Meniscal Injury.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Knee Flow Chart Acute
Symptom chart for acute knee pain START HERE Did the knee pain begin Does the knee joint You may have a fracture or Stop what you are doing immediately and go to a hospital emergency room YES YES suddenly, with an injury, appear deformed, or dislocated patella. or an orthopedic surgeon specializing in knee problems. slip, fall, or collision? out of position? If possible, splint the leg to limit the movement of the knee until you reach NO the doctor. Do not put any weight on the knee. Use a wheelchair, a cane, or NO crutch to prevent putting any weight on the leg, which might cause further damage to the joint. GO TO FLOW CHART #2 Go to an orthopedic surgeon Stop what you are doing. Continuing activity despite the feeling that the knee ON CHRONIC KNEE Did you hear a “pop” YES immediately, you may have is unstable can cause additional damage to other ligaments, meniscus , and PROBLEMS THAT DEVELOP and does your knee feel torn your anterior cruciate, or cartilage. Try ice on the knee to control swelling. Take anti-in ammatories OR WORSEN OVER TIME. unstable or wobbly? other ligaments in the knee. like Advil or Nuprin until your doctor’s appointment. About a third of ligament tears get better with exercises, a third may need a brace, and a third may need sur gery. NO Use R•I•C•E for sore knees Does your knee hurt YES You may have damaged the articular Try anti-in ammatories, as directed on the bottle, for two days to reduce R: Rest as you bend it? cartilage on the bottom of the the chronic in ammation. -
Isaac Newton Academy Revision Booklet- Exam 1
Isaac Newton Academy Revision Booklet- Exam 1 Component 01: Physical factors affecting performance 1.1 Applied anatomy and physiology 1.2 Physical training. Functions of the skeleton Location of Major Bones Bone stores crucial nutrients, minerals, and lipids and produces blood cells that nourish the body and play a vital role in protecting the body against infection. Bones have many functions, including the following: Support: Bones provide a framework for the attachment of muscles and other tissues. Bone Location Arm - humerus, radius and ulna. Hand - Carpals, Metacarpals and Phalanges. Sternum and Ribs. Femur – the thigh bone. Patella – the knee cap. Tibia – the shin bone, the larger of the two leg bones located below the knee cap. Fibula – the smaller of the two leg bones located below the knee cap. The OCR Spec expects us to know the following regarding synovial joints: The definition of a synovial joint, Articulating bones of the knee and elbow hinge joints and also the articulating bones of the shoulder and hip Ball and socket joints Hinge Joint- A hinge joint is found at the knee and the elbow, Synovial Joint- This is a freely moveable joint in thich the bones’ surfaces are covered Articulating bones of the elbow by cartilage and connected by joint are the Humerus radius fibrous connective tissue and Ulna . Articulating bones of capsule lines with synovial the knee are the Femur and fluid Tibia. Ball and socket joint- Allows a wide range of movement, they can be Articulating bones- These found at the hip and shoulder. are bones that move within a joint Articulating bones of the shoulder are Humerus and Scapula. -
An Evidence Based Medicine Understanding of Meniscus Injuries and How to Treat Them
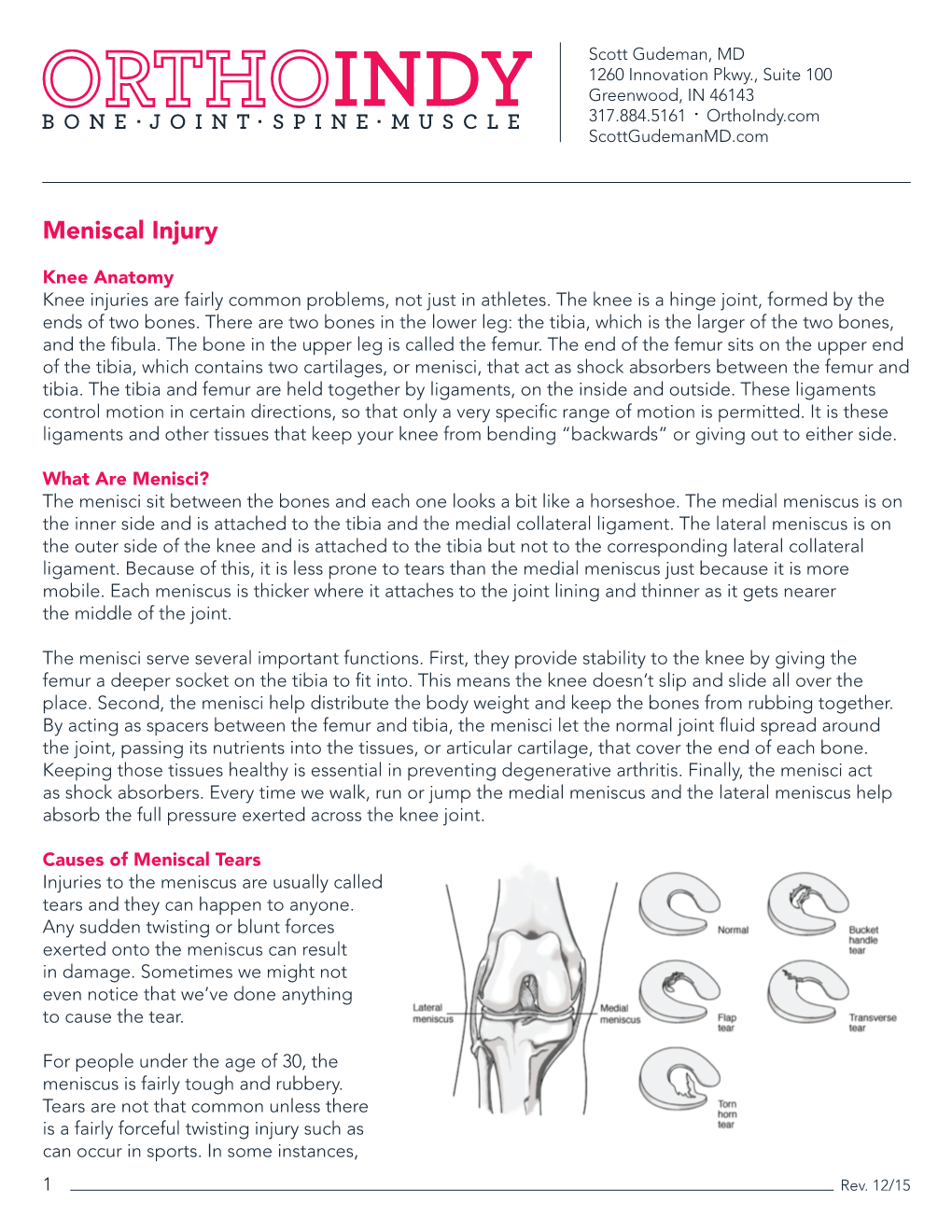
An Evidence Based Medicine Understanding of Meniscus Injuries and How to Treat Them Patrick S. Buckley, MD University Orthopaedic Associates June 1, 2019 Disclosures • None www.UOANJ.com Anatomy of the Meniscus • Act as functional extensions of the tibial plateaus to increase depth of tibial articular surface • The meniscotibial attachment contributes to knee stability • Triangular in cross-section Gross Anatomy of the Meniscus • Ultrastructural Anatomy – Primarily Type I collagen (90%) – 70% water – Fiber orientation is circumferential (hoop stressing) Meniscal Vascularity • Relatively avascular • Vascular penetration – 10 - 30% medial – 10 - 25% lateral • Non-vascularized portions gain nutrients from mechanical loading and joint motion Medial Meniscus • Semilunar shape • Thin anterior horn • Broader posterior horn • More stable & less motion than the lateral = tears more often Lateral Meniscus • Almost circular in shape • Intimately associated with the ACL tibial insertion • Posterior horn attachments – Ligament of Humphrey – Ligament of Wrisberg • Lateral meniscus is a more dynamic structure with more motion Main Importance of Menisci • Load transmission • Joint stability Load Bearing / Shock Absorption • MM 50% and 70% LM of load transmitted through mensicus in extension • 85 % at 90° of flexion • Meniscectomy – 50 % decrease in contact area – 20 % less shock absorption www.UOANJ.com Meniscal effect on joint stability • Secondary restraints to anterior tibial translation in normal knees • In an ACL-deficient knee: the posterior horn of the medial meniscus is more important than the lateral meniscus Interaction of ACL and PHMM • Lack of MM in ACLD knees significantly ↑ anterior tibial translation at all knee flexion angles • Think about with high grade pivot! (Levy, JBJS,1982) (Allen, JOR,2000) C9ristiani, AJSM, 2017) Meniscus Function -Now known to be important structure for load distribution and secondary stabilizer to the knee. -

Knee Joint Distraction Compared with Total Knee Arthroplasty a RANDOMISED CONTROLLED TRIAL
KNEE Knee joint distraction compared with total knee arthroplasty A RANDOMISED CONTROLLED TRIAL J. A. D. van der Woude, Aims K. Wiegant, Knee joint distraction (KJD) is a relatively new, knee-joint preserving procedure with the R. J. van Heerwaarden, goal of delaying total knee arthroplasty (TKA) in young and middle-aged patients. We S. Spruijt, present a randomised controlled trial comparing the two. P. J. E m ans , Patients and Methods S. C. Mastbergen, The 60 patients ≤ 65 years with end-stage knee osteoarthritis were randomised to either F. P. J. G. Lafeber KJD (n = 20) or TKA (n = 40). Outcomes were assessed at baseline, three, six, nine, and 12 months. In the KJD group, the joint space width (JSW) was radiologically assessed, From UMC Utrecht, representing a surrogate marker of cartilage thickness. Utrecht, The Netherlands Results In total 56 patients completed their allocated treatment (TKA = 36, KJD = 20). All patient reported outcome measures improved significantly over one year (p < 0.02) in both groups. J. A. D. van der Woude, MD, At one year, the TKA group showed a greater improvement in only one of the 16 patient- PhD, Resident in Orthopaedic Surgery, Limb and Knee related outcome measures assessed (p = 0.034). Outcome Measures in Rheumatology- Reconstruction Unit, Department of Orthopaedic Osteoarthritis Research Society International clinical response was 83% after TKA and 80% Surgery after KJD. A total of 12 patients (60%) in the KJD group sustained pin track infections. In the R. J. van Heerwaarden, MD, PhD, Orthopaedic Surgeon, KJD group both mean minimum (0.9 mm, standard deviation (SD) 1.1) and mean JSW (1.2 mm, Limb and Knee Reconstruction Unit, Department of SD 1.1) increased significantly (p = 0.004 and p = 0.0003). -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

Meniscus Tear
291 North Fireweed Soldotna, AK 99669 907-262-6454 www.kenaipeninsulaortho.com ______________________________________________________________________________________ Orthopaedic Surgeon: Hand and Wrist Specialist: Henry G. Krull, M.D. Edwin D. Vyhmeister, M.D. Meniscus Tear The meniscus is the rubbery, soft cartilage cushion in the knee. There are two of the C-shaped cushions in each knee, a medial (inner) and lateral (outer) meniscus. They sit between the two bones that form the knee joint, and function to cushion and support the knee. The meniscus can tear with injury or degeneration, or a combination of both. The medial meniscus is torn about 10X more frequently than the lateral meniscus. In young people, the meniscus usually tears with an injury. In older people, the cartilage can degenerate (weaken) with age, and can tear with or without an injury; spontaneous tears can occur. Meniscal tears can occur in association with other injuries to the knee. Symptoms: Pain is the usual symptom of complaint with a meniscus tear. There is often a noticeable “pop.” Swelling and stiffness can also occur. Mechanical symptoms are common—clicking, popping, and locking. Sometimes there is just a feeling that something is wrong inside the knee. Pain can be sharp, or can be dull and aching. Meniscus tears do not heal, but sometimes the symptoms dissipate. Chronic, intermittent symptoms is very common. Meniscal tears can cause a feeling of instability, or can cause the knee to buckle or give way. Cause: Injuries, particularly with sports, are a common cause of meniscal tears in young people. As people age, the meniscus tissue weakens through the normal degenerative process, and tears can occur spontaneously, or with simple activities, such as getting up from a chair, and changing direction while walking. -

About Your Knee
OrthoInfo Basics About Your Knee What are the parts of the knee? Your knee is Your knee is made up of four main things: bones, cartilage, ligaments, the largest joint and tendons. in your body Bones. Three bones meet to form your knee joint: your thighbone and one of the (femur), shinbone (tibia), and kneecap (patella). Your patella sits in most complex. front of the joint and provides some protection. It is also vital Articular cartilage. The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance to movement. helps your knee bones glide smoothly across each other as you bend or straighten your leg. Because you use it so Two wedge-shaped pieces of meniscal cartilage act as much, it is vulnerable to Meniscus. “shock absorbers” between your thighbone and shinbone. Different injury. Because it is made from articular cartilage, the meniscus is tough and rubbery to help up of so many parts, cushion and stabilize the joint. When people talk about torn cartilage many different things in the knee, they are usually referring to torn meniscus. can go wrong. Knee pain or injury Femur is one of the most (thighbone) common reasons people Patella (kneecap) see their doctors. Most knee problems can be prevented or treated with simple measures, such as exercise or Articular cartilage training programs. Other problems require surgery Meniscus to correct. Tibia (shinbone) 1 OrthoInfo Basics — About Your Knee What are ligaments and tendons? Ligaments and tendons connect your thighbone Collateral ligaments. These are found on to the bones in your lower leg. -

Arthroscopic Partial Meniscectomy 1
Chris Lena MD, James Alvarez PAC Arthroscopic and Reconstructive Surgery of the Shoulder and Knee Sports Medicine MEA’s Karen Smith, Jackie Zuidema, Annmarie Fiore Tel: (860) 549-8249 - FAX: (860) 244-8813 www.oahct.com Arthroscopic Partial Meniscectomy 1. ACTIVITIES: No harm is done in putting full weight on your knee immediately. You are encouraged to try to walk as smoothly as possible. Do not do any strenuous activity such as running and jumping until I clear you for this. You may experience some mild discomfort as you walk. You may use crutches, but generally they are not necessary. You may start bending your knee as tolerated, the sooner the better. 2. BANDAGES: Your bandage may be removed 2 days following surgery. The knee should then be re-wrapped with only the elastic bandage for about 3-4 days or until swelling is gone. DO NOT wrap the elastic bandage too tightly, or it will act like a tourniquet and cause ankle swelling. 3. MEDICATIONS: : A prescription will be provided to help relieve pain. Please use this medication as directed. This medication is strong, and should not be taken with alcohol or other pain medications, and may cause drowsiness. Exercise good judgment in its use. You may also try over the counter pain medications such as Aleve (naprosyn) or Advil (Ibuprofen). Take as directed unless there are contraindications. Take 1 Aspirin (325 mg) daily in addition to the pain medication. 4. SHOWER: You may shower after 48 hours. Do not take a bath or submerge the knee under water for 7 days. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Meniscus FAQ Robert T. Bents, MD
Meniscus FAQ Robert T. Bents, MD Q. What is a “meniscus”? A. The meniscus is a “C” shaped shock absorber in your knee joint. The meniscus is made of cartilage similar to your earlobe. The meniscus has several different functions‐shock absorption, joint stabilization, and joint instability. A healthy meniscus is important to protect against arthritis. Q. What does it mean to “tear” a meniscus? A. You can tear a meniscus in many different ways. As we get older the water content of the meniscus decreases and becomes more brittle. With twisting, squatting, or sporting activities the meniscus can be pinched between the femur and tibia causing it to fray, tear, or split. The tear may occur with injury or simply fray with aging. The most severe tears involve the attachment to the bone called the root. Q. What are some of the symptoms of a torn meniscus? A. Patients may have pain associated with twisting activities. The pain is usually localized along the inside (medial) or outside (lateral) part of the knee. Swelling of the joint is another common complaint. Sometimes patients will feel like something is catching or pinching in the joint. Occasionally the knee will “lock” in a certain position. Most of these symptoms are reproducible by the doctor’s examination. Q. Will an X‐ray detect a meniscal tear? A. No. The purpose of the X‐ray is to make certain that you do not have any underlying arthritis in your knee. Also a loose bone chips or “loose body” may mimic a meniscal tear. The X‐ray gives your doctor information about the “bony” anatomy of a joint. -

38.3 Joints and Skeletal Movement.Pdf
1198 Chapter 38 | The Musculoskeletal System Decalcification of Bones Question: What effect does the removal of calcium and collagen have on bone structure? Background: Conduct a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised. Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of bones that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones. Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours. Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments. Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest? Draw a conclusion: Did the results support or refute the hypothesis? How do the results observed in this experiment correspond to diseases that destroy bone tissue? 38.3 | Joints and Skeletal Movement By the end of this section, you will be able to do the following: • Classify the different types of joints on the basis of structure • Explain the role of joints in skeletal movement The point at which two or more bones meet is called a joint, or articulation. -

ANTERIOR KNEE PAIN Home Exercises
ANTERIOR KNEE PAIN Home Exercises Anterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including: • Weak or overused muscles • Chondromalacia of the patella (softening and breakdown of the cartilage on the underside of the kneecap) • Inflammations and tendon injury (bursitis, tendonitis) • Loose ligaments with instability of the kneecap • Articular cartilage damage (chondromalacia patella) • Swelling due to fluid buildup in the knee joint • An overload of the extensor mechanism of the knee with or without malalignment of the patella You may feel pain after exercising or when you sit too long. The pain may be a nagging ache or an occasional sharp twinge. Because the pain is around the front of your knee, treatment has traditionally focused on the knee itself and may include taping or bracing the kneecap, or patel- la, and/ or strengthening the thigh muscle—the quadriceps—that helps control your kneecap to improve the contact area between the kneecap and the thigh bone, or femur, beneath it. Howev- er, recent evidence suggests that strengthening your hip and core muscles can also help. The control of your knee from side to side comes from the glutes and core control; that is why those areas are so important in management of anterior knee pain. The exercises below will work on a combination of flexibility and strength of your knee, hip, and core. Although some soreness with exercise is expected, we do not want any sharp pain–pain that gets worse with each rep of an exercise or any increased soreness for more than 24 hours.