a o r d l i a o Thevenard et al., J Clin Exp Cardiolog 2018, 9:11 n l o r g u y o Cardiology DOI: 10.4172/2155-9880.1000616 J ISSN: 2155-9880 Review Article Open Access Major Clinical Considerations for Secondary Hypertension and Treatment Challenges: Systematic Review Gabriela Thevenard1, Nathalia Bordin Dal-Prá1 and Idiberto José Zotarelli Filho2* 1Santa Casa de Misericordia Hospital, São Paulo, Brazil 2Department of scientific production, Street Ipiranga, São José do Rio Preto, São Paulo, Brazil *Corresponding author: Idiberto José Zotarelli Filho, Department of scientific production, Street Ipiranga, São José do Rio Preto, São Paulo, Brazil, Tel: +5517981666537; E-mail: [email protected] Received date: October 30, 2018; Accepted date: November 23, 2018; Published date: November 30, 2018 Copyright: ©2018 Thevenard G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Introduction: In this context, secondary arterial hypertension (SH) is defined as an increase in systemic arterial pressure (SAP) due to an identifiable cause. Only 5 to 10% of patients suffering from hypertension have a secondary form, while the vast majorities have essential hypertension. Objective: This study aimed to describe, through a systematic review, the main considerations on secondary hypertension, presenting its clinical data and main causes, as well as presenting the types of treatments according to the literary results. -

Surgical Techniques for Repair of Peripheral Pulmonary Artery Stenosis
STATE OF THE ART Surgical Techniques for Repair of Peripheral Pulmonary Artery Stenosis Richard D. Mainwaring, MD, and Frank L. Hanley, MD Peripheral pulmonary artery stenosis (PPAS) is a rare form of congenital heart disease that is most frequently associated with Williams and Alagille syndromes. These patients typically have systemic level right ventricular pressures secondary to obstruction at the lobar, segmental, and subseg- mental branches. The current management of patients with PPAS remains somewhat controversial. We have pioneered an entirely surgical approach for the reconstruction of PPAS. This approach initially entailed a surgical patch augmentation of all major lobar branches and effectively reduced the right ventricular pressures by more than half. This was the first report demonstrat- ing an effective approach to this disease. Over the past 5 years, we have An illustration demonstrating key steps in the surgical gradually evolved our technique of reconstruction to include segmental and technique for reconstruction of peripheral pulmonary artery stenosis. subsegmental branch stenoses. An important technical aspect of this approach entails the division of the main pulmonary and separation of the Central Message branch pulmonary arteries to access the lower lobe branches. Pulmonary artery homograft patches are used to augment hypoplastic pulmonary artery This article provides a detailed description of branches. In addition, we perform a Heinecke-Miculicz–type ostioplasty for the surgical techniques that have been devel- oped for the surgical reconstruction of periph- isolated ostial stenoses. The technical details of the surgical approach to eral pulmonary artery stenosis. PPAS are outlined in this article and can also be used for other complex peripheral pulmonary artery reconstructions. -

Allergic Bronchopulmonary Aspergillosis: Diagnostic and Treatment Challenges
y & Re ar sp Leonardi et al., J Pulm Respir Med 2016, 6:4 on ir m a l to u r P y DOI: 10.4172/2161-105X.1000361 f M o e Journal of l d a i n c r i n u e o J ISSN: 2161-105X Pulmonary & Respiratory Medicine Review Article Open Access Allergic Bronchopulmonary Aspergillosis: Diagnostic and Treatment Challenges Lucia Leonardi*, Bianca Laura Cinicola, Rossella Laitano and Marzia Duse Department of Pediatrics and Child Neuropsychiatry, Division of Allergy and Clinical Immunology, Sapienza University of Rome, Policlinico Umberto I, Rome, Italy Abstract Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disorder, occurring mostly in asthmatic and cystic fibrosis patients, caused by an abnormal T-helper 2 lymphocyte response of the host to Aspergillus fumigatus antigens. ABPA diagnosis is defined by clinical, laboratory and radiological criteria including active asthma, immediate skin reactivity to A. fumigatus antigens, total serum IgE levels>1000 IU/mL, fleeting pulmonary parenchymal opacities and central bronchiectases that represent an irreversible complication of ABPA. Despite advances in our understanding of the role of the allergic response in the pathophysiology of ABPA, pathogenesis of the disease is still not completely clear. In addition, the absence of consensus regarding its prevalence, diagnostic criteria and staging limits the possibility of diagnosing the disease at early stages. This may delay the administration of a therapy that can potentially prevent permanent lung damage. Long-term management is still poorly studied. Present primary therapies, based on clinical experience, are not yet standardized. These consist in oral corticosteroids, which control acute symptoms by mitigating the allergic inflammatory response, azoles and, more recently, anti-IgE antibodies. -

Pulmonary Hypertension ______
Pulmonary Hypertension _________________________________________ What is it? High blood pressure in the arteries that supply the lungs is called pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH). The blood pressure measured by a cuff on your arm isn’t directly related to the pressure in your lungs. The blood vessels that supply the lungs constrict and their walls thicken, so they can’t carry as much blood. As in a kinked garden hose, pressure builds up and backs up. The heart works harder, trying to force the blood through. If the pressure is high enough, eventually the heart can’t keep up, and less blood can circulate through the lungs to pick up oxygen. Patients then become tired, dizzy and short of breath. If a pre-existing disease triggered the PH, doctors call it secondary pulmonary hypertension. That’s because it’s secondary to another problem, such as a left heart or lung disorder. However, congenital heart disease can cause PH that’s similar to PH when the cause isn’t known, i.e., idiopathic or unexplained pulmonary arterial hypertension. In this case, the PAH is considered pulmonary arterial hypertension associated with congenital heart disease, such as associated with a VSD or ASD (either repaired or unrepaired). The problem is due to scarring in the small arteries in the lung. It’s important to repair congenital heart problems (when possible) before permanent pulmonary hypertensive changes develop. Intracardiac left-to-right shunts (such as a ventricular or atrial septal defect, a hole in the wall between the two ventricles or atria) can cause too much blood flow through the lungs. -

Uncontrolled Hypertension and Associated Factors Among Hypertensive Adults in Bale Zone Public Hospitals, Ethiopia Feyissa Lemessa1* and Miressa Lamessa2
ISSN: 2474-3690 Lemessa and Lemessa. J Hypertens Manag 2021, 7:057 DOI: 10.23937/2474-3690/1510057 Volume 7 | Issue 1 Journal of Open Access Hypertension and Management ORIGINAL RESEARCH Uncontrolled Hypertension and Associated Factors among Hypertensive Adults in Bale Zone Public Hospitals, Ethiopia Feyissa Lemessa1* and Miressa Lamessa2 1 Department of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia Check for 2Department of Emergency and Critical Care, St. Paul’s Hospital Millennium Medical College, Addis Ababa, updates Ethiopia *Corresponding author: Feyissa Lemessa Jinfessa, Department of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, Tel : +251-920-405-878 Abstract Conclusion: The prevalence of uncontrolled hypertension was high at the study area among patients with hyperten- Background: Although blood pressure control has tremen- sion. Being overweight and lack of awareness on Hyperten- dous public health benefit, and has effective treatments, the sion i.e. poor knowledge on hypertension management can global rate of uncontrolled blood pressure remains high. In result in hypertension-related complications. Hence, Con- sub-Saharan Africa including Ethiopia uncontrolled blood tinuous health education on lifestyle practices and hyper- pressure resulted in a significant morbidity and mortality. tension-related complications in each follow-up visit highly Unfortunately, uncontrolled hypertension among adult hy- recommended. pertensive patients remains unclear and has been inade- quately studied in Ethiopia, in the study area in particular. Keywords Objective of the study: This study assessed uncontrolled Uncontrolled hypertension, Self-care practice, Bale, Ethiopia hypertension and associated factors among adult hyperten- sive patients on follow up clinics in Bale Zone Public Hospi- tals, Ethiopia, 2017.