Tana River County SMART Survey Report February 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Flash Update
Flash Update Kenya Floods Response Update – 29 June 2018 Humanitarian Situation and Needs Kenya Country Office An estimated 64,045 flood-affected people are still in camps in Galole, Tana Delta and Tana North Sub counties in Tana River County. A comprehensive assessment of the population still displaced in Tana River will be completed next week. Across the country, the heavy long rains season from March to May has displaced a total of 291,171 people. Rainfall continues in the Highlands west of the Rift Valley (Kitale, Kericho, Nandi, Eldoret, Kakamega), the Lake Basin (Kisumu, Kisii, Busia), parts of Central Rift Valley (Nakuru, Nyahururu), the border areas of Northwestern Kenya (Lokichoggio, Lokitaung), and the Coastal strip (Mombasa, Mtwapa, Malindi, Msabaha, Kilifi, Lamu). Humanitarian access by road is constrained due to insecurity along the Turkana-West Pokot border and due to poor roads conditions in Isiolo, Samburu, Makueni, Tana River, Kitui, and Garissa. As of 25 June 2018, a total of 5,470 cases of cholera with 78 deaths have been reported (Case Fatality Rate of 1.4 per cent). Currently, the outbreak is active in eight counties (Garissa, Tana River, Turkana, West Pokot, Meru, Mombasa, Kilifi and Isiolo counties) with 75 cases reported in the week ending 25 June. A total of 111 cases of Rift Valley Fever (RVF) have been reported with 14 death in three counties (Wajir 75, Marsabit 35 and Siaya 1). Case Fatality Rate is reported at 8 per cent in Wajir and 20 per cent in Marsabit. Active case finding, sample testing, ban of slaughter, quarantine, and community sensitization activities are ongoing. -

KENYA: FLOODS UPDATE NO.12 10 January 2007 This Information Bulletin (No
KENYA: FLOODS UPDATE NO.12 10 January 2007 This Information Bulletin (no. 12/2007) reflects the information available at this time. For further information specifically related to this operation please contact: • Abbas Gullet, Secretary General, Email: [email protected]. • Dr. Asha Mohamed, Deputy Secretary General, Email: [email protected] • Ahmed Abdi, Acting Head of Disaster Preparedness and Response, Email: [email protected] The Situation Rains continue in the country albeit with lower force than before. Most of the areas that were initially under water are now drying up even though the terrain remains muddy making some areas inaccessible using small vehicles. In the western parts of the country and parts of Rift Valley province however, people are still feeling the brunt of the heavy rains as rainfall continues heavily. The death toll according to media reports has now gone up to 142 (deaths by RVF not included) from the initial number of 114. Rift Valley Province In Tinderet Division, of Nandi South district, one child drowned while crossing Kigwal River. The search for the body is still going on. Landslides have also occurred affecting the squatter population of around 215 families living in a former forest land. Landslides caused destruction before in the years 1990, 1994, 1997 and 2006. Approximately 100 families are camping in Chebirer and Cherondo Primary schools. These schools do not have adequate sanitary facilities and enough rooms to accommodate the displaced families. Some of these people move to their homes during day only to come back to the centres at night in fear that it may rain again. -

Republic of Kenya Ministry of Environment and Mineral Resources
REPUBLIC OF\ KENYA MINISTRY OF ENVIRONMENT AND MINERAL RESOURCES i TANATANA RIVER RIVERDISTRICT DISTRICT ENVIRONMENTENVIRONMENT ACTION ACTION PLAN PLAN ACRONYMS 2009-2013 UNCED United Nations Conference2009 on Environment-2013 and Development NEAP National Environment Action Plan EMCA Environmental Management and Coordination Act ASAL Arid and Semi arid Lands GOK Government of Kenya NGO Non-Governmental Organization EIA Environmental Impact Assessment KWS Kenya Wildlife Services NEMA National Environment Management Authority ELSI Environment Liaison Center International TRPNR Tana River Primate National Reserve TRCC Tana River County Council EA Environmental Audit DEO District Environment Officer NEC National Environment Council KESSP Kenya Education Sector Support Program SEA Strategic Environment Assessment ILEG Institute for Law and Environmental Governance MOPND Ministry of Planning and National Development DLPO District Livestock Production Officer DPO District Planning Office KPLC Kenya Power and Lighting Company TARDA Tana and Athi River Development Authority MEA,s Multilateral Environmental Agreements CITES Convention on International Trade in Endangered Species of Flora and fauna DEAP District Environment Action Plan MOA Ministry of Agriculture WRMA Water Resources Management Authority CBO,s Community Based Organizations FUA Forest User Association FD Forest Department OOP Office of the President WUA Water User Association ii KENGEN Kenya Electricity Generating Company MOE Ministry of Energy NWC&PC National Water Conservation -

INSULT to INJURY the 2014 Lamu and Tana River Attacks and Kenya’S Abusive Response
INSULT TO INJURY The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response HUMAN RIGHTS WATCH hrw.org www.khrc.or.ke Insult to Injury The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response Copyright © 2015 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-6231-32446 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JUNE 2015 978-1-6231-32446 Insult to Injury The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response Map of Kenya and Coast Region ........................................................................................ i Summary ......................................................................................................................... 1 Recommendations .......................................................................................................... -
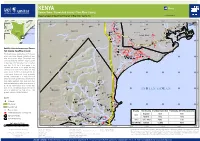
INDIAN OCEAN Yet Been Validated in the Field
KENYA AÆ Flood Garsen Town / Garsen Sub County / Tana River County Imagery analysis:4 May 2018 | Published 10 May 2018 | Version 1.0 FL20180508KEN ¥¦¬Juba 39°30'0"E 39°40'0"E 39°50'0"E 40°0'0"E 40°10'0"E 40°20'0"E 40°30'0"E 40°40'0"E 40°50'0"E 41°0'0"E Sailoni S Ziwa Shalu S " A " 0 Jipe 0 I ' ' 0 L Lamu East 0 1 1 ° Pate Island A Kulesa Hindi ° A 2 Sarbuye Simandaro 2 M Ziwa Gambi Mashundwani D O ¥¦¬ Wema Safarisi Bora Imani N S Mogadishu Pandanguo Kimari Maganga Kililana A Wama Kampala Hidiyo Mbwara Maganga G ¥¦¬ Hewani Mokowe U K E N YA Dumi Garsen Egge Ziwa Kiboko Masanga Kibirikani Nairobi Amu Tulu Koreni Lamu Map location Matondoni Kikomani ¥¦¬ Idsowe Takwa Milinga Ziwa Kambe ¥¦¬ Nkunumbi ShellaShela Milinga Lamu West KibirikaniKipungani MkonumbiaNdambwe Ndhambwe S S " Minjila Nyangoro " 0 0 ' ' 0 Maziwa Matatu 0 2 Kibusu 2 ° Kisibu ° 2 Mapenya 2 Pangani Witu Momba Sasa Kiongwe ¥¦¬ Ngao Ngau Mission Dida Waredi Satellite detected water over Garsen Mwanathumba Mandeni Golbanti MissionGolbanti Sub County, Tana River County Odd Borobini Tana River Furaka Kau S This map illustrates satellite-detected flood water S " " 0 Fitina 0 ' Kiko KoniOzi ' 0 Nduru Samicha 0 3 extent over Garsen, Magarini, Malindi and Lamu Chathuru 3 ° Ariti ° 2 Samikaro Anasa Maongo 2 Kalota West Sub Counties, Kenya. The analysis was Saidibabo Kipini conducted analyzing Sentinel-1 image acquired on the 4 May 2018. Within the extent of the map more than 25,000 ha of land appear to be inundated and around 20,000 people are living Karawa inside this flood water extent. -

Figure1: the Map of Kenya Showing 47 Counties (Colored) and 295 Sub-Counties (Numbered)
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Global Health Additional file 1: The county and sub counties of Kenya Figure1: The map of Kenya showing 47 counties (colored) and 295 sub-counties (numbered). The extents of major lakes and the Indian Ocean are shown in light blue. The names of the counties and sub- counties corresponding to the shown numbers below the maps. List of Counties (bold) and their respective sub county (numbered) as presented in Figure 1 1. Baringo county: Baringo Central [1], Baringo North [2], Baringo South [3], Eldama Ravine [4], Mogotio [5], Tiaty [6] 2. Bomet county: Bomet Central [7], Bomet East [8], Chepalungu [9], Konoin [10], Sotik [11] 3. Bungoma county: Bumula [12], Kabuchai [13], Kanduyi [14], Kimilili [15], Mt Elgon [16], Sirisia [17], Tongaren [18], Webuye East [19], Webuye West [20] 4. Busia county: Budalangi [21], Butula [22], Funyula [23], Matayos [24], Nambale [25], Teso North [26], Teso South [27] 5. Elgeyo Marakwet county: Keiyo North [28], Keiyo South [29], Marakwet East [30], Marakwet West [31] 6. Embu county: Manyatta [32], Mbeere North [33], Mbeere South [34], Runyenjes [35] Macharia PM, et al. BMJ Global Health 2020; 5:e003014. doi: 10.1136/bmjgh-2020-003014 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Global Health 7. Garissa: Balambala [36], Dadaab [37], Dujis [38], Fafi [39], Ijara [40], Lagdera [41] 8. -

Download Map (PDF | 3.82
KENYA AÆ Flood Garsen Town / Garsen Sub County / Tana River County Imagery analysis:4 May 2018 | Published 10 May 2018 | Version 1.0 FL20180504KEN ¥¦¬Juba 39°30'0"E 39°40'0"E 39°50'0"E 40°0'0"E 40°10'0"E 40°20'0"E 40°30'0"E 40°40'0"E 40°50'0"E 41°0'0"E Sailoni S Ziwa Shalu S " A " 0 Jipe 0 I ' ' 0 L Lamu East 0 1 1 ° Pate Island A Kulesa Hindi ° A 2 Sarbuye Simandaro 2 M Ziwa Gambi Mashundwani D O ¥¦¬ Wema Safarisi Bora Imani N S Mogadishu Pandanguo Kimari Maganga Kililana A Wama Kampala Hidiyo Mbwara Maganga G ¥¦¬ Hewani Mokowe U K E N YA Dumi Garsen Egge Ziwa Kiboko Masanga Kibirikani Nairobi Amu Tulu Koreni Lamu Map location Matondoni Kikomani ¥¦¬ Idsowe Takwa Milinga Ziwa Kambe ¥¦¬ Nkunumbi ShellaShela Milinga Lamu West KibirikaniKipungani MkonumbiaNdambwe Ndhambwe S S " Minjila Nyangoro " 0 0 ' ' 0 Maziwa Matatu 0 2 Kibusu 2 ° Kisibu ° 2 Mapenya 2 Pangani Witu Momba Sasa Kiongwe ¥¦¬ Ngao Ngau Mission Dida Waredi Satellite detected water over Garsen Mwanathumba Mandeni Golbanti MissionGolbanti Sub County, Tana River County Odd Borobini Tana River Furaka Kau S This map illustrates satellite-detected flood water S " " 0 Fitina 0 ' Kiko KoniOzi ' 0 Nduru Samicha 0 3 extent over Garsen, Magarini, Malindi and Lamu Chathuru 3 ° Ariti ° 2 Samikaro Anasa Maongo 2 Kalota West Sub Counties, Kenya. The analysis was Saidibabo Kipini conducted analyzing Sentinel-1 image acquired on the 4 May 2018. Within the extent of the map more than 25,000 ha of land appear to be inundated and around 20,000 people are living Karawa inside this flood water extent. -

TANA RIVER SECONDARY DATA REVIEW AS at FEBRUARY 2014 Introduction Summary
TANA RIVER SECONDARY DATA REVIEW AS AT Tana River County constitutes 0.6% of the national population FEBRUARY 2014 ranked 44/47. 49.9% of the population are male while 50.1% are female Table 1 Introduction The county shares 15.0% of the national urban population ranked 33/47 CRA 2011 This document is a baseline for humanitarian needs assessment in Hola town is the largest urban population taking 7.2% of the Tana River with an aim to provide information that would aid in county’s population, Madogo 6.7% and Garsen 1.2%1 decision making. The information presented has been gathered It has a population density of 383.5 which is lower than the through a review of pre-crisis secondary data, studies and lessons national population density of 401.1 per square kilometer, with 6.2 learnt reports. Available indicator information is by Sub County, people in every km 2 see Table 1 county and national (where there is no available sub-county/county The rate of poverty (adult equivalent poverty head count) is 76.9% information). This desk review is to help in the process of higher than the national rate of 45.9% and its ranked 43/472 assessment planning for humanitarian needs assessment. The average household size in Tana River is 5.06, 0.6 higher than the national household size of 4.4. Table 1. Purpose of the Desk review The county’s age distribution is 50.9% between 0-14 years, 46.2% (15–64 yrs) and 2.9% are above 65 years old CRA 2011 This desk review is not a comprehensive survey on food security, 20.04% of the population is under the age of 5 years and 37.54% livelihoods, WASH, protection e.t.c nor is it an inter-agency needs are between the ages of 0-9 years3 assessment. -

MSF-Spain Final Floods Report.Pdf
Response To Flood Emergency 2013 A MSF Spain Acknowledgement MSF Spain appreciates the financial support provided by ECHO in assisting the flood affected population in 1 Kenya during the long rain season in 2013. It is with their support that MSF Spain was able to assist over 25,000 people with health care services , shelter material, non food items and water and sanitation. Gabriel Sanchez, Head of Mission, MSF Spain Disclaimer: The views and opinions expressed in this report are from MSF Spain and do not reflect the position of any other actors during the floods intervention. The information given in the report is based on the experience of MSF Spain during the floods intervention in the period April to May 2013. Response To Flood Emergency 2013 B MSF Spain TABLE OF CONTENTS Summary 2 1 Background 3 2 Area of Intervention 3 2.1 Bura 3 2.2 Garsen 4 2.3 Lamu West 4 2.4 Gilgil 4 2.5 Garissa 5 2.6 Narok 5 2.7 Isiolo 5 3 Intervention Strategy 6 3.1 Tana River area: Bura, Garsen, and Lamu West 7 3.2 Garissa 7 3.3 Narok and Gilgil 7 3.4 Isiolo 7 4 Intervention results 8 4.1 Result 1 8 ¨The flood affected population has an increased access to health care while surveillance of notifiable diseases is reinforced.¨ 4.1.1 Beneficiaries of medical services 8 4.1.2 Surveillance 9 4.1.3 Consultations 10 4.1.4 Morbidity 11 4.1.5 Maternal child health services in Bura and Garsen 13 4.1.6 Referrals 14 4.2 Result 2 “The displaced population has access to shelter material and non-food items.” 14 4.2.1 NFI distribution 15 4.2.2 IEC Sessions 15 4.3 Result 3 “The displaced population has access to a minimum standard of drinking water and temporary sanitation facilities.” 16 4.3.1 Latrines 16 4.3.2 Aqua tablets 18 5 Challenges 19 6 Conclusions - Recommendations 20 Response To Flood Emergency 2013 1 MSF Spain Summary Floods in Kenya are relatively common during the short and the long rains. -
Hanshak Nyongoro
HANSHAK-NYONGORO COMMUNITY CONSERVANCY MANAGEMENT AND COMMUNITY DEVELOPMENT PLAN (2016 - 2020) 1 HANSHAK-NYONGORO COMMUNITY CONSERVANCY 1 2 INTRODUCTION This Conservancy Management and Community Development Plan has been developed by Hanshak-Nyongoro Community Conservancy with support from the Northern Rangelands Trust. The plan was developed through a participatory process led by the Conservancy Board. The process included the following steps: Background information– including reference to previous reports, baseline statistics on human livelihoods. Mapping – participatory and field mapping of key features across the conservancy, development of a conservancy map to visualize the current status and future vision for the conservancy. Board brainstorming session – to identify the main challenges and long term priorities for the conservancy, and identify key partners and stakeholders for inclusion in the planning process. Consultation with community and key partners – meetings with community, government and partner organization representatives in all zones of the conservancy, to discuss and develop the goals and objectives. Draft plan– a draft plan was developed and circulated to Conservancy Management for discussion with the Board to ensure it accurately captured discussions and priorities from community and stakeholder meetings. Final plan – presented to the AGM for endorsement, publication and dissemination of the plan to partners. The purpose of this plan is to capture the holistic, long-term vision for community development and conservation success of our Conservancy. It is a tool to: Guide the conservancy management in their activities, ensuring they focus on priorities that have been determined by the wider community, conservancy staff and Boards. Provide continuity of management and hold managers and Boards to account by their members. -

Environmental Sensitivity Atlas of Lamu County
Environmental Sensitivity Atlas of Lamu County © This Atlas has been prepared with support from NORAD and WWF-Kenya FOREWORD proposed development initiatives such as an oil refinery, a coal powered plant and modern city area, by the government will have far reaching consequences Ecosystems in Lamu County are under enormous if proper strategic environmental assessments are not done. The Atlas presents pressure from increasing human population. The information in map and pictorial form to draw the attention of decision-makers population is extracting and using resources at an to existing environmental hotspots and anticipated human impacts that may lead accelerated rate from a resource base that is vulnerable to environmental degradation and therefore loss of environmental resources. The and finite. The pressure on the natural resources is Atlas also documents the location and extent of current environmental resources manifested in vegetation removal; land and water such as the coral reefs, sand dunes, mangroves, coastal forest and cultural resources degradation and pollution; overfishing and heritages whose conservation value has attracted both local and international degradation of fish habitats; competition for use of sentimental concern. aquatic space; and changes in atmospheric processes, such as climate change and its consequences. Lamu County’s environmental resources including rare marine biodiversity such as corals, dugongs and sea turtles which is what lead to the establishment of Kiunga Environmental resources are important to Kenya’s Marine National Reserve. The sheltered bays have deep waters leading to the socio-economic development. They support wealth proposal to develop the Lamu Port part of the LAPSSET Project. The discovery of creation, ensure food security and maintain a safe and clean environment. -

Tana River Garissa Lamu
KENYA AÆ Flood Tana River, Galole & Garsen Sub Counties Imagery analysis: 4 May 2018 | Published 11 May 2018 | Version 1.0 FL20180508KEN 39°55'0"E 40°0'0"E 40°5'0"E 40°10'0"E 40°15'0"E E T H I O P I A Ghalamani Fafi S S " A " 0 Chewani 0 ' ' D A 5 5 2 I Mwogahendi 2 ° ° N 1 Malindi 1 L A A Wacha Koni G M U Ngwena Fafi O ¥¦¬ S K E N YA Nairobi Balguda ¥¦¬ GaloleHola Pendeza S S " Laza " 0 0 ' Map location ' 0 Koni 0 3 3 ° ° 1 1 Galole Analysis Extent Mikinduni Dodoma ~ 6,800 ha inundated Chenani ¥¦¬ ~4,300 people potentially affected Lenda S S " Satellite detected water along " 0 0 ' ' 5 Handampia 5 3 3 ° Tana River, Galole & Garsen sub ° 1 1 counties, TanaRiver county, Pumwani Kenya Mkomaniboi This map illustrates satellite-detected flood Galole Mazuni water extent along Tana River, Galole and Garsen sub counties, Tana River county, S S " " 0 0 Kenya. The analysis was conducted by ' Fanjua ' 0 Garissa 0 4 4 ° ° 1 analyzing Sentinel-1 imagery acquired on the 1 Majengo 4 May 2018. The analysis extent is focused Ijara on the river bed of Tana, the surrounding MassalaniWalu land between the primary road and the limit of the Tana River boundary, specifically Gubani where the population is concentrated. Within Kanjonja S S " the analysis extent, around 22,700 ha of land " 0 0 ' ' 5 5 4 4 ° appears to be inundated and more than ° 1 1 21,600 people are living inside this flood water extent.