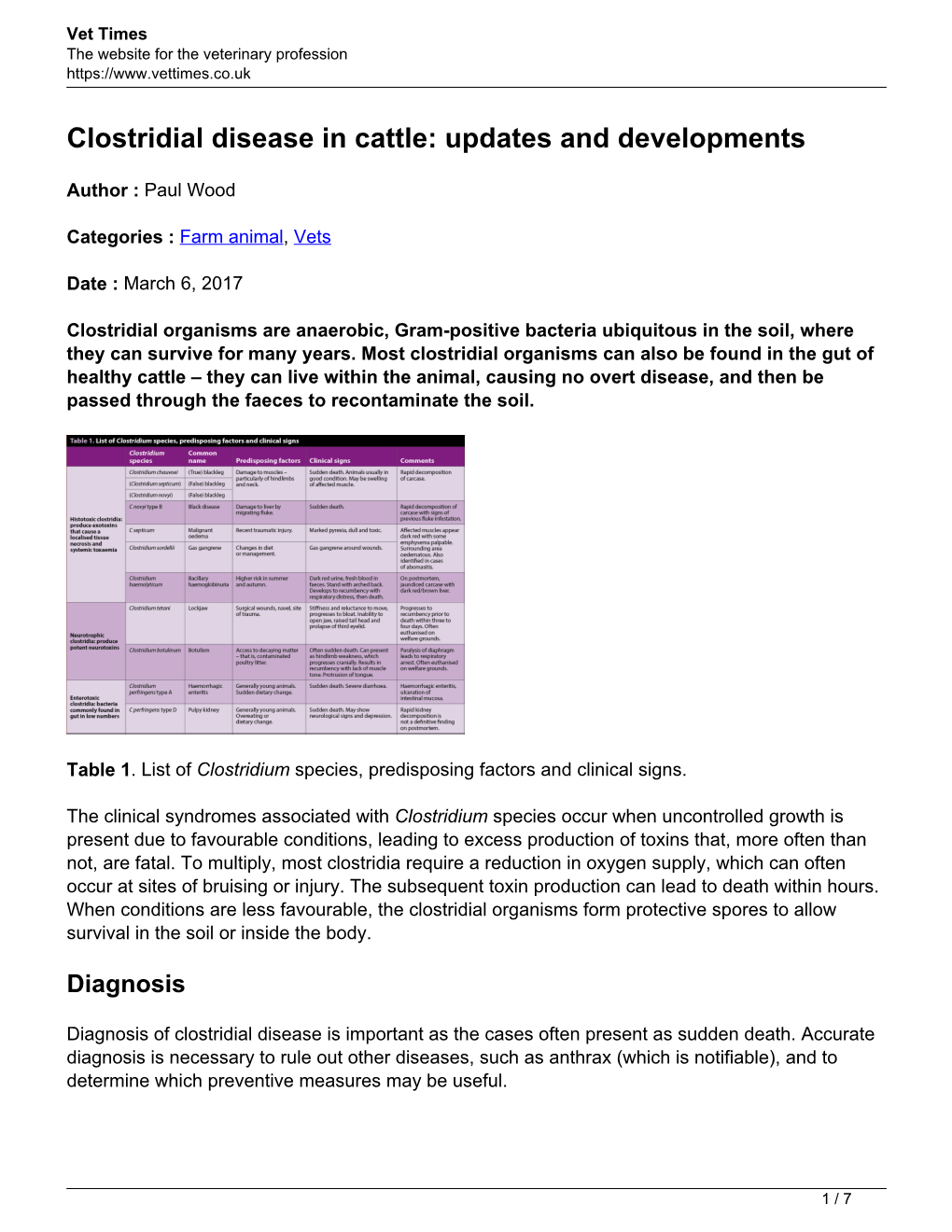
Clostridial Disease in Cattle: Updates and Developments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Clostridial Septicemia with Intravascular Hemolysis: a Case Report G
Henry Ford Hospital Medical Journal Volume 13 | Number 4 Article 4 12-1965 Clostridial Septicemia With Intravascular Hemolysis: A Case Report G. M. Mastio E. Morfin Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Mastio, G. M. and Morfin, E. (1965) "Clostridial Septicemia With Intravascular Hemolysis: A Case Report," Henry Ford Hospital Medical Bulletin : Vol. 13 : No. 4 , 421-425. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol13/iss4/4 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Henry Ford Hosp. Med. Bull. Vol. 13, December 1965 CLOSTRIDIAL SEPTICEMIA WITH INTRAVASCULAR HEMOLYSIS A CASE REPORT G. M. MASTIC, M.D. AND E. MORFIN, M.D. In 1871 Bottini' demonstrated the bacterial nature of gas gangrene, but failed to isolate a causal organism. Clostridium perfringens, sometimes known as Clostridium welchii, was discovered independently during 1892 and 1893 by Welch, Frankel, "Veillon and Zuber.^ This organism is a saprophytic inhabitant of the intestinal tract, and may be a harmless saprophyte of the female genital tract occurring in the vagina in 4-6 per cent of pregnant women. Clostridial organisms occur in great numbers and distribution throughout the world. Because of this, they are very common in traumatic wounds. Very few species of Clostridia, however, are pathogenic, and still fewer are capable of producing gas gangrene in man. -

Naeglaria and Brain Infections
Can bacteria shrink tumors? Cancer Therapy: The Microbial Approach n this age of advanced injected live Streptococcus medical science and into cancer patients but after I technology, we still the recipients unfortunately continue to hunt for died from subsequent innovative cancer therapies infections, Coley decided to that prove effective and safe. use heat killed bacteria. He Treatments that successfully made a mixture of two heat- eradicate tumors while at the killed bacterial species, By Alan Barajas same time cause as little Streptococcus pyogenes and damage as possible to normal Serratia marcescens. This Alani Barajas is a Research and tissue are the ultimate goal, concoction was termed Development Technician at Hardy but are also not easy to find. “Coley’s toxins.” Bacteria Diagnostics. She earned her bachelor's degree in Microbiology at were either injected into Cal Poly, San Luis Obispo. The use of microorganisms in tumors or into the cancer therapy is not a new bloodstream. During her studies at Cal Poly, much idea but it is currently a of her time was spent as part of the undergraduate research team for the buzzing topic in cancer Cal Poly Dairy Products Technology therapy research. Center studying spore-forming bacteria in dairy products. In the late 1800s, German Currently she is working on new physicians W. Busch and F. chromogenic media formulations for Fehleisen both individually Hardy Diagnostics, both in the observed that certain cancers prepared and powdered forms. began to regress when patients acquired accidental erysipelas (cellulitis) caused by Streptococcus pyogenes. William Coley was the first to use New York surgeon William bacterial injections to treat cancer www.HardyDiagnostics.com patients. -

Hawaii State Department of Health Tetanus Factsheet
TETANUS ABOUT THIS DISEASE Tetanus is an infection caused by a bacterium called Clostridium tetani. Spores of tetanus bacteria are everywhere in the environment, including soil, dust, and manure. These spores develop into bacteria when they enter the body through breaks in the skin, usually through injuries from contaminated objects. Clostridium tetani produce a toxin (poison) that causes painful muscle contractions. Tetanus is often called “lockjaw” because the first sign is most commonly spasms of the jaw muscles. Tetanus can lead to serious health problems, including being unable to open the mouth and having trouble swallowing and breathing, possibly leading to death (10% to 20% of cases). Tetanus is uncommon in the United States, with an average of 30 reported cases each year. Nearly all cases of tetanus in the U.S. are among people who have never received a tetanus vaccine, or adults who don’t stay up to date on their 10-year booster shots. SIGNS AND SYMPTOMS Symptoms of tetanus include: • Jaw cramping • Sudden, involuntary muscle tightening (muscle spasms) – often in the stomach • Painful muscle stiffness all over the body • Trouble swallowing • Jerking or staring (seizures) • Headache • Fever and sweating • Changes in blood pressure and a fast heart rate. Serious health problems that can happen because of tetanus include: • Laryngospasm (uncontrolled/involuntary tightening of the vocal cords) • Fractures (broken bones) • Hospital-acquired infections (Infections caught by a patient during a hospital stay) • Pulmonary embolism (blockage of the main artery of the lung or one of its branches by a blood clot that has travelled from elsewhere in the body through the bloodstream) • Aspiration pneumonia (lung infection that develops by breathing in foreign materials) • Breathing difficulty, possibly leading to death (1 to 2 in 10 cases are fatal) TRANSMISSION Tetanus is different from other vaccine-preventable diseases because it does not spread from person to person. -

Safety and Immunogenicity of Capsular Polysaccharide–Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib
142 Safety and Immunogenicity of Capsular Polysaccharide±Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib Carol J. Baker, Lawrence C. Paoletti, Section of Infectious Diseases, Departments of Pediatrics and of Michael R. Wessels, Hilde-Kari Guttormsen, Microbiology and Immunology, Baylor College of Medicine, Houston, Marcia A. Rench, Melissa E. Hickman, Texas; Channing Laboratory, Department of Medicine, Brigham and Women's Hospital, and Department of Microbiology and Molecular and Dennis L. Kasper Genetics, Harvard Medical School, Boston, Massachusetts About 40% of invasive group B streptococcal (GBS) isolates are capsular polysaccharide Downloaded from https://academic.oup.com/jid/article/179/1/142/877598 by guest on 01 October 2021 (CPS) types Ia or Ib. Because infant and maternal GBS infections may be preventable by maternal vaccination, individual GBS CPS have been coupled to tetanus toxoid (TT) to prepare vaccines with enhanced immunogenicity. Immunogenicity in rabbits and protective capacity in mice of a series of type Ia- and Ib-TT conjugates increased with the degree of polysaccharide-to-protein cross-linking. In total, 190 healthy, nonpregnant women aged 18±40 years were randomized in four trials to receive Ia- or Ib-TT conjugate (dose range, 3.75±63 mg of CPS component), uncoupled Ia or Ib CPS, or saline. All vaccines were well-tolerated. CPS-speci®c IgG serum concentrations peaked 4±8 weeks after vaccination and were signif- icantly higher in recipients of conjugated than of uncoupled CPS. Immune responses to the conjugates were dose-dependent and correlated in vitro with opsonophagocytosis. These re- sults support inclusion of Ia- and Ib-TT conjugates when formulating a multivalent GBS vaccine. -

Sheep Diseases the FARMERS’ GUIDE 2Nd Edition - July 2015 Sheep Diseases the FARMERS’ GUIDE
Sheep Diseases THE FARMERS’ GUIDE 2nd Edition - July 2015 Sheep Diseases THE FARMERS’ GUIDE Developed by: Emily Litzow for Primary Industries and Regions South Australia, Biosecurity SA Animal Health Funded by: SA Sheep Industry Fund and Biosecurity SA Use of the information/advice in this guide is at your own risk. The Department of Primary Industries and Regions SA and its employees do not warrant or make any representation regarding the use, or results of the use, of the information contained herein as regards to its correctness, accuracy, reliability, currency or otherwise. The entire risk of the implementation of the information/ advice which has been provided to you is assumed by you. All liability or responsibility to any person using the information/advice is expressly disclaimed by the Department of Primary Industries and Regions SA and its employees. 2 Acknowledgements and Further Reading The Information in this publication has been collected from: Allan, S 2010, Foot Abscess in Sheep, NSW DPI Primefact 7, NSW. Animal Biosecurity Unit 2008, Ovine Johne’s Disease, NSW DPI Primefact 661, NSW. Australian Animal Welfare Standards and Guidelines - Land Transport of Livestock, Animal Health Australia (AHA) 2012, Canberra. Brightling, A 2006, Livestock Diseases in Australia, C H Jerram and Associates Science Publishers, Australia. Butler, R 2008, Ovine Brucellosis, Department of Agriculture and Food Farmnote 334, WA. Chester, L 2010, Sheep Welfare – Avoiding Losses due to Hypothermia, Department of Agriculture and Food Farmnote 453, WA. Cotter, J 2011, Sheep Lice – Spread and Detection, Department of Agriculture and Food Farmnote 478, WA. Erickson, A 2010, Hydatid Disease, Department of Agriculture and Food Farmnote 448, WA. -

Blackleg and Clostridial Diseases
DIVISION OF AGRICULTURE RESEARCH & EXTENSION UJA--University of Arkansas System Agriculture and atural Resources FSA3073 Livestock Health eries Blackleg and Other Clostridial Diseases symptoms. Therefore, prevention of Heidi Ward, Introduction these diseases through immunization VM, Ph Clostridial bacteria cause several is more successful than trying to treat Assistant Professor diseases that affect cattle and other infected animals. and Veterinarian farm animals. This group of bacteria is known to produce toxins with varying effects based on the way they enter the Blackleg Jeremy Powell, body. The bacteria are frequently Blackleg, or clostridial myositis, VM, Ph found in the environment (primarily in affects cattle worldwide and is caused Professor the soil) and tend to multiply in warm by Clostridium chauvoei. Susceptible weather following heavy rain. The animals first ingest endospores. The bacteria are also found in the intes - endospores then cross over the gastro - tinal tracts of healthy farm animals, intestinal tract and enter the blood- where they only cause disease under stream where they are deposited in certain circumstances. The most muscle tissue in the animal’s body. common diseases caused by clostridial They then lie dormant in the tissue bacteria in beef cattle are blackleg, until they become activated and enterotoxemia, malignant edema, black trigger the disease. disease and tetanus. These diseases Clostridium chauvoei is activated are usually seen in young cattle (less in an anaerobic (oxygen deficient) than 2 years of age) and are widely environment such as damaged, distributed throughout Arkansas. devitalized or bruised tissue. Events Bacteria of the Clostridium genus such as transport, rough handling or produce long-lived structures called aggressive pasture activity can lead to endospores. -

Studies Upon the Blackleg Disease of the Potato, with Special Reference to the Rela- Tionship of the Causal Organisms
STUDIES UPON THE BLACKLEG DISEASE OF THE POTATO, WITH SPECIAL REFERENCE TO THE RELA- TIONSHIP OF THE CAUSAL ORGANISMS By W. J. MORSE, Plant Pathologist, Maine Agricultural Experiment Station HISTORICAL REVIEW The fact that the potato (Solanum tuberosum) is subject to maladies like that under consideration in this paper was noted at a comparatively early date in the literature of bacterial diseases of plants. De Jubain- ville and Vesque (8)1 mentioned in 1878 a "cellular-rot" of potatoes, radishes, carrots, and beets as occurring in the soil and in cellars; but bacteria are not mentioned as the cause. Their paper and the one following are reviewed by Smith (32). In 1879 Reinke and Berthold (30) pointed out quite clearly that a wetrot of potatoes could occur without the presence of any fungi. According to Smith, they apparently did not have any active parasite and did not work with pure cultures. However, they were able to inoculate and cause a decay of healthy tubers by means of the watery fluid taken from diseased potatoes, provided especially favorable condi- tions were supplied in the line of moisture. They were also able to demonstrate the constant association of bacteria with the wetrotting of the tubers. Prillieux and Delacroix (28) described a disease of the potato stem from France in 1890 and gave the name "Bacillus caulivorus" to the organism which they considered to be the cause. Nothing is said in this paper as to the isolation of the organism and the growth of it in pure cultures, although later Prillieux (27, v. -

Skin and Soft Tissue Infections Ohsuerin Bonura, MD, MCR Oregon Health & Science University Objectives
Difficult Skin and Soft tissue Infections OHSUErin Bonura, MD, MCR Oregon Health & Science University Objectives • Compare and contrast the epidemiology and clinical presentation of common skin and soft tissue diseases • State the management for skin and soft tissue infections OHSU• Differentiate true infection from infectious disease mimics of the skin Casey Casey is a 2 year old boy who presents with this rash. What is the best treatment? A. Soap and Water B. Ibuprofen, it will self OHSUresolve C. Dicloxacillin D. Mupirocin OHSUImpetigo Impetigo Epidemiology and Treatment OHSU Ellen Ellen is a 54 year old morbidly obese woman with DM, HTN and venous stasis who presented with a painful left leg and fever. She has had 3 episodes in the last 6 months. What do you recommend? A. Cefazolin followed by oral amoxicillin prophylaxis B. Vancomycin – this is likely OHSUMRSA C. Amoxicillin – this is likely erysipelas D. Clindamycin to cover staph and strep cellulitis Impetigo OHSUErysipelas Erysipelas Risk: lymphedema, stasis, obesity, paresis, DM, ETOH OHSURecurrence rate: 30% in 3 yrs Treatment: Penicillin Impetigo Erysipelas OHSUCellulitis Cellulitis • DEEPER than erysipelas • Microbiology: – 6-48hrs post op: think GAS… too early for staph (days in the making)! – Periorbital – Staph, Strep pneumoniae, GAS OHSU– Post Varicella - GAS – Skin popping – Staph + almost anything! Framework for Skin and Soft Tissue Infections (SSTIs) NONPurulent Purulent Necrotizing/Cellulitis/Erysipelas Furuncle/Carbuncle/Abscess Severe Moderate Mild Severe Moderate Mild I&D I&D I&D I&D IV Rx Oral Rx C&S C&S C&S C&S Vanc + Pip-tazo OHSUEmpiric IV Empiric MRSA Oral MRSA TMP/SMX Doxy What Are Your “Go-To” Oral Options For Non-Purulent SSTI? Amoxicillin Doxycycline OHSUCephalexin Doxycycline Trimethoprim-Sulfamethoxazole OHSU Miller LG, et al. -

TETANUS in ANIMALS — SUMMARY of KNOWLEDGE Malinovská, Z
DOI: 10.2478/fv-2020-0027 FOLIA VETERINARIA, 64, 3: 54—60, 2020 TETANUS IN ANIMALS — SUMMARY OF KNOWLEDGE Malinovská, Z., Čonková, E., Váczi, P. Department of Pharmacology and Toxicology University of Veterinary Medicine and Pharmacy in Košice, Komenského 73, 041 81 Košice Slovakia [email protected] ABSTRACT the effects of the neurotoxin. The treatment is difficult with an unclear prognosis. Tetanus is a neurologic non-transmissible disease (often fatal) of humans and other animals with a world- Key words: animal; Clostridium tetani; toxin; spasm; wide occurrence. Clostridium tetani is the spore produc- treatment ing bacillus which causes the bacterial disease. In deep penetrating wounds the spores germinate and produce a toxin called tetanospasmin. The main characteristic sign INTRODUCTION of tetanus is a spastic paralysis. A diagnosis is usually based on the clinical signs because the detection in the Of the clostridial neurotoxins, botulinum neurotoxin wound and the cultivation of C. tetani is very difficult. and tetanus neurotoxin are the most potent toxins [15]. Between animal species there is considerable variabili- Their extraordinary toxicity is caused by neurospecificity ty in the susceptibility to the bacillus. The most sensi- and metalloprotease activity, which results in the paralysis. tive animal species to the neurotoxin are horses. Sheep Tetanus is potentially a fatal disease and in some countries and cattle are less sensitive and tetanus in these animal it is still very active. Tetanus is a traumatic clostridiosis, species are less common. Tetanus in cats and dogs are an infection in humans and other animals with worldwide rare and dogs are less sensitive than cats. -

Phylogenetic Positions of Clostridium Novyi and Clostridium
International Journal of Systematic and Evolutionary Microbiology (2001), 51, 901–904 Printed in Great Britain Phylogenetic positions of Clostridium novyi NOTE and Clostridium haemolyticum based on 16S rDNA sequences 1 National Veterinary Assay Yoshimasa Sasaki,1 Noriyasu Takikawa,2 Akemi Kojima,1 Laboratory, 1-15-1, 3 1 1 Tokura, Kokubunji, Tokyo Mari Norimatsu, Shoko Suzuki and Yutaka Tamura 185-8511, Japan 2 Research Center for Author for correspondence: Yoshimasa Sasaki. Tel: j81 42 321 1841. Fax: j81 42 321 1769. Veterinary Science, The e-mail: sasakiy!nval.go.jp Kitasato Institute, 6-111, Arai, Kitamoto, Saitama, 364-0026, Japan The partial sequences (1465 bp) of the 16S rDNA of Clostridium novyi types A, B 3 Institute for Animal and C and Clostridium haemolyticum were determined. C. novyi types A, B and Health, Compton, Newbury RG20 7NN, UK C and C. haemolyticum clustered with Clostridium botulinum types C and D. Moreover, the 16S rDNA sequences of C. novyi type B strains and C. haemolyticum strains were completely identical; they differed by 1 bp (level of similarity S 999%) from that of C. novyi type C, they were 987% homologous to that of C. novyi type A (relative positions 28–1520 of the Escherichia coli 16S rDNA sequence) and they exhibited a higher similarity to the 16S rDNA sequence of C. botulinum types D and C than to that of C. novyi type A. These results suggest that C. novyi types B and C and C. haemolyticum may be one independent species generated from the same phylogenetic origin. Keywords: Clostridium novyi types A, B and C, Clostridium haemolyticum, 16S rRNA analysis Clostridium novyi is divided into three types, A, B and duction of alpha (necrotizing) toxin, observed only in C. -

Blackleg in Cattle: Current Understanding and Future Research Needs
Ciência Rural, Santa Maria, v.48:05,Blackleg e20170939,in cattle: current 2018 understanding and future research http://dx.doi.org/10.1590/0103-8478cr20170939 needs. 1 ISSNe 1678-4596 MICROBIOLOGY Blackleg in cattle: current understanding and future research needs Rosangela Estel Ziech1* Leticia Trevisan Gressler2 Joachim Frey3 Agueda Castagna de Vargas1 1Departamento de Medicina Veterinária Preventiva, Universidade Federal de Santa Maria (UFSM), 97105-900, Santa Maria, RS, Brasil. E-mail: [email protected]. *Corresponding author. 2Instituto Federal Farroupilha (IFFar), Frederico Westphalen, RS, Brasil. 3Institute of Veterinary Bacteriology, Vetsuisse Faculty, University of Bern, Bern, Switzerland. ABSTRACT: Blackleg is an endogenous acute infection that principally affects cattle, whose etiologic agent is the anaerobic bacterium Clostridium chauvoei. In recent years, the major virulence factors of C. chauvoei have been discovered and described. However, the pathogenesis of blackleg in cattle, and in particular, the movement of the pathogen from the point of entry to the affected tissues is not yet fully elucidated. Disease control is based on appropriate management and vaccination. This review summarizes the latest research findings that contribute toward the understanding of the disease in cattle, provide a foundation to preventive strategies, and identify future research needs. Key words: Clostridium chauvoei, sudden death, myonecrosis. Carbúnculo sintomático: compreensão atual e futuras necessidades de pesquisa RESUMO: O carbúnculo sintomático é uma infecção endógena, aguda, que acomete principalmente bovinos, cujo agente etiológico é a bactéria anaeróbica Clostridium chauvoei. Recentemente, os principais fatores de virulência do C. chauvoei foram descobertos e descritos. Contudo, a patogênese do carbúnculo sintomático em bovinos, especialmente a circulação do patógeno desde o ponto de entrada até os tecidos acometidos ainda não está completamente elucidada. -

Blackleg ( Clostridium Chauvoei Infection) in Beef Calves: a Review and Presentation of Two Cases with Uncommon Pathologic Presentations
PEER REVIEWED Blackleg ( Clostridium chauvoei Infection) in Beef Calves: A Review and Presentation of Two Cases with Uncommon Pathologic Presentations 1 2 Russell F. Daly ·, DVM; Dale W. Miskimins1, DVM, MS; Roland G. Good , DVM; Thomas Stenberg', DVM 1Veterinary Science Department, South Dakota State University, Brookings, SD 57007 2Parker Veterinary Clinic, Parker, SD 57053-5661 3Volga Veterinary Clinic, Volga, SD 57071-2006 *Corresponding author: Russ Daly, 605-688-6589 Office, [email protected] Abstract laires sont bien connues et incluent des changements sous cutanes gelatineux et gazeux de meme que des Blackleg (Clostridium chauvoei infection) has long necroses musculaires bien demarquees. Des zones de been recognized as a cause of death in calves grazing necrose peuvent aussi etre presentes dans le myocarde, summer pastures. Clinical signs are not often observed le diaphragme et la langue par exemple. Les lesions in affected calves due to the peracute nature of the macroscopiques primaires chez les animaux examines disease, but may include fever, lameness, and swelling etaient associees a des pleuresies et a des pericardites. and crepitation over large muscle groups, followed by Des lesions de charbon symptomatique plus typiques se collapse and death. Typical gross and histopathologic retrouvaient chez certains mais pas chez tous les veaux lesions in these muscle groups are well-described and atteints et incluaient une necrose dans les muscles de include gelatinous, gassy subcutaneous changes, along la cuisse et de l'abdomen, une decoloration foncee du with well-defined muscle necrosis. Areas of necrosis can muscle du diaphragme et des indices histologiques de also be present in myocardium, diaphragm, and tongue, myocardite necrotique.