1 1 Abstract in Recent Years There Has Been Growing Concern About Concussion in Sport in General and Rugby Union in Particular
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Irish Rugby Injury Surveillance Project
IRIS The Irish Rugby Injury Surveillance Project All-Ireland League Amateur Club Rugby 2018-2019 Season Report IRIS Authored by the Irish Rugby Injury Surveillance (IRIS) Project Steering Group IRFU: Dr. Rod McLoughlin (Medical Director, IRFU) Ms. Mairéad Liston (Medical Department Co-ordinator, IRFU) Principal Investigators: Dr. Tom Comyns (Strength and Conditioning, University of Limerick) Dr. Ian Kenny (Biomechanics, University of Limerick) Supporting Investigators: Dr. Róisín Cahalan (Doctoral Supervisor, Physiotherapy, University of Limerick) Dr. Mark Campbell (Doctoral Supervisor, Sport Psychology, University of Limerick) Prof. Liam Glynn (Graduate Entry Medicine, University of Limerick) Mr. Alan Griffin (Doctoral Researcher, Sport Sciences, University of Limerick) Prof. Drew Harrison (Biomechanics, University of Limerick) Ms. Therese Leahy (Doctoral Researcher, Physiotherapy, University of Limerick) Dr. Mark Lyons (Doctoral Supervisor, Strength and Conditioning, University of Limerick) Dr. Helen Purtill (Mathematics and Statistics, University of Limerick) Dr. Giles Warrington (Sport and Exercise Physiology, University of Limerick) Ms. Caithríona Yeomans (Doctoral Researcher, Physiotherapy, University of Limerick)* The authors would like to acknowledge with considerable gratitude, the work of the doctors, physiotherapists and club staff involved with the IRIS clubs who have recorded injury information throughout the project. *Report Primary Author (ii) Contents The IRIS team (ii) 4.4 Nature of Training Injuries 28 4.5 Training Injury -

In Amateur Rugby Union Irfu Guide To
IRFU GUIDE TO IN AMATEUR RUGBY UNION THE AIM OF THIS BROCHURE IS TO PROVIDE INFORMATION ON CONCUSSION TO THOSE INVOLVED IN RUGBY UNION IN IRELAND. > Concussion MUST be taken extremely seriously. > Any player with a suspected concussion MUST be removed immediately from training/play and not return. > They MUST complete the Graduated Return to Play Protocol. > Concussion is treatable. RECOGNISE AND REMOVE PAGE 1 WHAT IS CONCUSSION? Sports related concussion is a traumatic brain injury that is caused by a direct force to the head or a force elsewhere in the body which is transmitted to the head. Concussion results in temporary impairment of brain function. However, in some cases, signs and symptoms evolve over a number of minutes to hours. What causes it? Concussion can be caused by a blow to the head or from a whiplash type movement of the head and neck that can occur when a player is tackled or collides with another player or the ground. Concussion Facts: > You do not have to lose consciousness to suffer from a concussion. > The effects of concussion cannot be seen on standard x-ray, CT scan or MRI. > Concussion can occur in a game or at training. > The onset of the effects of concussion may be delayed for up to 24–48 hours. > Symptoms generally resolve over a period of days or weeks but in some cases can be more prolonged. > Most doctors would argue that the physical benefits of taking part in contact sports outweigh the potential risks associated with sports related concussion. Concussion is treatable. -

Injuries in Amateur Male and Female Rugby Union
Injuries in Amateur Male and Female Rugby Union Caithríona Yeomans, MSc, BSc Supervisors Dr Thomas Comyns Dr Ian Kenny Dr Róisín Cahalan Thesis submitted to the University of Limerick, in fulfilment of the requirements for the degree of Doctor of Philosophy Submitted to the University of Limerick, January 2020 Abstract Title: Injuries in Amateur Male and Female Rugby Union Author: Caithríona Yeomans Rugby Union (RU) is a physically demanding team sport, and while comprehensive injury surveillance has been conducted in professional cohorts, there is little consensus regarding the incidence of injury in the amateur game. Aim: To establish and compare the incidence, nature and mechanism of injuries occurring in male and female amateur RU in Ireland. Methods: A systematic research strategy was undertaken, comprising; 1) A critical review of existing literature, 2) A national survey investigating injury monitoring practices in Irish amateur RU, 3) The design and development of a bespoke web-based surveillance system, and 4) An investigation into injury incidence and aetiology in amateur RU. Results: A pooled incidence rate of 46.8/1,000 player hours was calculated from six previously published epidemiological studies. Injury monitoring in Irish amateur RU varied widely and lacked a systematic approach, therefore a comprehensive surveillance system was designed and developed. Injury data were recorded from 25 male teams (959 players; 38±8 players/team) and eight female teams (234 players; 29±13 players/team) over two seasons. Females had a lower match injury incidence rate compared to males (35.6/1,000 player hours versus 49.1/1,000 player hours). -

Background: the Irish Rugby Football Union (IRFU) Is the Governing Body for Rugby Union in Ireland
Background: The Irish Rugby Football Union (IRFU) is the governing body for Rugby Union in Ireland. The IRFU is responsible for the development of the sport in schools, colleges and clubs and is one of the member unions of World Rugby (formally the International Rugby Board (IRB)). The IRFU are inviting tenders for the development and implementation of a long-term high quality injury surveillance and prevention programme across rugby union within the amateur game. We are currently seeking applications from individuals and/or organisations to partner on this project to commence in January 2016. Project Description and Aims: The objective of this injury surveillance project is to collect injury and prevention data from across the domestic game in Ireland (Ulster Bank League Level down to mini rugby). This would be a long-term funded project by the IRFU, which would provide continuous data for analysis. The preferred method is that of using a representative sample of clubs and/or schools, the data from which can be extrapolated into the wider game. While the long-term intent is for this to cover the whole game, it is anticipated that the project will have pilot phase and a staged roll out over a number of seasons at the different levels. Consideration should be given to the difficulties in conducting injury surveillance within community sport. It is widely recognised that injury surveillance at this level presents more challenges than at the elite end of the game, which has the trained personnel to record data (e.g. coaches, trainers, doctors, physiotherapists); an easily identifiable population; financial; and IT resources. -

The Irish Rugby Injury Surveillance Project
IRIS The Irish Rugby Injury Surveillance Project All-Ireland League Rugby 2017 - 2018 Season Report IRIS Authored by the Irish Rugby Injury Surveillance (IRIS) Project Steering Group IRFU: Dr. Rod McLoughlin (Medical Director, IRFU) Ms. Mairead Liston (Medical Department Co-ordinator, IRFU) Principal Investigators: Dr. Tom Comyns (Strength and Conditioning, University of Limerick) Dr. Ian Kenny (Biomechanics, University of Limerick) Supporting Investigators: Dr. Roisin Cahalan (Doctoral Supervisor, Physiotherapy, University of Limerick) Dr. Mark Campbell (Sport Psychology, University of Limerick) Prof. Liam Glynn (General Practice Medicine, University of Limerick) Prof. Drew Harrison (Biomechanics, University of Limerick) Dr. Kevin Hayes (Mathematics and Statistics, University of Limerick) Dr. Mark Lyons (Strength and Conditioning, University of Limerick) Dr. Giles Warrington (Sport and Exercise Physiology, University of Limerick) Ms. Caithriona Yeomans (Doctoral Researcher, Physiotherapy, University of Limerick) The authors would like to acknowledge with considerable gratitude, the work of the doctors, physiotherapists and club staff involved with the IRIS clubs who have recorded injury information throughout the project. (ii) Contents The IRIS team (ii) 4.3 Body Location of Training Injuries 22 4.4 Nature of Training Injuries 24 Contents (iii) 4.5 Training Injury Event 25 4.6 Training Injury Severity 26 Irish Rugby Football Union Foreword (v) 4.7 Training Injury Burden (number of injuries x time lost per injury) 27 4.8 Medical Attention -

Rugby League As a Televised Product in the United States of America
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Professional Projects from the College of Journalism and Mass Communications, College Journalism and Mass Communications of 7-31-2020 Rugby League as a Televised Product in the United States of America Mike Morris University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/journalismprojects Part of the Broadcast and Video Studies Commons, Communication Technology and New Media Commons, Journalism Studies Commons, and the Mass Communication Commons Morris, Mike, "Rugby League as a Televised Product in the United States of America" (2020). Professional Projects from the College of Journalism and Mass Communications. 23. https://digitalcommons.unl.edu/journalismprojects/23 This Article is brought to you for free and open access by the Journalism and Mass Communications, College of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Professional Projects from the College of Journalism and Mass Communications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Rugby League as a Televised Product in the United States of America By Mike Morris Abstract Rugby league is a form of rugby that is more similar to American football than its more globally popular cousin rugby union. This similarity to the United States of America’s most popular sport, that country’s appetite for sport, and its previous acceptance of foreign sports products makes rugby league an attractive product for American media outlets to present and promote. Rugby league’s history as a working-class sport in England and Australia will appeal to American consumers hungry for grit and authenticity from their favorite athletes and teams. -

Sport Matters 2017
IRISH SPORT DOES MATTER The Federation of Irish Sport is the representative body for Ireland’s National Sporting Organisations and the country’s 28 Local Sports Partnerships (LSP’s). The Federation works on behalf of its members to create a greater awareness of the importance of sport across a wide number of areas including health, business, tourism, community, diversity and the economy. Membership is comprised of : NGB’s LSP’s • Angling Council of Ireland • Irish Rugby Football Union • Carlow Sports Partnership • Archery Ireland • Irish Sailing Association • Cavan Sports Partnership • Athletics Ireland • Irish Squash • Clare Sports Partnership • Australian Rules Football League of Ireland • Irish Surfing • Cork Sports Partnership • Badminton Ireland • Irish Taekwondo Union • Donegal Sports Partnership • Basketball Ireland • Irish Ten Pin Bowling Association • Dublin City Sport and Wellbeing Partnership • Baton Twirling Association of Ireland • Irish Tug of War Association • Dun Laoghaire-Rathdown Sports Partnership • Bol Chumann na hEireann • Irish Underwater Council • Fingal Sports Partnership • Bowling League of Ireland • Irish Water Safety • Kerry Recreation and Sports Partnership • Canoeing Ireland • Irish Waterski and Wakeboard Federation • Kildare Sports Partnership • Comhairle Liathróid Láimhe na hÉireann • Irish Wheelchair Association • Kilkenny Recreation and Sports Partnership • Cricket Ireland • Ladies Gaelic Football Association • Laois Sports Partnership • Croquet Association of Ireland • Motor Cycling Ireland • Leitrim -

Cosgrave Pts Authors Accepted
Citation for published version: Cosgrave, M & Williams, S 2019, 'The epidemiology of concussion in professional rugby union in Ireland', Physical Therapy in Sport, vol. 35, pp. 99-105. https://doi.org/10.1016/j.ptsp.2018.11.010 DOI: 10.1016/j.ptsp.2018.11.010 Publication date: 2019 Document Version Peer reviewed version Link to publication Publisher Rights CC BY-NC-ND University of Bath Alternative formats If you require this document in an alternative format, please contact: [email protected] General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. Oct. 2021 The Epidemiology of Concussion in Professional Rugby Union in Ireland 1 Abstract Objectives: To determine incidence rates, severity and the nature of concussion in professional rugby union in Ireland. Design: Retrospective observational study of time-loss concussion. Setting: Professional rugby union in Ireland. Participants: 160 male professional rugby union players. Outcome measures: Incidence rates (concussion/1000 player-match-hours) and mean/median severity (days absence) of concussion. Results: This study observed 60 concussions in 47 players over the course of the 2016/17 season. The match concussion incidence rate was 18.4/1000 player- match-hours. Mean and median severity was 12 and 10 days respectively. -

THE PSYCHOSOCIAL IMPACT of CAREER-ENDING INJURIES in ELITE RUGBY UNION PLAYERS: a QUALITATIVE STUDY Diarmuid Hurley
THE PSYCHOSOCIAL IMPACT OF CAREER-ENDING INJURIES IN ELITE RUGBY UNION PLAYERS: A QUALITATIVE STUDY Diarmuid Hurley Master’s Thesis in Sport and Exercise Psychology Spring 2014 Department of Sport Sciences University of Jyväskylä ACKNOWLEDGEMENTS I would like to express my sincere gratitude to Dr. Montse Ruiz and Dr. Monna Arvinen-Barrow for their cooperation, patience and guidance over the course of writing this thesis. I was fortunate to have two knowledgeable supervisors who offered different and valuable perspectives on my work. Credit must also go to Dr. Mary Hassandra and my fellow classmates for their contributions, feedback and enthusiasm over the course of all those thesis seminars. This completion of this thesis marks the end of my two years as an EMSEP student and of my time in Finland. These two years have been the best of my life and this experience has been life changing. It will be with a heavy heart that I bid farewell to the city of Jyvaskyla and to my classmates whose friendship has grown from day one to be so special and with whom I have shared countless enjoyable moments. I will miss you all until the day we meet again. Finally, I would like to thank my parents for their continued support and patience with my academic endeavours. Perhaps upon completion of my degree, I will get one of those “jobs” they are always talking about. Seriously though, my completion of this degree would not have been possible without their support and I hope one day to be able to repay their unwavering generosity and kindness. -

'From Ludicrous to Logical: the Transformation of Sport in North Munster, 1850–1890. Thomas Hayes Ph. D. by Research And
‘From ludicrous to logical: the transformation of sport in North Munster, 1850–1890. Thomas Hayes Ph. D. by research and thesis Mary Immaculate College University of Limerick Supervisor: Dr. Maura Cronin September 2009 Acknowledgements Sincere thanks to Dr. Maura Cronin for patiently and wisely supervising this thesis. My gratitude to the Interim Research Council for Humanities and Social Science whose award of a scholarship enabled me to begin this work; it is now, thankfully, a dream realised. Commonly used abbreviations. LAAC Limerick Amateur Athletic Club LAABC Limerick Amateur Athletic and Bicycle Club LBC Limerick Boat Club LCC Limerick Coursing Club LCCC Limerick County Cricket Club LFC Limerick County Football Club LPYMA Limerick Protestant Young Men’s Association CLF County Limerick Foxhounds CLI Catholic Literary Institute SRC Shannon Rowing Club Dedication To my wonderful wife, Louise Anne Marnell. Contents Prologue……………1 Introduction………...3 Chapter 1………….20 Chapter 2………….97 Chapter 3………...214 Chapter 4………...268 Conclusion……....327 Epilogue…………333 Bibliography…….334 Prologue ‘O Captain! My captain.’ 1 In the summer of 2006, while driving between Castlemaine and Milltown in County Kerry on the way to a country house hotel, my wife and I encountered a large number of motorcyclists, extremely well attired and each in possession of an expensive designer vehicle; given the location it was not unduly fanciful to suggest they resembled latter day ‘wild colonial’ boys and girls. As a teenager my wife and I (separately) spent part of our social lives in an edgy pub in Limerick city frequented by many motorcycle enthusiasts and musicians. Those earlier male and female bikers affected an Easy Rider/Hell’s Angels attitude, but their youth, rebelliousness, coolness and angst appeared substantial, romantic and authentic. -

Genetic Factors That Could Affect Concussion Risk in Elite Rugby
sports Review Genetic Factors That Could Affect Concussion Risk in Elite Rugby Mark R. Antrobus 1,2,* , Jon Brazier 1,3 , Georgina K. Stebbings 1 , Stephen H. Day 4, Shane M. Heffernan 5, Liam P. Kilduff 5, Robert M. Erskine 6,7 and Alun G. Williams 1,7 1 Sports Genomics Laboratory, Department of Sport and Exercise Sciences, Manchester Metropolitan University, Manchester M1 5GD, UK; [email protected] (J.B.); [email protected] (G.K.S.); [email protected] (A.G.W.) 2 Sport and Exercise Science, University of Northampton, Northampton NN1 5PH, UK 3 Department of Psychology and Sports Sciences, University of Hertfordshire, Hatfield AL10 9AB, UK 4 Faculty of Science and Engineering, University of Wolverhampton, Wolverhampton WV1 1LY, UK; [email protected] 5 Applied Sports, Technology, Exercise and Medicine (A-STEM) Research Centre, College of Engineering, Swansea University, Swansea SA1 8EN, UK; [email protected] (S.M.H.); [email protected] (L.P.K.) 6 Research Institute for Sport & Exercise Sciences, Liverpool John Moores University, Liverpool L3 3AF, UK; [email protected] 7 Institute of Sport, Exercise and Health, University College London, London WC1E 6BT, UK * Correspondence: [email protected] Abstract: Elite rugby league and union have some of the highest reported rates of concussion (mild traumatic brain injury) in professional sport due in part to their full-contact high-velocity collision-based nature. Currently, concussions are the most commonly reported match injury during the tackle for both the ball carrier and the tackler (8–28 concussions per 1000 player match hours) and reports exist of reduced cognitive function and long-term health consequences that can end a Citation: Antrobus, M.R.; Brazier, J.; playing career and produce continued ill health. -
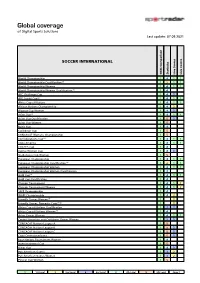
Sportradar Coverage List
Global coverage of Digital Sports Solutions Last update: 07.09.2021 SOCCER INTERNATIONAL Odds Comparison Statistics Live Scores Live Centre World Championship 1 4 1 1 World Championship Qualification (1) 1 2 1 1 World Championship Women 1 4 1 1 World Championship Women Qualification (1) 1 4 AFC Challenge Cup 1 4 3 AFF Suzuki Cup (6) 1 4 1 1 Africa Cup of Nations 1 4 1 1 African Nations Championship 1 4 2 Algarve Cup Women 1 4 3 Asian Cup (6) 1 4 1 1 Asian Cup Qualification 1 5 3 Asian Cup Women 1 5 Baltic Cup 1 4 Caribbean Cup 1 5 CONCACAF Womens Championship 1 5 Confederations Cup (1) 1 4 1 1 Copa America 1 4 1 1 COSAFA Cup 1 4 Cyprus Women Cup 1 4 3 SheBelieves Cup Women 1 5 European Championship 1 4 1 1 European Championship Qualification (1) 1 2 1 1 European Championship Women 1 4 1 1 European Championship Women Qualification 1 4 Gold Cup (6) 1 4 1 1 Gold Cup Qualification 1 4 Olympic Tournament 1 4 1 2 Olympic Tournament Women 1 4 1 2 SAFF Championship 1 4 WAFF Championship 1 4 2 Friendly Games Women (1) 1 2 Friendly Games, Domestic Cups (1) (2) 1 2 Africa Cup of Nations Qualification 1 3 3 Africa Cup of Nations Women (1) 1 4 Asian Games Women 1 4 1 1 Central American and Caribbean Games Women 1 3 3 CONCACAF Nations League A 1 5 CONCACAF Nations League B 1 5 3 CONCACAF Nations League C 1 5 3 Copa Centroamericana 1 5 3 Four Nations Tournament Women 1 4 Intercontinental Cup 1 5 Kings Cup 1 4 3 Pan American Games 1 3 2 Pan American Games Women 1 3 2 Pinatar Cup Women 1 5 1 1st Level 2 2nd Level 3 3rd Level 4 4th Level 5 5th Level Page: