Buxar District Health Action Plan 2010-2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Demp Kaimur (Bhabua)
DEMP KAIMUR (BHABUA) SL SUBJECT REMARKS NO. 1 2 3 1. DISTRICT BRIEF PROFILE DISTRICT POLITICAL MAP KEY STATISTICS BRIEF NOTES ON THE DISTRICT 2. POLLING STATIONS POLLING STATIONS LOCATIONS AND BREAK UP ACCORDING TO NO. OF PS AT PSL POLLING STATION OVERVIEW-ACCESSIBILITY POLLING STATION OVERVIEW-TELECOM CONNECTIVITY POLLING STATION OVERVIEW-BASIC MINIMUM FACILITIES POLLING STATION OVERVIEW-INFRASTRUCTURE VULNERABLES PS/ELECTIORS POLLING STATION LOCATION WISE ACCESSIBILITY & REACH DETAILS POLLING STATION WISE BASIC DETAISLS RPOFILING AND WORK TO BE DONE 3. MANPOWER PLAN CADRE WISE PERSONNEL AVAILABILITY FOR EACH CATEGORY VARIOUS TEAMS REQUIRED-EEM VARIOUS TEAMS REQUIRED-OTHERS POLLING PERSONNEL REQUIRED OTHER PERSONNEL REQUIRED PERSONNEL REQUIRED & AVAILABILITY 4. COMMUNICATION PLAN 5. POLLING STAFF WELFARE NODAL OFFICERS 6. BOOTH LIST 7. LIST OF SECTOR MAGISTRATE .! .! .! .! !. .! Assembly Constituency map State : BIHAR .! .! District : KAIMUR (BHABUA) AC Name : 205 - Bhabua 2 0 3 R a m g a r h MOHANIA R a m g a r h 9 .! ! 10 1 2 ! ! ! 5 12 ! ! 4 11 13 ! MANIHAR!I 7 RUP PUR 15 3 ! 14 ! ! 6 ! 8 73 16 ! ! ! RATWAR 19 76 ! 2 0 4 ! 18 .! 75 24 7774 17 ! M o h a n ii a (( S C )) ! ! ! 20 23 DUMRAITH ! ! 78 ! 83 66 21 !82 ! ! .! 32 67 DIHARA 22 ! ! 68 ! 30 80 ! 26 ! 31 79 ! ! ! ! 81 27 29 33 ! RUIYA 70 ! 25 ! 2 0 9 69 ! 2 0 9 KOHARI ! 28 KAITHI 86 ! K a r g a h a r 85 ! 87 72 K a r g a h a r ! ! 36 35 ! 71 60 ! ! ! 34 59 52 38 37 ! ! ! ! 53 KAIMUR (BHABUA) BHABUA (BL) 64 ! ! 40 84 88 62 55 MIRIA ! ! ! ! BAHUAN 54 ! 43 39 !89 124125 63 61 ! ! -

Brief Industrial Profile of Bhojpur District
Government of India Ministry of MSME Brief Industrial Profile of Bhojpur District Carried out by MSME -Development Institute (Ministry of MSME, Govt. of India,) Patliputra Industrial Estate, PATNA - 800013 Phone: 0612-2262186/2262208/2262719 Fax: 0612=2262186 e-mail: [email protected] Web-www.msmedipatna.gov.in 1 Contents S. No. Topic Page No. 1. General Characteristics of the District 03 1.1 Location & Geographical Area 03 1.2 Topography 03 1.3 Availability of Minerals. 03 1.4 Forest 04 1.5 Administrative set up 04 2. District at a glance 04 2.1 Existing Status of Industrial Area in the District Bhojpur 07 3. Industrial Scenario Of Bhojpur 07 3.1 Industry at a Glance 07 3.2 Year Wise Trend Of Units Registered 08 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The 09 District 3.4 Large Scale Industries / Public Sector undertakings 09 3.5 Major Exportable Item 09 3.6 Growth Trend 09 3.7 Vendorisation / Ancillarisation of the Industry 10 3.8 Medium Scale Enterprises 10 3.8.1 List of the units in Bhojpur & near by Area 10 3.8.2 Major Exportable Item 10 3.9 Service Enterprises 10 3.9.1 Coaching Industry == 3.9.2 Potentials areas for service industry 10 3.10 Potential for new MSMEs 10 4. Existing Clusters of Micro & Small Enterprise 10 4.1 Detail Of Major Clusters 10 4.1.1 Manufacturing Sector 10 4.1.2 Service Sector 11 4.2 Details of Identified cluster 11 5. General issues raised by industry association during the course of 12 meeting 6 Steps to set up MSMEs 13 2 Brief Industrial Profile of Bhojpur District 1. -

National Family Health Survey (Nfhs-5) India 2019-20 Bihar
NATIONAL FAMILY HEALTH SURVEY (NFHS-5) INDIA 2019-20 National Family Health 2019-20 Survey (NFHS-5) BIHAR MARCH 2021 Suggested citation: International Institute for Population Sciences (IIPS) and ICF. 2021. National Family Health Survey (NFHS-5), India, 2019-20: Bihar. Mumbai: IIPS. For additional information about the 2019-20 National Family Health Survey (NFHS-5), please contact: International Institute for Population Sciences, Govandi Station Road, Deonar, Mumbai-400088 Telephone: 022-4237 2442 Email: [email protected], [email protected] For related information, visit http://www.rchiips.org/nfhs or http://www.iipsindia.ac.in CONTRIBUTORS S.K. Singh Laxmi Kant Dwivedi Chander Shekhar Brajesh CONTENTS Page KEY FINDINGS Introduction .............................................................................................................................................. 1 Household Characteristics ...................................................................................................................... 3 Education ................................................................................................................................................... 6 Fertility ...................................................................................................................................................... 7 Family Planning ..................................................................................................................................... 10 Infant and Child Mortality ................................................................................................................... -

Report No.2 of 2019
Report of the Comptroller and Auditor General of India on Revenue Sector for the year ended 31 March 2018 Government of Bihar Report No. 2 of the year 2019 TABLE OF CONTENTS Paragraph Page Preface iii Overview v CHapter 1: General Trend of receipts 1.1 1 Analysis of arrears of revenue 1.2 7 Follow up on Audit Reports – summarised position 1.3 8 Response of the departments/Government to Audit 1.4 9 Internal Audit by Finance (Audit) Department 1.5 11 Results of audit 1.6 12 Coverage of this Report 1.7 12 CHapter 2: Commercial TAXes Tax administration 2.1 13 Results of audit 2.2 13 Audit on Implementation of transitional provisions of Goods 2.3 15 and Services Tax Act in Bihar Suppression of turnover 2.4 33 Short levy of tax due to application of incorrect rate of tax 2.5 34 Input Tax Credit 2.6 35 Short levy of tax due to incorrect adjustment of entry tax towards 2.7 37 payment of VAT Short levy of tax due to incorrect availing/claim of deduction 2.8 38 Short levy of tax on rental charges of electric meter 2.9 38 Non/short payment of admitted tax and interest 2.10 39 Non/short levy of entry tax 2.11 41 Short/non-payment of admitted entry tax and interest 2.12 41 Short levy of electricity duty 2.13 43 CHapter 3 : REVenUE anD LanD Reforms Tax administration 3.1 45 Results of audit 3.2 45 Non-remittance of establishment charges into the consolidated 3.3 45 fund of the State Non-realisation/remittance of revenue on alienation/transfer of 3.4 47 Government land Excess realisation of contingency charges 3.5 48 Table of Contents CHapter 4 : TAXes -

Bhojpur 2019-20
Ministry of Micro, Small & Medium Enterprises Government of India DISTRICT PROFILE BHOJPUR 2019-20 Carried out by MSME-Development Institute (Ministry of MSME, Govt. of India,) Patliputra Industrial Estate, Patna-13 Phone:- 0612-2262719, 2262208, 2263211 Fax: 06121 -2262186 e-mail: [email protected] Web- www.msmedipatna.gov.in Veer Kunwar Singh Memorial, Ara, Bhojpur Sun Temple, Tarari, Bhojpur 2 FOREWORD At the instance of the Development Commissioner, Micro, Small & Medium Enterprises, Government of India, New Delhi, District Industrial Profile containing basic information about the district of Bhojpur has been updated by MSME-DI, Patna under the Annual Plan 2019-20. It covers the information pertaining to the availability of resources, infrastructural support, existing status of industries, institutional support for MSMEs, etc. I am sure this District Industrial Profile would be highly beneficial for all the Stakeholders of MSMEs. It is full of academic essence and is expected to provide all kinds of relevant information about the District at a glance. This compilation aims to provide the user a comprehensive insight into the industrial scenario of the district. I would like to appreciate the relentless effort taken by Shri Ravi Kant, Assistant Director (EI) in preparing this informative District Industrial Profile right from the stage of data collection, compilation upto the final presentation. Any suggestion from the stakeholders for value addition in the report is welcome. Place: Patna Date: 31.03.2020 3 Brief Industrial Profile of Bhojpur District 1. General Characteristics of the District– Bhojpur district was carved out of erstwhile Shahbad district in 1992. The Kunwar Singh, the leader of the Mutineers during Sepoy Mutiny in 1857, was from district Bhojpur. -

Ground Water Arsenic Poisoning In
ntal & A me na n ly o t ir ic v a Kumar et al., J Environ Anal Toxicol 2015, 5:4 n l T E o Journal of f x o i l DOI: 10.4172/2161-0525.1000290 c o a n l o r g u y o J Environmental & Analytical Toxicology ISSN: 2161-0525 ResearchResearch Article Article OpenOpen Access Access Ground Water Arsenic Poisoning in “Tilak Rai Ka Hatta” Village of Buxar District, Bihar, India Causing Severe Health Hazards and Hormonal Imbalance Kumar A*, Ali Md, Rahman S Md, Iqubal A Md, Anand G, Niraj PK, Shankar P and Kumar R Mahavir Cancer Institute and Research Centre, Patna, Bihar, India Abstract In the recent times, arsenic poisoning due to contaminated ground water in the middle Gangetic plain has resulted to lots of health related problems in the population. In Bihar (India), about 16 districts have been reported to be affected with arsenic poisoning. In the present study, Tilak Rai Ka Hatta village, a flood plain Diara region of river Ganga in Buxar district was targeted for the ground water arsenic assessment and health related problems assessments among the village population. Altogether, 120 water samples were randomly collected for arsenic estimation and their results were statistically analysed. While for assessment of health related problems in the village people, 120 biological samples (blood) were collected from the same households. The study showed high contamination of arsenic in the ground water as three fourth region of the entire village had arsenic levels more than 100 ppb. The typical symptoms of hyperkeratosis in the palm and sole, melanosis of the skin in the village people were highly prevalent. -
Cbwtf/1838/2019
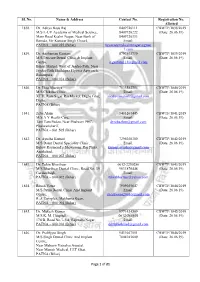
Sl. No. Name & Address Contact No. Registration No. Allotted 1838. Dr. Aditya Basu Raj 8409726111 CBWTF/1838/2019 M/S L-UV Academy of Medical Science, 8409726222 (Date: 26.06.19) Main Road Keshri Nagar, Near Bank of 8409726333 Baroda, Vir Kunwar Singh Chowk, Email: PATNA – 800 025 (Bihar) luvacademykeshrinagar@gmai l.com 1839. Dr. Anshuman Gautam 8797503739 CBWTF/1839/2019 M/S Pericare Dental Clinic & Implant Email: (Date: 26.06.19) Centre, [email protected] Bihari Market, West of Jagdeo Path, Near Jagdeo Path Sheikhpra Flyover Approach, Rukanpura, PATNA – 800 014 (Bihar) 1840. Dr. Ekta Bhartiya 7033582754 CBWTF/1840/2019 M/S Chikitsa Clinic, Email: (Date: 26.06.19) XTTI, Ram Sagar Rai Market, Digha Ghat, [email protected] Digha, PATNA (Bihar) 1841. Zeba Alam 9431267445 CBWTF/1841/2019 M/S A Y Health Care, Email: (Date: 26.06.19) Tam Tam Padao, Near Phulwari PHC, [email protected] Phulwarisharif, PATNA – 801 505 (Bihar) 1842. Dr. Ayusha Kumari 7295038300 CBWTF/1842/2019 M/S Daant Dental Speciality Clinic, Email: (Date: 26.06.19) Below Raymond’s Showroom, Raj Plaza, [email protected] Anishabad, PATNA – 800 002 (Bihar) 1843. Dr. Tuhin Bharthuar 0612-2250286 CBWTF/1843/2019 M/S Bharthuar Dental Clinic, Road No. 39, 9631876448 (Date: 26.06.19) Gardanibagh, Email: PATNA – 800 002 (Bihar) [email protected] 1844. Ritesh Vatsa 7909055647 CBWTF/1844/2019 M/S Patna Dental Clinic And Implant Email: (Date: 26.06.19) Centre, [email protected] R. J. Complex, Makhania Kuan, PATNA – 800 004 (Bihar) 1845. Dr. Mukesh Kumar 9771424509 CBWTF/1845/2019 M/S K. -

Bihar Power 13Th Plan BSPTCL & BGCL
83°30'0"E 84°0'0"E 84°30'0"E 85°0'0"E 85°30'0"E 86°0'0"E 86°30'0"E 87°0'0"E 87°30'0"E 88°0'0"E 27°30'0"N Surajpura Hydel P.S 27°30'0"N BIHAR MAP (Nepal) BHPC Valmikinagar (BSPTCL & BGCL WITH 13th PLAN) ± WEST CHAMPARAN Harinagar Sugar Mill Harinagar Narkatiaganj TSS Narkatiaganj Sugar Mill 132 kV Ramnagar (Parwanipur - Nepal) 27°0'0"N 33 kV 33kV Jaleshwar 27°0'0"N HPCL (Nepal) Raxaul (Birganj - Nepal) Lauriya TSS Raxaul Sugarmill Majhaulia NEPAL TSS Raxaul (New) Jivdhara TSS Dhanaha Bettiah Sugauli 33 KV Bettiah TSS Sugar Mill Dhaka Bairgania Biratnagar 132 KV TSS Duhabi Motihari SITAMARHI Pupri 33 KV EAST CHAMPARAN Rajbiraj Motihari Sitamarhi Sheohar Jainagar GOPALGANJ (DMTCL) Pakridayal Sitamarhi 26°30'0"N Hathua Areraj (New) MADHUBANI Kataiya 26°30'0"N SHEOHAR Bajpatti Laukahi TSS Benipatti Bharat Chakia Belsand Thakurganj Gopalganj Sugar Mill Mahwal Runnisaidpur TSS Madhubani Phulparas SUPAUL ARARIA Motipur Shiso TSS Pandaul UTTAR Maharajganj KISHANGANJ Kishanganj (PG) Siwan Ramdayalu Forbesganj TSS MTPS Raghopur Kishanganj SIWAN Gangwara Sakari TSS Pachrukhi Rajapatti SKMCH (New) PRADESH TSS Triveniganj TSS Darbhanga Nirmali Supaul Mashrakh Muzaarpur Mushahari Araria Darbhanga Jhanjharpur DLF MUZAFFARPUR Benipur Kishanganj 132/33 kV Marhowrah (Railway) MADHEPURA 26°0'0"N GSS Siwan Muzaarpur-PG Turki DARBHANGA TSS 26°0'0"N Madhepura SARAN Vaishali Saharsa Amnor-BGCL Shahpurpatori Darbhanga Saharsa Ekma Bela Rail Tajpur (DMTCL) (New) Factory Goraul Samastipur Kusheshwarsthan Banmankhi Purnea Chapra (New) Rosera Baisi Hajipur VAISHALI -

An Archaeological As Well As Social Anthropological Expedition at Bandha-II, Kaimur Range, Bihar
An Archaeological as well as Social Anthropological Expedition at Bandha-II, Kaimur Range, Bihar Sachin Kr. Tiwary1 1. Department of Ancient Indian History Culture and Archaeology, Faculty of Arts, Banaras Hindu University, Varanasi - 221005, Uttar Pradesh, India (Email: [email protected]) Received: 01 September 2016; Accepted: 30 September 2016; Revised: 28 October 2016 Heritage: Journal of Multidisciplinary Studies in Archaeology 4 (2016): 793-805 Abstract: The paper is based on the recent expedition on the border of Kaimur and Ghadhawa districts. While expedition author stayed at the village Bandha-II which is inhabited by the Kharwar tribe. Paper is specially focused on the rock art sites which are abundantly found near that village. The main purpose of the paper is to highlight the rich wealth of the rock art site on the left bank of river Son near Bandha-II. Meanwhile the paper is focusing the rituals and traditional games among the tribes on special occasion. Keywords: Bandha II, Kaimur Range, Archaeology, Anthropology, Expedition, Rock Art, Dance Introduction Between 7th-10th December of 2013 author explored the Bandha-II. The range of the Kaimur as well as the entire area of the south of the Middle Ganga seems to be in the state of terra-incognita that is seeking help of the massive efforts of archaeologists, historians, anthropologists, geologists and other relative discipline. And the present attempt to make an archaeological as well as social anthropological study (Tiwary 2013:1-16) of the Kaimurian (those tribes and live person who evolved and developed in this region only, also they did artistic work in the caves and shelter, which is still live) rock art reveals great potentialities in respect from the prehistoric times to the present times. -

Bihar Industrial Area Development Authority
-, BIHAR INDUSTRIAL AREA DEVELOPMENT AUTHORITY ----~-...--.,~-.- ,-- Minutes of the proceedings of meeting of the Project Clearence Committee (P.c.q held at Head office at Udyog Bhawan, Gandhi Maidan, Patna-800004 on Thrusday, 16th July, 2020 at 11.00 A.M (Application Received in June, 2020) Land Demanded Appl, Name of Area in Marks SI.No Proposed Unit & Address (in Sq. ft.)1 Remarks ID.No. Product Sq.ft. Obtained Plot No. & Area I 2 3 4 5 6 7 8 - MICRO Mis Enviro Tech Technologies, Producing ,nN Proprietor- Pankaj Kishor 14401 -e- Makhana POI)S, ::> GUilla, V-2 0 Making 0 Slo Sri Nawal Kishore Gupta, N Flavored/Roaste I ::>r-, At- Kali Bari Road. Mali Ghat, Bela Muzaffl,rpur 1440 82 Recommended d Makhana -< Muzaffarpur, Musahri, (11:) Q Snacks RTC District- Muzaffarpur (Bihar) ~ Kheer,l:Ially co 842001 Food etc. Mob-9709200338 a-. ..,on MIs Khushi Enterprises, 20001 0 0 Proprtetor-Binay Kumar.At- Shed B-3 0 N Daga Park, Pali Road, Dehri- On Cooler, Heater, 20001 0 2 N 4000 60 Recommended -e Sene District-Rohtas, Bihar- Motor etc Shed B-4 Q -e 821307 c: Mob-9304375158 Barun Rajeev Trade Comm Pvt. Ltd. ....Vi Director- 0 153561 0 Sri Shree Gopal Auto Pvt. Ltd. 0 Plot N0- C-2I N Maruti Suzuki Campus" N.H. 28 Fruit Juices and 3 0 15356 .-_---.. Not Recommended* N Danapur, Gopalganj, other Beverages -e Patliputa Qs District- Gopalganj, (Bihar) 0: Pin- 841428 Mob-9811652279 SMALL 0 'C -e MIs Mateshwari Rice Mill 0 <:> Proprietor- Manoj Kumar 50001 0 N Yadav, S/o Late Dadan Singh, 0-11 (P) 4 0 RiceM.i1l 5000 ------- Not Recommended* N-< Nandan, Durnrao, District- Q ::; Buxar Bihar -802119 Buxar 0: Mob-7748953333 Preference Plot- 1 Nirankari Enterprises, 14401 0..,.on Proprietor- Umesh Chaudhary, V-2 0 <:> Brijbihari Gall, Bela M uza ffa rpu r <:> N Laxmi Chowk, Snacks & (IE) s <:>... -

Hematological and Free Radicals Changes
of Publ al ic H rn e u a l Rahman et al., Int J Pub Health Safe 2019, 4:3 o t h J l a a n n d o i International Journal of S t a a f n e r t e y t n I Public Health & Safety Research Article Open Access Hematological and Free Radicals Changes among People of Arsenic Endemic Region of Buxar District of Bihar, India Rahman MS1, Kumar A2*, Kumar R2, Ali M2, Ghosh AK2 and Singh SK1 1Department of Biotechnology, Anugrah Narayan College, Patna, Bihar, India 2Department of Research, Mahavir Cancer Institute and Research Centre, Patna, Bihar, India Abstract Groundwater arsenic is developing as a major problem in floodplain of the Ganga. The large scale shift in the water resource allocation from surface water to groundwater in India exposed millions of people to the arsenic through groundwater. Arsenic induced toxicity in human blood cells has been evident from the several cases like Megaloblastic Dyserythropoietic Anemia, Pancytopenia. The present study is aims to know about the toxic effect of arsenic on human health by exploring blood arsenic concentration, some free radical assessment [Malondialdehyde (MDA), Glutathione Peroxidase (GPx)] and hematological parameters (RBC, Hb, HCT, MCV, MCH, MCHC and WBC) evaluation. The subjects belong from our recently explored arsenic hit area of Bihar. The result reveals maximum blood arsenic concentration as 706.1 μg/L while the mean blood arsenic concentration was 83.04 ± 10.60 μg/L in adult male and 70.47 ± 18.49 μg/L in adult female which was calculated corresponding to 228.105 ± 18.942 μg/L mean arsenic concentration in their drinking water. -

2019030915.Pdf
SN Applicati User ID Applied On Applicant Father's/ Date Of Gender Category Physicall Mobile No. Email ID Correspon Permanent Home Block Applied Is Matric Obt. Percen Inter Obt. Percen Graduation Obt. Percen on ID Name Husband's Birth (dd- y dence Address District District Finally Board/ Marks/ Full tage Board/ Marks/ Full tage Board/ Marks/ tage Name mm-yyyy) Handica Address Name Submit University- Marks University- Marks University- Full pped ted Passing Passing Passing Marks Year Year & Year & Specializati Specializati on on 4 EXA/232 5T2XBFCL 15-Sep-18 AAKID MD ALI 30-12-1990 Male EBC No 9709528145 majid9470 VILL- VILL- KATIHAR Katihar BUXAR N B.S.E.B 359/ 700 51.29 B.S.E.B 290/ 500 58 - 0 Spec.- 0/ 0 0 024303 HASAN HASAN 727182@g MAKHDUM MAKHDUM PATNA- PATNA- RAJA mail.com PUR P.O- PUR P.O- 2006 2009 Spec.- SIRNIA P.S- SIRNIA P.S- Science MUFASSIL MUFASSIL KATIHAR KATIHAR DIST- DIST- KATIHAR KATIHAR PIN - PIN - 854103 854103 75 EXA/232 KTFU58D2 15-Sep-18 ABHISHEK SUBHASH 19-04-2000 Male EBC No 7903946736 rajan.kuma S/O- SRI S/O- SRI PATNA PATNA BUXAR N C.B.S.E- 450/ 500 90 B.S.E.B- 257/ 500 51.4 - 0 Spec.- 0/ 0 0 023270 KUMAR KUMAR r4sinha199 SUBHASH SUBHASH SADAR 2016 2018 Spec.- [email protected] RAY RAY Science om RAGHUNAT RAGHUNAT H TOLA H TOLA ROAD NO. ROAD NO. 39 39 ANISABAD ANISABAD PATNA PATNA PIN - PIN - 99 EXA/232 2BRC4KGT 29-Aug-18 ABHISHEK LAL BABU 15-10-1991 Male EBC No 9608991292 Abhisheksh Vill+post-800002 Vill+post-800002 BHOJPUR Sahar BUXAR N BSEB 430/ 700 61.43 BSEB 551/ 900 61.22 V.K.S.U 538/ 67.25 000562 KUMAR SHARMA