قائمة المستشفيات و العيادات المعتمدة Asbetar Hospital & Clinic Network
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Book Rskm5ub.Pdf
رؤيتنا الريادة يف خدمة جمتمع اﻷعمال رسالتنا دعم بيئة اﻷعمال من خﻻل تقديم خدمات جتارية واستشارية وقانونية وفقا ًﻷفضل املمارسات العاملية لتعزيز استدامة الرخاء اﻻقتصادي قيمنا التميز والريادة الرتكيز على املتعاملني الشراكات البناءة املسؤولية اجملتمعية العمل بروح الفريق املرونة والشفافية روح الوﻻء التعلم املؤسسي 1 Our Vision Leadership in Serving the Business Community Our Mission Business environment support through excellent services offering and finding promising investment opportunities locally, regionally and globally in order to achieve sustainable economic and social prosperity. Our Values Excellence & Leadership Focus on Customers Teamwork Transparency & accountability Knowledge Management Effective Communication Sustainability Strategic Partnerships and Alliances 2 إمجالي املنشآت املسجلة يف الغرفة خﻻل الربع الثاني من عام 2015 Total Number of Establishments registered with RAK Chamber during Second quarter of 2015 جدول رقم )Table no. (1( )1 عدد املنشآت Number of Establishment الشهر Month الرخص اجلديدة الرخص اجملددة الرخص امللغاة cancelled Licenses Renewed Licenses New Licenses أبريل April 85 1,636 208 مايو May 87 1,739 218 يونيو June 71 1,642 179 اﻹجمالي Total 243 5,017 605 3 إمجالي املنشآت العاملة يف القطاع اخلاص مصنفة حسب درجات العضوية خﻻل الربع الثاني من عام 2015 Total Number of Private Sector Establishments classified according to RAK Chamber membership categories during Second quarter of 2015 جدول رقم )Table no. (2( )2 احلصة النسبية عدد املنشآت الدرجة Grade Percentage Number of Establishments % اخلاصة Special 9.8 59 املمتازة Excellent 3 18 اﻷولى First 10.7 65 الثانية Second 44 266 الثالثة Third 30.7 186 الرابعة Fourth 1.8 11 اﻹجمالي Total 100 605 4 التوزيع النسيب للمنشآت حسب الشكل القانوني هلا خﻻل الربع الثاني من عام 2015 Relative Distribution of Establishments according to Legal status during Second quarter of 2015 جدول رقم )Table no. -

Provider's Name Location & Phone Doctor's Name Doctor's Specialty
Restricted Network (RN) Hospitals (Dubai) Provider's Name Location & Phone Doctor's Name Doctor's Specialty Iranian Hospital Al Wasl Road, Jumeirah 1, Dubai-UAE Kourosh Ghaznavi Internist 04-3440250 Pajman Kokabian General Physician Arzhang Mokhtarpour General Physician Iman Safari Geberal Physician Mohammad Semsar Kazerooni General Physician Safoora Hosseini General Physician Hamidreza Foroutan Paediatric cardiologist Vahid Baqeri Ophtalmologist Shahin Mirkhani ENT Zahra Vahedi Internist Seyed Ali Fakhraei Psychiatrist Ramin Vakilipour Neurologsit Gholamabbas Kiani General Physician Kuteni Safwan Radiologist Taban Rahjoo Urologist Mehran Karimi Oncologist Ehsan Sotoudeh General Surgeon Mohammad Ali Kheiry Internist Ahmed Maleki General Physician Leila Chamani Tabriz Infectious Diseases Specialist Seyed Mehrdad Solati Endocrinologist Masoud Sanatkar Cardiologist Afif Zarwi Urologist Fahimeh Mir Naseri Pediatrician Seyed Reza Safizadeh General Dentist Mehrdad Mirouliaei Endocrinologist (Pedia) Mahin Rasi Etemadi Gynecologist Syed Mahmoud Meraji Paediatric cardiologist Bachar Aboubaker Orthopedic Narges Pourheidari Dermatologist Fatemehsadat Miri Gynecologist Hooman Hooshangi Gastroenterologist Ali Nasser Tork Dermatologist Zina Molla Zeinali Cardiologist Fatemeh Tasdighi Pharmacist Leila Taban Pharmacist Soraya Shahrzad Cardiologist Kasem Hosseini Asl Gastroenterologist Zahra Sharghi General Physician Mehrnaz Ataei Naeini ENT Mahdi Ghodstehrani Neotologist Tabassom Enayatollahi Pharmacist Zahra Tavakoli Lemrasi Radiologist Behfar Jodeiri -

Lands & Properties Sector Real Estate Transactions Report First Half
Lands & Properties Sector Real Estate Transactions Report First Half 2018-2019 Lands & Properties Sector-Real Estate Transactions achieved more than AED 1.630 billion for the first half of 2019. According to the annual report issued by Lands & Properties Sector, a large number of Real Estate Transactions such as sales and mortgages of vouchers, documents and waivers were recorded. Of which included 1075 sales exceeding AED 566 million, 264 mortgages totaling more than AED 433 million dirhams and 586 waiver transactions totaling over AED 629 million. Table (1) Direction of Real Estate Transactions in Ras Al First Half First Half % % Percent Khaimah 2018 2019 Change Real Estate Sales 902,130,005 %31 566,723,734 %35 -37% Real Estate Mortgages 1,745,603,018 %60 433,978,003 %27 -75% Waivers Market Value 283,631,275 %10 629,622,861 %39 122% 1,630,324,59 Total Transactions 2,931,364,298 100% %100 -44% 8 Number of Sales 1412 %68 1,075 %56 -24% Number of Mortgages 297 %14 264 %14 -11% Number of Waivers 358 %17 586 %30 64% Total number of Real Estate Transactions 2,067 %100 1,925 %100 -7% Real Estate Transactions Highest Value Al Jazeera Al Jazeera Area Al Hamra Al Hamra In Table 1, we note a 44% decrease in the total value of Real Estate Transactions for the first half of 2019 compared to the first half of 2018, and a decrease in the total number of Real Estate Transactions by 7%. Vogue Areas by Real Estate Sales for the first half 2018/2019 The top 3 regions in terms of Real Estate Sales for the first half of 2018 in Ras Al Khaimah are: Al Jazeera Al Hamra, Julfar and Al Dhait. -
Mednet EBP Network OP IP MRE.Xlsx
Network Type EMIRATE CODE REGION FACILTY NAME PROVIDER TYPE STREET / AREA ADDRESS TELEPHONE EBP IN - PATIENT ABU DHABI H626 ABU DHABI SEHA EMIRATES HOSPITAL HOSPITAL AL NAHYAN CAMP AL LEDEEM STREET 02-4438999 EBP IN - PATIENT ABU DHABI H207 ABU DHABI AL RAHA HOSPITAL HOSPITAL AL NAJDA STREET AL NAJDA STREET , SECOND FLOOR , HYPER MARKET BUILDING 02-6330440 EBP IN - PATIENT AL AIN H29 AL AIN SPECIALISED MEDICAL CARE HOSPITAL HOSPITAL AL JAHLI STREET AL JAHLI STREET, NEAR AL AIN MUESUM 03-7552291 EBP IN - PATIENT DUBAI H39 ABU HAIL NEW MEDICAL CENTER HOSPITAL HOSPITAL ABUHAIL ROAD GALADARI ROUND ABOUT, OPP. RAMADA HOTEL, NEAR HOR AL ANZ BUS STATION 04-2689800 EBP IN - PATIENT DUBAI H130 JEBEL ALI CEDARS - JEBEL ALI INT'L HOSPITAL HOSPITAL JEBEL ALI ROAD OPP. RAMADA HOTEL, NEAR HOR AL ANZ BUS STATION 04-8814000 EBP IN - PATIENT DUBAI H142 NADHA 2 NMC SPECIALITY HOSPITAL HOSPITAL AL NADHA ROAD , NADHA 2 BEHIND SAHARA CENTER 04-2679999 EBP IN - PATIENT DUBAI H618 DIP NMC SPECIALITY HOSPITAL - DIP HOSPITAL DIP DUBAI INVESTMENT PARK 04-8108800 EBP IN - PATIENT DUBAI H667 MANKHOOL ASTER HOSPITAL BR OF ASTER DM HEALTHCARE- HOSPITAL MANKHOOL AL RAFA STREET 04-3814800 EBP IN - PATIENT ABU DHABI H172 ABU DHABI LLH HOSPITAL L.L.C. HOSPITAL ELECTRA STREET ELECTRA STREET, AL MARWA BUILDING 02-6335522 EBP IN - PATIENT ABU DHABI H419 ABU DHABI LIFECARE HOSPITAL HOSPITAL WATHBA BANIYAS STREET, WATHBA, GATE NO. 6 AL RAHA VILLAGE 02-5856333 EBP IN - PATIENT ABU DHABI H612 MUSAFFAH LIFECARE HOSPITAL LLC-BRANCH 1-LIFELINE HOSPITAL MUSAFFAH MUSAFFAH 02-5566666 EBP IN - PATIENT ABU DHABI H198 MUSAFFAH LLH HOSPITAL AL MUSAFFAH LLC HOSPITAL MUSAFFAH MUSSAFAH, ALI KAHBOUS AL ZAABI 02-5557711 EBP IN - PATIENT AL AIN H180 AL AIN NMC SPECIALTY HOSPITAL - AL AIN - NMC GROUP / HOSPITAL AL MUTAREDH AREA OUD AL HASSA STREET, AL MUTAREDH 03-7555999 EBP IN - PATIENT SHARJAH H168 TAWAUN W. -
Provider Name Network Type Type
Provider Name Network Type Type WELCARE HOSPITAL PREMIUM NETWORK Hospital WELCARE HOSPITAL FOR PREMIUM NETWORK - BUPA Hospital IRANIAN HOSPITAL COMPREHENSIVE NETWORK Hospital IRANIAN HOSPITAL RESTRICTED NETWORK Hospital IRANIAN HOSPITAL PREMIUM NETWORK Hospital IRANIAN HOSPITAL FOR PREMIUM NETWORK - BUPA Hospital BELHOUL EUROPEAN HOSPITAL COMPREHENSIVE NETWORK Hospital BELHOUL EUROPEAN HOSPITAL RESTRICTED NETWORK Hospital BELHOUL EUROPEAN HOSPITAL PREMIUM NETWORK Hospital BELHOUL EUROPEAN HOSPITAL FOR PREMIUM NETWORK - BUPA Hospital AL RAZI POLYCLINIC COMPREHENSIVE NETWORK Clinic AL RAZI POLYCLINIC RESTRICTED NETWORK Clinic AL RAZI POLYCLINIC PREMIUM NETWORK Clinic AL RAZI POLYCLINIC FOR PREMIUM NETWORK - BUPA Clinic DR. MOHD. SHOWKAT AL ZUBAIDY COMPREHENSIVE NETWORK Clinic DR. MOHD. SHOWKAT AL ZUBAIDY RESTRICTED NETWORK Clinic DR. MOHD. SHOWKAT AL ZUBAIDY PREMIUM NETWORK Clinic DR. MOHD. SHOWKAT AL ZUBAIDY FOR PREMIUM NETWORK - BUPA Clinic NEW EMIRATES MEDICAL CENTRE COMPREHENSIVE NETWORK Clinic NEW EMIRATES MEDICAL CENTRE RESTRICTED NETWORK Clinic NEW EMIRATES MEDICAL CENTRE PREMIUM NETWORK Clinic NEW EMIRATES MEDICAL CENTRE FOR PREMIUM NETWORK - BUPA Clinic DR. NASSER'S CLINIC COMPREHENSIVE NETWORK Clinic DR. NASSER'S CLINIC RESTRICTED NETWORK Clinic DR. NASSER'S CLINIC PREMIUM NETWORK Clinic DR. NASSER'S CLINIC FOR PREMIUM NETWORK - BUPA Clinic NEW MEDICAL CENTRE HOSP (DXB) COMPREHENSIVE NETWORK Hospital NEW MEDICAL CENTRE HOSP (DXB) RESTRICTED NETWORK Hospital NEW MEDICAL CENTRE HOSP (DXB) PREMIUM NETWORK Hospital NEW MEDICAL CENTRE HOSP (DXB) FOR PREMIUM NETWORK - BUPA Hospital AL NOOR POLYCLINIC COMPREHENSIVE NETWORK Clinic AL NOOR POLYCLINIC RESTRICTED NETWORK Clinic AL NOOR POLYCLINIC PREMIUM NETWORK Clinic AL NOOR POLYCLINIC FOR PREMIUM NETWORK - BUPA Clinic DR. MOOPEN'S POLYCLINIC COMPREHENSIVE NETWORK Clinic DR. MOOPEN'S POLYCLINIC RESTRICTED NETWORK Clinic DR. -
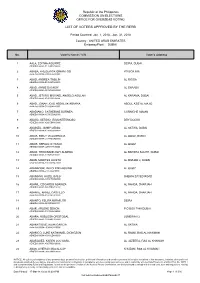
List of Voters Approved by the Rerb
Republic of the Philippines COMMISSION ON ELECTIONS OFFICE FOR OVERSEAS VOTING LIST OF VOTERS APPROVED BY THE RERB Period Covered: Jan. 1, 2018 - Jan. 31, 2018 Country : UNITED ARAB EMIRATES Embassy/Post : DUBAI No. Voter's Name / VIN Voter's Address 1 AALA, EDITHA AGUIRRE DEIRA, DUBAI AEAEDU-0000A-E1392EAA20000 2 ABABA, FREDERICK GIMANTOG PO BOX 686 AEAEDU-0000A-J1380FGA10000 3 ABAD, ANDREA TABILIN AL RIGGA AEAEDU-0000A-B0483ATA20000 4 ABAD, ANNIE DAANOY AL SHAABA AEAEDU-0000A-G0787ADA20000 5 ABAD, JETHRO MICHAEL ANGELO AGULAN AL KARAMA, DUBAI AEAEDU-0000A-K1493JAA10000 6 ABAD, JONAH JOJO HEERLIJK ABARRA ABDUL AZIZ AL MAJID AEAEDU-0000A-C0886JAA10000 7 ABADIANO, CATHERINE BORNEA CORNICHE AJMAN AEAEDU-0000A-K1790CBA20000 8 ABAGA, SERGIO JR MONTERMOSO DRY DOCKS AEAEDU-0000A-K2665SMA10000 9 ABAINZA, JIMMY GENIO AL SATWA, DUBAI AEAEDU-0000A-K2984JGA10000 10 ABAIS, EMILY VILLAGRACIA AL QOUZ, DUBAI AEAEDU-0000A-G1788EVA20000 11 ABAIS, SERGIO III YATOC AL QUOZ AEAEDU-0000A-J2587SYA10000 12 ABAIZ, FERDINAND ROY ALMEDA AL BARSHA SOUTH, DUBAI AEAEDU-0000A-I1192FAA10000 13 ABAN, MARITES HICETA AL MIZHAR 2, DUBAI AEAEDU-0000A-E0876MHA20000 14 ABANADOR, IAN GLENN AQUINO AL QUOZ AEAEDU-0000A-L1483IAA10000 15 ABANGAN, HAZEL BALO SHEIKH ZAYED ROAD AEAEDU-0000A-C2591HBA20000 16 ABANIL, EDGARDO ABAINZA AL NAHDA, SHARJAH AEAEDU-0000A-D0678EAA10000 17 ABANTE, ARNEL CASTILLO AL NAHDA, SHARJAH AEAEDU-0000A-K1479ACA10000 18 ABANTO, FELIPA MIRAFLOR DEIRA AEAEDU-0000A-I2049FMA20000 19 ABAR, ARLENE SENON P.O BOX 7880 DUBAI AEAEDU-0000A-E1075ASA20000 20 ABARA, -

SAADA Network List August 2018-Website.Xlsx
SAADA Network List Telephone City Type Name Address No Fax No DXB(04) Clinic Doctors Clinic ‐ DXB Al Maktoum Road 151 Sultan Owais, Deira, Dubai 2246688 2247181 DXB(04) Clinic Dr. Ismail Medical Centre ‐ DXB 1st Floor, Flat 12&13, A4 Sheikh Mohd Building, above West Hill Pharmcy 3378585 3349019 DXB(04) Hospital Cedar Jebel Ali International Hospital ‐ DXB Behind HSBC Bank,Dubai 8814000 8814001 DXB(04) Pharmacy Al Anber Pharmacy ‐ DXB Khalid Bin Al Walid Street 3973396 3973033 DXB(04) Pharmacy Al Woqaya Pharmacy ‐ DXB Karama Center, Box 27227 3348348 3360631 DXB(04) Pharmacy West Hill Pharmacy ‐ DXB Sheikh Mohd Building, 3377131 3344136 DXB(04) Clinic Dr. Maysoon Al Kaisi Clinic Hamarain Centre, Gate 4, Floor 3, Abu Baker Al Siddiq Road 2662044 2663611 DXB(04) Clinic Nasser Medical Consultant Centre ‐ DXB Hamarain Center, 2nd Floor, Entrance 4 2698400 2668636 DXB(04) Clinic New Apollo PolyClinic ‐ DXB Karama Center, near Lulu Supermarket 3379040 3346800 DXB(04) Clinic Al Mansoor Medical Center(ex.Dr. Arun Clinic)‐DXB Al Musalla Road 3554040 3596554 DXB(04) Pharmacy Union Pharmacy ‐ MEDSHOP ‐ DXB Rafa Police Station Road, Al Rafa Building, Burdubai 3935619 3935324 DXB(04) Clinic Naif Medical Centre ‐ DXB Naief Road, opposit Whitehouse Carpet 2716224 2711043 DXB(04) Dx & Lab Medinova Diagnostic Center Br. Al Futtaim Building, Al Fahidi Metro Station, Khalid Bin Waleed Road, Meena Bazaar, Bur Dubai, Dubai 5090327 3888650 DXB(04) Pharmacy Al Raha Pharmacy ‐ DXB Near to York International Hotel, Kalid Bin Al Walid Road, Burdubai 3523383 3515665 -

Aster Hospital
Restricted Network (RN) S.No Provider's Name Location & Phone Hospitals (Dubai) 1 Iranian Hospital Al Wasl Road, Jumeirah 1, Dubai-UAE 04-3440250 2 NMC Specialty Hospital Near Dubai Women's College, Ghussais, Dubai-UAE 04-2679999 3 Belhoul Speciality Hospital Deira, Dubai-UAE 04-2733333 4 NMC Hospital Dubai Salahuddin Road, New Al safyia Bldg, Deira, Dubai-UAE 04-2689800 5 Zulekha Hospital (Dubai) P.O.Box 48577, Dubai-UAE 04-2678866 6 Lifeline Hospital L.L.C Jebel Ali, Dubai-UAE 04-8845666 7 Aster Hospital (Aster Group) Aster Hospital Bldg, Al Rafa St., Mankhool Area, Burdubai 04-3814800 8 Cedars Jebel Ali International Hospital Jebel Ali Near freezone gate, # 2 Dubai, 04-8814000 9 NMC Hospital LLC, DIP Plot No. 5981220,Dubai Investments Park-1 ( DIP-1 Residential Zone ),Dubai 04-2372409 10 Medstar Health Care LLC Ground Floor,Gulf Tower,Beside DHCC,Oud Metha,Dubai (04 3577877) Hospitals (Abu Dhabi) 1 NMC Speciality Hospital LLC, Abu Dhabi Zayed 2nd street,samah tower / M1- flat 101 02-6332255 2 AL AHLI HOSPITAL COMPANY - WLL HAMDAN STREET, 1ST FLOOR OMEIR BIN YOUSEUF BUILDING 02-6228294 3 Lifecare Hospital LLC Gate No. 6, Workers Village 2, Baniyas West. Landmark: Al Madina Super Market, Abu Dhabi 02-586333 4 LLH Hospital LLC, Electra GOLDEN TOWER,ELECTRA STREET,ABU DHABI ,UAE 02-6335522 5 LLH Hospital Al Musaffah P.O BOX 92313, 16th Street, Musaffah - 1, Sanayya - 7 02-5557711 6 Medeor 24x7 Hospital (VPS Group) Opposite Empost, Muroor Street 02 6900600 7 Al Ruwais Hospital (Al Ruwais Hospital Group) Ruwais City -Abu Dhabi, UAE 02-6020575 8 Universal Hospital LLC-Abudhabi Behind Al Hilal Bank, Sheikh Rashid Bin Saeed Street, Old Airport Road, Abudhabi (02-6435555) Hospitals (Sharjah) 1 Enjab Hospital For Day Care 6th floor, Durrah Tower, Next to al ferdan Center, Sharjah-UAE 06-5563433 2 Sharjah Corniche Hopsital Corniche Plaza 2, 10th floor, Opp. -

Provider's Name Location & Phone Doctor's Name Doctor's Specialty
General Network (GN) Hospitals (Dubai) Provider's Name Location & Phone Doctor's Name Doctor's Specialty Canadian Specialist Hospital Abu Hail, Deira,Dubai-UAE Dr. Fatima Habes Epse Zairi General Practitioner 04-7072222 Dr. Emilia Kadour Internal Medicine Dr. Ahmed Badie Abdulmajeed Al Fikry Otorhinolaryngology Dr. Ethar Mohammed Abdulkader Abdulkader Radiology Dr. Sindhu Sony Raj Raveendran General Practitioner Dr. Hajira Najmi General Practitioner Dr. Shadia Thamir Obstetrics and Gynecology Dr. May Sidki Dental Dr. Naima Kulsoom Obstetrics and Gynecology Dr. Mehdi Shahriyari Afshar Interventional Cardiology Dr. Ali Reza Eghtedari General Surgery Dr. Chaaban Hassan General Practitioner Dr. Uzma Sabir Aleem Obstetrics and Gynecology Dr. Abduladeem M. Al Tamimi Radiology Dr. Seyed Mahmoodi Orthopedic Surgery Dr. Abdulameer Majeed Abu nailah Rheumatology Dr. Hayder Hussein Matouk Intensive Care Unit Dr. Fatemeh Fallahrajab Zadeh General Practitioner Dr. Noobi Moideen Koya Pediatrics Dr. Ibtisam Hussein Azeez Laboratory Dr. Shoaib Shahzad Khan Pediatrics Dr. Luma Musa Al Kurbasi Dental Dr. Sameem Majid Matto Internal Medicine Dr. Erum Khalil General Practitioner Dr. Mohammed Nooruldeen Jabbar Neurology Dr. Sunanda Arora Registrar Anesthesia Dr. Faisal Akbar General Practitioner Dr. Fidan Nadmi Obstetrics and Gynecology Dr. Ali Reza Shafizadeh General Practitioner Dr. Rola Ahmed Abuelnaaj General Practitioner Dr. Ardalan Ardeshir Papari Head of Department Dr. Kashif Malik Sana Ullah General Practitioner Dr. Nazish Ijaz General Practitioner Dr. Rehana Moin Obstetrics and Gynecology Dr. Mazin Abdul Hakeem Al Qaysi Anesthesia Dr. Abdelgadir mohamed Osman General Practitioner Dr. Muhammad Rizwan Husain General Practitioner Dr. Zahira Safeek General Practitioner Dr. Afrah Khalid Musa General Practitioner Dr.Paolo Cellocco SPECIALIST ORTHOPEDICS Dr. Nesreen Mahmoud Rfaa Pediatrics Dr. -

32 SMILE STONES DENTAL CARE CENTER LLC Address AMMAN
32 SMILE STONES DENTAL CARE CENTER LLC Address AMMAN STREET, AL NAHDA Region United Arab Emirates City/Emirate Dubai Telephone 04 2577211 FAX -- Network Green Specialties General Dentistry AALIYA MEDICAL CENTRE AJMAN-AALIYA HEALTH FOUNDATION Address AL SHAAB BLDG, 2 ndFLOOR,FLAT209 Region United Arab Emirates City/Emirate Ajman Telephone 7475599 FAX -- Network Green Specialties Dermatology, Radiology, General Dentistry, General Practice, Ophthalmology, Orthopedics, Pediatrics, Gynaecology & obestetric ABBARA POLY2 Address AL HAWAI BUILDING Region United Arab Emirates City/Emirate Dubai Telephone 04 2685333 FAX -- Network Green Specialties Gynaecology & obestetric, Urology ABDUL GHANI MEDICAL CENTRE-SHARJAH Address A-208/2, AL FARDAN CENTRE Region United Arab Emirates City/Emirate Sharjah Telephone 06-5562727 FAX -- Network Green Specialties ENT ABRAHAMS MEDICAL CENTRE-SHARJAH Address ROLLA TOWER BLDG, AL ZAHRA ST Region United Arab Emirates City/Emirate Sharjah Telephone 06 5612737 FAX -- Network Green Specialties General Dentistry, General Practice, Gynaecology & obestetric ABU SALMAN MEDICAL CENTRE - ABU DHABI / MF 1519 Address ABU SALMAN MEDICAL CENTRE Region United Arab Emirates City/Emirate Abu Dhabi Telephone 02 5522549 FAX -- Network Green Specialties General Practice ABU SHAGARA PHARMACY Address KING FAISAL STREET, AL RAWDAN BLDG Region United Arab Emirates City/Emirate Sharjah Telephone 5536414 FAX -- Network Green Specialties Pharmacy ACCESS CLINIC FREEZONE- JAFZA - DR. MOOPEN'S GRP Address Food court 3, 1st Floor, Next to commercial centre, Jabel Ali Free zone Region United Arab Emirates City/Emirate Dubai Telephone 04 8806577 FAX -- Network Green Specialties General Practice ACCESS CLINIC INTERNATIONAL CITY-DR.MOOPEN'S GROUP Address I -11 MORROCO CLUSTER, INTERNATIONAL CITY Region United Arab Emirates City/Emirate Dubai Telephone 04-3606587 FAX -- Network Green Specialties General Practice ACCESS CLINIC SONAPUR-DR. -

General Network Plus (GN +)
General Network Plus (GN +) S.No Provider's Name Location & Phone Emirates Contact No: Hospitals (Dubai) Oud Metha, Dubai-UAE 1 American Hospital Dubai 04-3367777 Abu Hail, Deira,Dubai-UAE 2 Canadian Specialist Hospital Dubai 04-7072222 Mediclinic Welcare Hospital L.L.C Abu Hail, Deira,Dubai-UAE 3 Dubai 04-2827788 (Mediclinic Group) Jumeirah, Opp. Jumeirah beach park, Dubai-UAE 4 Neuro Spinal Hospital Dubai 04-3420000 Mediclinic City Hospital FZ LLC (Mediclinic Dubai Healthcare City, Dubai-UAE 5 Dubai 04-4359999 Group) Jebel Ali, Dubai-UAE 6 Lifeline Hospital L.L.C Dubai 04-8845666 Near Dubai Women's College, Al Qusais, Dubai- 7 NMC Specialty Hospital UAE Dubai 04-2679999 Deira, Dubai-UAE 8 Belhoul Speciality Hospital Dubai 04-2733333 Dune Centre, Al diyafa street, satwa,dubai-UAE 9 Belhoul European Hospital Dubai 04 3454000 Al Razi Bldg #64, Dubai healthcare city, Dubai- Magrabi Eye Hopital-Outpatient surgery 10 UAE Dubai 04-4370606 center Opp. Al Safa PaRK, Gate 1, Jumeirah, Dubai-UAE 11 Medcare Hospital Dubai 04-4079100 Al Hamarain Center, 2nd floor, entrance 7 & 8, 12 Gulf Speciality Hospital Deira, Dubai-UAE Dubai 04-2699717 Sheikh Rashed Road, Mankhoul Area, Near Port 13 International Modern Hospital Rashed,Dubai-UAE Dubai 04-3988888 American Academy of Cosmetic Surgery DHCC, DISTRICT 1, Building 73, Dubai, UAE 14 Dubai 04-4237600 Hospital Salahuddin Road, New Al safyia Bldg, Deira, 15 NMC Hospital Dubai Dubai-UAE Dubai 04-2689800 P.O.Box 48577, Dubai-UAE 16 Zulekha Hospital (Dubai) Dubai 04-2678866 Jumeirah Beach road, opposite -

William Russell Comprehensive Network
WILLIAM RUSSELL COMPREHENSIVE NETWORK EMIRATES TYPE PROVIDER BUILDING ADDRESS STREET/AREA PO BOX SPECIALITIES PHONE FAX AUH (02) HOSPITAL AHALIA HOSPITAL COMPANY (LLC) AHALIA HOSPITAL BLDG, OPP BANK OF BARODA HAMDAN STREET 2419 MULTIPLE SPECIALITIES 626-2666 627-3871 AL MAZROUI HOSPITAL ONE DAY SURGERY AHMED KHALIFA KHALAF AL MAZROUI BLDG, STREET # 6, FLOOR AUH (02) HOSPITAL (FORMERLY KNOWN AS AL MAZROUI AL NAJDA STREET 54873 MULTIPLE SPECIALITIES 672-3232 672-3880 # 1, FLAT # 101 HOSPITAL) AUH (02) HOSPITAL AL NOOR HOSPITAL (AL NOOR GROUP) SHEIKH MOHD. BIN BUTTI BLDG KHALIFA STREET 46713 MULTIPLE SPECIALITIES 626-5265 626-6874 AL NOOR HOSPITAL AIRPORT ROAD (AL AUH (02) HOSPITAL NEAR KFC & ROCCO FORTE HOTEL, IN BETWEEN CARREFOUR AIRPORT ROAD 48481 MULTIPLE SPECIALITIES 444-6655 444-4199 NOOR GROUP) AL RAHA HOSPITAL (FORMERLY KNOWN AS AUH (02) HOSPITAL HYPERMAKET BLDG, FLOOR # 2 AL NAJDAH STREET 8119 MULTIPLE SPECIALITIES 633-0440 631-2601 GENERAL MEDICAL CENTRE HOSPITAL) AUH (02) HOSPITAL AL REEF INTERNATIONAL HOSPITAL SAIF TOWERS, FLOOR # 3 ELECTRA STREET 40407 MULTIPLE SPECIALITIES 632-8000 632-5577 AUH (02) HOSPITAL AL SALAMA HOSPITAL ABDULLA AL NIWAS BLDG, GROUND FLOOR HAMDAN STREET 46266 MULTIPLE SPECIALITIES 671-1220 671-1330 DAR AL SHIFA HOSPITAL BLDG, INTERSECTION OF DEFENCE AUH (02) HOSPITAL DAR AL SHIFA HOSPITAL AL NAJDAH STREET 2519 MULTIPLE SPECIALITIES 641-6999 641-6669 STREET EMIRATES FRENCH HOSPITAL LLC (FORMERLY AUH (02) HOSPITAL NADHA TOWER, GROUND FLOOR, FLAT # 2 CORNICHE ROAD 230 MULTIPLE SPECIALITIES 626-5722 626-5797