Prevalence and Associated Risk Factors of Peripheral Artery Disease In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kwara Annual School Census Report 2013
ANNUAL SCHOOL CENSUS REPORT 2013-2014 State Ministry of Education and Human Capital Development Kwara State School Census Report 2013-2014 Preface The Y2013/2014 Annual School Census exercise began with sensitization meetings with Public Schools Education Managers and Private Schools Proprietors, which was followed by the update of school list (with support from NGOs), clustering of schools and selection of supervisors/enumerators. The State EMIS Committee then met to deliberate on the modality for the conduct of the exercise. This was followed by the training of supervisors and enumerators, and distribution of questionnaires with the technical and financial support by ESSPIN. The success of the previous census was manifest in its wide acceptance and use in planning, budgeting, monitoring/evaluation within the MDAs and as source of reference by other users. This year exercise which was conducted between 24th February to 7th March began with data collection that was monitored by D/PRSs across the MDAs and ESSPIN Team. Completed forms were returned and screened for face and content validity. Forms with errors or incomplete data were returned for corrections. The data entry officers were trained in four LGA EMIS nodes, spread across the State, where data entry took place. Data cleansing and analysis took place at the State central EMIS in the State Ministry of Education and Human Capital Development. There was a great improvement in data quality and slight improvement in private schools participation as a result of the sensitization engagement with the stakeholders. The LGEA EMIS nodes were strengthened and grassroots commitment enhanced with the data entry that took place at the four centres. -

The Incidence of Microemboli to the Brain Is Less with Endarterectomy Than with Percutaneous Revascularization with Distal filters Or flow Reversal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector From the Southern Association for Vascular Surgery The incidence of microemboli to the brain is less with endarterectomy than with percutaneous revascularization with distal filters or flow reversal Naren Gupta, MD, PhD,a Matthew A. Corriere, MD, MS,a,c Thomas F. Dodson, MD,a Elliot L. Chaikof, MD, PhD,a Robert J. Beaulieu, BS,b James G. Reeves, MD,a Atef A. Salam, MD,a and Karthikeshwar Kasirajan, MD,a Atlanta, Ga Background: Current data suggest microembolization to the brain may result in long-term cognitive dysfunction despite the absence of immediate clinically obvious cerebrovascular events. We reviewed a series of patients treated electively with carotid endarterectomy (CEA), carotid artery stenting (CAS) with distal filters, and carotid stenting with flow reversal (FRS) monitored continuously with transcranial Doppler scan (TCD) during the procedure to detect microembolization rates. Methods: TCD insonation of the M1 segment of the middle cerebral artery was conducted during 42 procedures (15 CEA, 20 CAS, and 7 FRS) in 41 patients seen at an academic center. One patient had staged bilateral CEA. Ipsilateral microembolic signals (MESs) were divided into three phases: preprotection phase (until internal carotid artery [ICA] cross-shunted or clamped if no shunt was used, filter deployed, or flow reversal established), protection phase (until clamp/shunt was removed, filter removed, or antegrade flow re-established), and postprotection phase (after clamp/ shunt was removed, filter removed, or antegrade flow re-established). Descriptive statistics are reported as mean ؎ SE for continuous variables and N (%) for categorical variables. -

Superstitious Beliefs Held by the People of Ilorin, Kwara State, Nigeria
KIU Journal of Social Sciences KIU Journal of Social Sciences Copyright©2018 Kampala International University ISSN: 2413-9580; 4(1): 127–133 Superstitious Beliefs Held By the People of Ilorin, Kwara State, Nigeria MULKAH ADEBISI AHMED, ISAAC OLAKANMI ABIMBOLA, YAHAYA LUKMAN University of Ilorin, Nigeria BILIKIS ADENIKE ABDULSALAM Federal University of Technology, Minna, Nigeria Abstract. This study examined the scientific explanations and educational implications of 1. Introduction superstitious beliefs held by the people of Ilorin in Kwara State, Nigeria. A total number of 250 Taking a cursory look at the standard of living respondents were purposively sampled across and welfare of people globally, the impact of the three local government areas (LGAs) in science and technology cannot be over Ilorin metropolis, namely, Ilorin South, Ilorin emphasized. The attitude of humans towards West, and Ilorin East. The instrument used for nature manifests their traditional way of life and the study was research designed interview culture, which is prevalent in Africa. The protocol. The interview protocol was to find out traditional or common sense refers to one’s the superstitious beliefs held by the people of viewpoints, beliefs, attitudes, outlook, or ways Ilorin metropolis and to provide their scientific of life. For instance, in the traditional belief, the explanations. Four research questions were elders’ words are assumed to be words of raised and answered. The data collected were wisdom. Scientists (philosophers) use logical, subjected to frequency counts, percentages, and consistent, and systematic thinking in their chart presentation. The results showed that the efforts to reach sound conclusions about man, people of Ilorin South, Ilorin West, and Ilorin the world, and everything that exists—natural East held some superstitious beliefs about and supernatural. -

Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Hindawi Publishing Corporation International Journal of Vascular Medicine Volume 2016, Article ID 3805380, 6 pages http://dx.doi.org/10.1155/2016/3805380 Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry Kimihiro Igari, Toshifumi Kudo, Takahiro Toyofuku, and Yoshinori Inoue Division of Vascular and Endovascular Surgery, Department of Surgery, Tokyo Medical and Dental University, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8519, Japan Correspondence should be addressed to Kimihiro Igari; [email protected] Received 16 July 2016; Revised 17 September 2016; Accepted 27 September 2016 Academic Editor: Thomas Schmitz-Rixen Copyright © 2016 Kimihiro Igari et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objective. Endothelial dysfunction plays a key role in atherosclerotic disease. Several methods have been reported to be useful for evaluating the endothelial dysfunction, and we investigated the endothelial dysfunction in patients with peripheral arterial disease (PAD) using peripheral arterial tonometry (PAT) test in this study. Furthermore, we examined the factors significantly correlated with PAT test. Methods. We performed PAT tests in 67 patients with PAD. In addition, we recorded the patients’ demographics, including comorbidities, and hemodynamical status, such as ankle brachial pressure index (ABI). Results. In a univariate analysis, the ABI value ( = 0.271, = 0.029) and a history of cerebrovascular disease ( = 0.208, = 0.143) were found to significantly correlatewithPATtest,whichcalculatedthereactivehyperemiaindex(RHI).Inamultivariateanalysis,onlytheABIvalue significantly and independently correlated with RHI ( = 0.254, = 0.041). -

Impact of Climatic Change on Livelihood of Rural Dwellers in Kwara State
International Journal of Scientific & Engineering Research Volume 11, Issue 8, August-2020 1721 ISSN 2229-5518 IMPACT OF CLIMATIC CHANGE ON LIVELIHOOD OF RURAL DWELLERS IN KWARA STATE 1 2 2 1 Gana , N.N., Haruna , I.S., Ibrahim , M. D. and Igbokwe , G. O. Corresponding author: Gana, N. N. [email protected] 1, 2 Department of Physics Edu, Kwara State College of Education (Tech) Lafiagi 2Dept of Agric Educ, College of Education (Technical) Lafiagi, Kwara State 1 Department of Forestry and Fisheries, Usmanu Danfodiyo University, Sokoto Abstract Eight local government areas in Kwara State senatorial district being the areas that are prone to the effects of climate change were purposively selected. Proportionate sampling was employed to select the villages. A total of two thousand (2000) copies of the questionnaires were administered and one thousand four hundred and ninety-three returned. The data collected were subjected to descriptive statistical analysis (frequency and percentages) to analyze socio- economic characteristics of the farmers. The result indicated significant impact of climate change on livelihood such that 5.7% of people lost their lives due to flood, 18.3% of livestock were destroyed due to flood and 22.7% of the respondents agreed that livestock were destroyed due to harsh weather. 43.9% of the respondents also indicated that farm produce were invaded by birds (quelea), 40.8% showed that deforestation was the major cause of climate change, 25.1% agreed that over population was imminent in the selected LGA sampled. Key: Climate change,IJSER Livelihood, Impact, Rural dwellers, Kwara State INTRODUCTION In many developing countries there massive soil erosion and silting up of river are severe impacts of climate change. -

New York State Surgical and Invasive Procedure Protocol (NYSSIPP)
State of New York Department of Health Office of Health Systems Management Division of Primary and Acute Care Services New York State Surgical and Invasive Procedure Protocol for Hospitals ~ Diagnostic and Treatment Centers Ambulatory Surgery Centers ~ Individual Practitioners Antonia C. Novello, M.D., M.P.H., Dr.P.H. Commissioner of Health Hon. George E. Pataki Governor – State of New York September 2006 Surgical and Invasive Procedure Protocol September 2006 NEW YORK STATE SURGICAL AND INVASIVE PROCEDURE PROTOCOL (FOR THE PREVENTION OF WRONG PATIENT, WRONG SITE, WRONG SIDE & WRONG INVASIVE PROCEDURE EVENTS) I. STATEMENT OF PURPOSE The State of New York is committed to providing its residents access to quality health care. Hon. George E. Pataki, Governor and Antonia C. Novello M.D., M.P.H., Dr.P.H., Commissioner of Health, continue to work toward a system that reduces medical and surgical errors by commitment to a safe and protected patient care environment. Key to achieving this goal is promoting a culture of safety and strengthening open communication among health care providers, individual practitioners and the patients they serve. One of the goals of Governor Pataki and Commissioner Novello, is the elimination of wrong patient, wrong site, wrong side and wrong invasive procedures, through the development of comprehensive systems that ensure the correct procedure is done on the correct patient on the correct site. Increased practitioner awareness combined with strong provider protocols and standardization will enhance the patient safety measures currently in place. The New York State Surgical and Invasive Procedure Protocol (NYSSIPP) developed by the Procedural and Surgical Site Verification Panel (PSSVP) is intended for all patient care settings and for all individual practitioners. -
Fluorescein Angiography: Preventing and Responding to Complications
Fluorescein Angiography: Preventing and Responding to Complications Jacqueline G. Jaffee, J.D. OMIC Risk Management Specialist PURPOSE OF RISK MANAGEMENT RECOMMENDATIONS OMIC regularly analyzes its claims experience to determine loss prevention measures that our insured ophthalmologists can take to reduce the likelihood of professional liability lawsuits. OMIC policyholders are not required to implement these risk management recommendations. Use your professional judgment in determining the applicability of a given recommendation to their particular patients and practice situation. These loss prevention documents may refer to clinical care guidelines such as the American Academy of Ophthalmology’s Preferred Practice Patterns, peer-reviewed articles, or to federal or state laws and regulations. However, our risk management recommendations do not constitute the standard of care nor do they provide legal advice. If legal advice is desired or needed, consult an attorney. Information contained here is not intended to be a modification of the terms and conditions of the OMIC professional and limited office premises liability insurance policy. Please refer to the OMIC policy for these terms and conditions. Version 1/24/08 Fluorescein angiography (FA) is a diagnostic procedure in which a rapid sequence of photographs is taken to document the blood circulation of the retina/choroid. The dye is usually injected into a vein in the arm, forearm, or hand. While generally well tolerated, angiography is an invasive procedure with associated risks, very rarely but notably of a life-threatening allergic reaction. The following risk management recommendations have been compiled to assist you and your staff so that you may both prevent and better respond to the risks of the procedure. -

Anti-Apolipoprotein A-1 Igg Influences Neutrophil Extracellular Trap
International Journal of Molecular Sciences Article Anti-Apolipoprotein A-1 IgG Influences Neutrophil Extracellular Trap Content at Distinct Regions of Human Carotid Plaques Rafaela F. da Silva 1,2 , Daniela Baptista 1, Aline Roth 1, Kapka Miteva 1 , Fabienne Burger 1, Nicolas Vuilleumier 3,4, Federico Carbone 5,6 , Fabrizio Montecucco 5,6 , François Mach 1 and Karim J. Brandt 1,* 1 Division of Cardiology, Foundation for Medical Researches, Department of Medicine Specialties, Faculty of Medicine, University of Geneva, Av. de la Roseraie 64, 1211 Geneva, Switzerland; [email protected] (R.F.d.S.); [email protected] (D.B.); [email protected] (A.R.); [email protected] (K.M.); [email protected] (F.B.); [email protected] (F.M.) 2 Department of Physiology and Biophysics, Institute of Biological Sciences, Federal University of Minas Gerais, 31270-901 Belo Horizonte, Brazil 3 Department of Diagnostics, Division of Laboratory Medicine, Geneva University Hospitals, 1211 Geneva, Switzerland; [email protected] 4 Department of Medical Specialities, Division of Laboratory Medicine, Faculty of Medicine, 1211 Geneva, Switzerland 5 First Clinic of Internal Medicine, Department of Internal Medicine, University of Genoa, viale Benedetto XV n6, 16132 Genoa, Italy; [email protected] (F.C.); [email protected] (F.M.) 6 IRCCS Ospedale Policlinico San Martino Genoa-Italian Cardiovascular Network, Largo Rosanna Benzi n10, 16132 Genoa, Italy * Correspondence: [email protected]; Tel.: +41-2237-94-647 Received: 9 September 2020; Accepted: 13 October 2020; Published: 19 October 2020 Abstract: Background: Neutrophils accumulate in atherosclerotic plaques. Neutrophil extracellular traps (NET) were recently identified in experimental atherosclerosis and in complex human lesions. -

The Cardiopulmonary Bypass, Hemolysis, and End Organ Function: an Integration of Political Science, Chemistry, and Zoology
The Cardiopulmonary Bypass, Hemolysis, and end organ function: an Integration of Political Science, Chemistry, and Zoology By Nathan V. Luce A capstone project submitted to the faculty of Weber State University in fulfillment of the requirements of the degree of Bachelor of Integrated Studies in the Department of Integrated Studies. Ogden, Utah (Date Approved) Approved by: Department Director Dr. Michael Cena Ph.D. Committee Members: Political Science Dr. Gary Johnson Ph.D. Clinical and Clinical Research: Chemistry and Zoology Dr. Peter C. Minneci M.D. Marie Hart Clayton MSN, RN TABLE OF CONTENTS PREFACE......................................................................................................................................... v INTRODUCTION............................................................................................................................... 1 HISTORY AND BASICS: CARDIAC SURGERY AND THE CPB.................................................... 3 Evolution of Cardiac Surgery............................................................................................ 3 Intraoperative........................................................................................................... 5 Effects of Cardiopulmonary Bypass................................................................................. 6 Mechanical............................................................................................................... 6 Physiological: Whole Body Inflammatory Response............................................... -

1 1 0190004 Government Secondary School, Ilorin 1902 Tanke/Basin
NATIONAL EXAMINATIONS COUNCIL PMB 159, MINNA NIGER STATE SENIOR SCHOOL CERTIFICATE EXAMINATION (EXTERNAL) 2019 NOV/DEC SSCE LIST OF CENTRES AND CUSTODIAN POINTS KWARA STATE 019 S/n Neighbourhood Senatorial S/n Centre Code Name of Centre Neighbourhood Name Custodian Point L G A Per CP Code District 1. NECO OFFICE ILORIN 1 1 0190004 Government Secondary School, Ilorin 1902 Tanke/Basin NECO Office Ilorin Ilorin East Kwara Central 2 2 0190008 Government Day Secondary School, Tanke, Ilorin 1902 Tanke/Basin NECO Office Ilorin Ilorin South Kwara Central 3 3 0190085 Government Day Secondary School, Fate 1902 Tanke/Basin NECO Office Ilorin Ilorin South Kwara Central 4 4 0190013 Community Secondary School, Baboko, Ilorin 1904 Baboko/Sawmill NECO Office Ilorin Ilorin South Kwara Central 5 5 0190005 Army Day Secondary School, Sobi 1914 Gambari/Shao NECO Office Ilorin Ilorin South Kwara Central 6 6 0190015 Government High School, Ilorin 1915 Adeta/Oloje NECO Office Ilorin Ilorin East Kwara Central 8 8 0190032 Community Secondary School, Ogele 1916 Odota/Otte NECO Office Ilorin Ilorin East Kwara Central 9 9 0190078 Government Day Secondary School Airport, Ilorin 1916 Odota/Otte NECO Office Ilorin Ilorin East Kwara Central 10 10 0190116 Lasoju Comprehensive High School, Lasoju 1916 Odota/Otte NECO Office Ilorin Ilorin East Kwara Central 3. UNITY BANK OFFA 11 1 0190019 Ansarul-Deen College, Offa 1905 Offa/Oyun Unity Bank Offa Offa Kwara South 12 2 0190023 Erin-Ile Secondary School, Erin-Ile 1905 Offa/Oyun Unity Bank Offa Offa Kwara South 4. UNION BANK ORO 13 1 0190028 Jammat Nasir Islamic College, Oro 1906 Oro Union Bank Oro Irepodun Kwara South 5. -
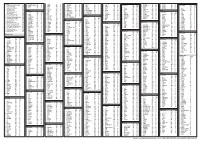
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Cervical Epidural Anaesthesia for Carotid Artery Surgery
353 Cervical epidural Francis Bonnet MD,* Jean Paul Derosier MD,'i" anaesthesia for carotid Frederic Pluskwa MD,* Kou Abhay MD,* A. Gaillard MDt artery surgery A series of 394 patients (251 men, 143 women; mean age 70.0 +- C2 d D4-D8 a ainsi dtd obtenu. Les patients sont restds dveillds 8.4 yr) selected for carotid artery" surgery, (CAS) performed pendant la durde de l'acte opdratoire dans des conditions de under cervical epidural anaesthesia (CEA ) was analysed retro- confort acceptables. Les complications sdrieuses rencontrdes spectively. Carotid endarterectomy was performed in 326 ont dtd la survenue d'une brdche duremdrienne dans deux cas, patients and saphenous vein bypass in 68. The cervical epidural d'une brdche vasculaire dans six cas et d'une insuffisance administration of 15 ml 0.5 per cent bupivacaine or 0.37-0.40 respiratoire chez trois patients. Hypotension (10,9 pour cent et per cent bupivacaine plus fentanyl (50-100 Izg) resulted in an bradycardie (2,8 pour cent) dtaient les effets secondaires les effective sensory blockade from C2 to T4-Ts. Patients were plus frdquemment observds. Un accident neurologique transi- maintained awake during the surgical procedure in comfortable toire s'est produit chez 84 patients pendant I'intervention condition. Serious complications included dural puncture in two chirugicale. Un accident neurologique irrdversible est survenu patients, epidural venipuncture in six patients and respiratory chez 12 patients. Trois infarctus du myocarde ont dtE diagnos- muscle paralysis in three patients. Hypotension (10.9 per cent) tiquds dans les suites opdratoires. La mortalitE de cette sdrie and bradycardia (2.8 per cent) were the most frequent side- Eta# de 2,3 pour cent.