Recommendation for Accreditation of Obsterical
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Product List March 2019 - Page 1 of 53
Wessex has been sourcing and supplying active substances to medicine manufacturers since its incorporation in 1994. We supply from known, trusted partners working to full cGMP and with full regulatory support. Please contact us for details of the following products. Product CAS No. ( R)-2-Methyl-CBS-oxazaborolidine 112022-83-0 (-) (1R) Menthyl Chloroformate 14602-86-9 (+)-Sotalol Hydrochloride 959-24-0 (2R)-2-[(4-Ethyl-2, 3-dioxopiperazinyl) carbonylamino]-2-phenylacetic 63422-71-9 acid (2R)-2-[(4-Ethyl-2-3-dioxopiperazinyl) carbonylamino]-2-(4- 62893-24-7 hydroxyphenyl) acetic acid (r)-(+)-α-Lipoic Acid 1200-22-2 (S)-1-(2-Chloroacetyl) pyrrolidine-2-carbonitrile 207557-35-5 1,1'-Carbonyl diimidazole 530-62-1 1,3-Cyclohexanedione 504-02-9 1-[2-amino-1-(4-methoxyphenyl) ethyl] cyclohexanol acetate 839705-03-2 1-[2-Amino-1-(4-methoxyphenyl) ethyl] cyclohexanol Hydrochloride 130198-05-9 1-[Cyano-(4-methoxyphenyl) methyl] cyclohexanol 93413-76-4 1-Chloroethyl-4-nitrophenyl carbonate 101623-69-2 2-(2-Aminothiazol-4-yl) acetic acid Hydrochloride 66659-20-9 2-(4-Nitrophenyl)ethanamine Hydrochloride 29968-78-3 2,4 Dichlorobenzyl Alcohol (2,4 DCBA) 1777-82-8 2,6-Dichlorophenol 87-65-0 2.6 Diamino Pyridine 136-40-3 2-Aminoheptane Sulfate 6411-75-2 2-Ethylhexanoyl Chloride 760-67-8 2-Ethylhexyl Chloroformate 24468-13-1 2-Isopropyl-4-(N-methylaminomethyl) thiazole Hydrochloride 908591-25-3 4,4,4-Trifluoro-1-(4-methylphenyl)-1,3-butane dione 720-94-5 4,5,6,7-Tetrahydrothieno[3,2,c] pyridine Hydrochloride 28783-41-7 4-Chloro-N-methyl-piperidine 5570-77-4 -

Endogenous Opioid Analgesia in Peripheral Tissues and the Clinical Implications for Pain Control
REVIEW Endogenous opioid analgesia in peripheral tissues and the clinical implications for pain control Daniel Kapitzke1,2 Abstract: Opioid receptors are widely expressed in the central and peripheral nervous system Irina Vetter1,2 as well as in numerous nonneuronal tissues. Both animal models and human clinical data Peter J Cabot2 support the involvement of peripheral opioid receptors in analgesia, particularly in inflammation where both opioid receptor expression and efficacy are increased. Immune cells have been 1 These authors contributed equally β to this work. 2School of Pharmacy, shown to contain numerous opioid peptides such as -endorphin (END), met-enkephalin University of Queensland, 4072, (ENK), and dynorphin-A (DYN), although the predominant opioid peptide involved in immune- Australia cell mediated antinociception is thought to be END. These opioid-containing immune cells migrate to inflamed tissues during a complex process of recruitment by chemokines, adhesion, and extravasation. In these tissues, opioid peptide is released from the immune cells upon stimulation with corticotrophin-releasing factor (CRF), noradrenaline, and interleukin 1β (IL-1β), and the immune cells return to the local lymph node depleted of peptide. Consistent with this model, systemic immunosuppression may lead to impaired endogenous analgesia as competent immune cells are essential to achieve release of endogenous opioid peptides within inflamed tissue. A further level of complexity is added by the observation that exogenous opioids may impair immune cell function, although there is some evidence to suggest that endogenous opioid peptides do not share this immunosuppressive effect. Improving our understanding of endogenous opioid mechanisms will provide valuable insight towards the development of novel treatments for pain with improved side effect profiles. -

Download Drug Labels List
Syringe Labelling System Price Per Label Description/Drug Name Item No. Quanitiy Per Pack Pack Abciximab 99801 2 x 500 roll's £6.30 Abidec 100602 2 x 500 roll's £6.30 Acepromazine 99802 2 x 500 roll's £6.30 Acetazolamide 99803 2 x 500 roll's £6.30 Acetylcholine 99804 2 x 500 roll's £6.30 Acetylcysteine 99805 2 x 500 roll's £6.30 Acetylsalicylic Acid 99806 2 x 500 roll's £6.30 Aciclovir 99807 2 x 500 roll's £6.30 ACP/Buprenorphine 100208 2 x 500 roll's £6.30 Actrapid Insulin 99808 2 x 500 roll's £6.30 Adenosine 99809 2 x 500 roll's £6.30 Adrenaline (Top Half Black, Bottom Violet, Violet Text) 99810 2 x 500 roll's £6.30 Adrenaline/Epinephrine 99811 2 x 500 roll's £6.30 Albumin Solution 99812 2 x 500 roll's £6.30 Alchol 99813 2 x 500 roll's £6.30 Alemtuzmab 99814 2 x 500 roll's £6.30 ALERT 100243 2 x 500 roll's £6.30 Alfaxalone 99815 2 x 500 roll's £6.30 Alfentanil 99816 2 x 500 roll's £6.30 Alfentanil 99817 2 x 500 roll's £6.30 Alteplase 99818 2 x 500 roll's £6.30 Amikacin 99819 2 x 500 roll's £6.30 Aminophylline 99820 2 x 500 roll's £6.30 Amiodarone 100194 2 x 500 roll's £6.30 Amoxicillin 100195 2 x 500 roll's £6.30 Amphotericin 99821 2 x 500 roll's £6.30 Ampicillin 99822 2 x 500 roll's £6.30 Antibiotic 99823 2 x 500 roll's £6.30 Anticoagulant 99824 2 x 500 roll's £6.30 Antifungal 100228 2 x 500 roll's £6.30 Antiseptic 99825 2 x 500 roll's £6.30 Aprotinin 99826 2 x 500 roll's £6.30 Aqueous Iodine 99827 2 x 500 roll's £6.30 Arterial 100259 2 x 500 roll's £6.30 Arterial ( Line Label - White with Red Writing) 100176 2 x 500 roll's £6.30 Arterial -

Sale Catalog
Hoffman Manufacturing Page: 2 Controlled Environment Chambers, Seed Testing Equipment and Lab Supplies DW-86L578J DW-86L338J Read More Read More SKU: N/A SKU: N/A Price: $16,995.00 Price: $15,790.00 $12,995.00 $12,500.00 Categories: Refrigerators Categories: Refrigerators and Freezers, Vaccine and Freezers, Vaccine Storage Storage Tags: -86, Cold Storage, Tags: -86, Cold Storage, freezer, Haier, Pharmacy freezer, Haier, Pharmacy Freezer, Ultra Low, vaccine, Freezer, Ultra Low, vaccine, vaccine storage vaccine storage SHEL LAB SVAC2 SHEL LAB SVAC2 DIGITAL VACUUM OVEN, DIGITAL VACUUM OVEN, 1.67 CU. FT. (47.2 L), 1.67 CU. FT. (47.2 L), 115V - SVAC2-2 115V - SVAC2 Model: SVAC2-2 Model: SVAC2 Read More Read More SKU: N/A SKU: N/A Price: $6,945.00 $5,900.00 Price: $6,314.00 $5,400.00 Hoffman Manufacturing Page: 3 Controlled Environment Chambers, Seed Testing Equipment and Lab Supplies SHEL LAB® SVAC4 SHEL LAB® SVAC4 DIGITAL VACUUM OVEN, DIGITAL VACUUM OVEN, 4.5 CU. FT. (127.4 L), 4.5 CU. FT. (127.4 L), 115V - SVAC4 115V - SVAC4-2 Model: SVAC4 Model: SVAC4-2 Read More Read More SKU: SVAC4 SKU: SVAC4 Price: $12,214.00 Price: $13,435.00 $10,400.00 $11,000.00 SHEL LAB® SCO6WE SHEL LAB® SMI6 CO2 WATER JACKETED MICROBIOLOGICAL INCUBATOR, 6.0 CU.FT. INCUBATOR, 5.9 CU.FT. (171 L), 115V - (166 L), 110-120V - SCO6WE-2 SMI6-2 230V Voltage: SCO6WE-2 Model: SMI6-2 230V Read More Read More SKU: SHC10 SKU: INC SM16 Price: $6,831.00 $5,508.00 Price: $3,516.00 $3,300.00 Hoffman Manufacturing Page: 4 Controlled Environment Chambers, Seed Testing Equipment and Lab Supplies SHEL LAB® SMI6 SG22 SINGLE CHAMBER MICROBIOLOGICAL INCUBATOR, 5.9 CU.FT. -

A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Clifford Gevirtz
The Role of Anesthesiology in Global Health A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Cli ord Gevirtz Editors Carrie L.H. Atcheson Associate Editor 123 The Role of Anesthesiology in Global Health Ram Roth • Elizabeth A.M. Frost Clifford Gevirtz Editors Carrie L.H. Atcheson Associate Editor The Role of Anesthesiology in Global Health A Comprehensive Guide Editors Ram Roth Elizabeth A.M. Frost Department of Anesthesiology Department of Anesthesiology Icahn School of Medicine at Mount Sinai Icahn School of Medicine at Mount Sinai New York , NY , USA New York , NY , USA Clifford Gevirtz Department of Anesthesiology LSU Health Sciences Center New Orleans , LA , USA Associate Editor Carrie L.H. Atcheson Oregon Anesthesiology Group Department of Anesthesiology Adventist Medical Center Portland , OR , USA ISBN 978-3-319-09422-9 ISBN 978-3-319-09423-6 (eBook) DOI 10.1007/978-3-319-09423-6 Springer Cham Heidelberg New York Dordrecht London Library of Congress Control Number: 2014956567 © Springer International Publishing Switzerland 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -
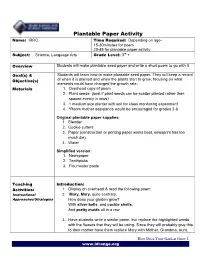
Plantable Seed Paper and Write a Short Poem to Go with It
Plantable Paper Activity Name: IRRC Time Required: Depending on age- 15-30minutes for poem 20-45 for plantable paper activity Subject: Science, Language Arts Grade Level: 3rd + Overview Students will make plantable seed paper and write a short poem to go with it. Goal(s) & Students will learn how to make plantable seed paper. They will keep a record of when it is planted and when the plants start to grow; focusing on what Objective(s) elements could have changed the growth rate. Materials 1. Overhead copy of poem 2. Plant seeds- (best if plant seeds can be scatter planted rather than spaced evenly in rows) 3. 1 medium size planter with soil for class monitoring experiment 4. *Room mother assistance would be encouraged for grades 3-6 Original plantable paper supplies: 1. Blender 2. Cookie cutters 3. Paper (construction or printing paper works best, newsprint has too much die) 4. Water Simplified version: 1. Newspaper 2. Toothpicks 3. Flour/water paste Teaching Introduction: Activities: 1. Display on overhead & read the following poem: Instructional 2. Mary, Mary, quite contrary, Approaches/Strategies How does your garden grow? With silver bells, and cockle shells, And pretty maids all in a row 3. Have students write a similar poem, but replace the highlighted words with the flowers that they will be using- Since they will probably give this to their mother have them replace Mary with Mother, Grandma, Aunt, How Does Your Garden Grow 1 www.idrange.org etc. ex: Mother, Mother quite contrary How does your garden grow? With wildflowers and cosmos, And pretty marigolds all in a row. -

Low Doses of A2-Adrenoceptor Antagonists Augment Spinal Morphine Analgesia and Inhibit Development of Acute and Chronic Tolerance
British Journal of Pharmacology (2008) 155, 1264–1278 & 2008 Macmillan Publishers Limited All rights reserved 0007– 1188/08 $32.00 www.brjpharmacol.org RESEARCH PAPER Low doses of a2-adrenoceptor antagonists augment spinal morphine analgesia and inhibit development of acute and chronic tolerance B Milne, M Sutak, CM Cahill and K Jhamandas Department of Pharmacology and Toxicology, and Department of Anesthesiology, Queen’s University, Kingston, Ontario, Canada Background and purpose: Ultra-low doses of opioid receptor antagonists augment spinal morphine antinociception and block the induction of tolerance. Considering the evidence demonstrating functional and physical interactions between the opioid and a2-adrenoceptors, this study investigated whether ultra-low doses of a2-adrenoceptor antagonists also influence spinal morphine analgesia and tolerance. Experimental approach: Effects of low doses of the competitive a2-adrenoceptor antagonists—atipamezole (0.08, 0.8 ng), yohimbine (0.02, 2 ng), mirtazapine (0.02 ng) and idazoxan (0.08 ng) were investigated on intrathecal morphine analgesia, as well as acute and chronic morphine antinociceptive tolerance using the rat tail flick and paw pressure tests. Key results: At doses markedly lower than those producing a2-adrenoceptor blockade, atipamezole, yohimbine, mirtazapine and idazoxan, prolonged the antinociceptive effects of morphine. When co-administered with repeated acute spinal injections of morphine, all four agents blocked the induction of acute tolerance. Co-injection of atipamezole with morphine for 5 days inhibited the development of tolerance in a chronic treatment paradigm. Spinal administration of atipamezole also reversed established antinociceptive tolerance to morphine as indicated by the restoration of morphine antinociceptive potency. The effects of atipamezole on spinal morphine tolerance were not influenced by treatment with 6-hydroxydopamine. -

Supplementary Material Final Submitted
Supplementary material S1 Ciprofloxacin, Danofloxacin, Difloxacin, Enrofloxacin, Flumequine, Marbofloxacin, Nalidixic acid, Norfloxacin, Oxolinic acid, Sarafloxacin, Sulfaguanidine, Sulfanilamide, Sulfachlorpyridazine, Sulfadiazine, Sulfadimethoxine, Sulfadoxine, Sulfamerazine, Sulfamethazine, Sulfamethizole, Sulfamethoxypyridazine, Sulfamonomethoxine, Sulfapyridine, Sulfaquinoxaline, Sulfathiazole, Sulfisoxazole, Sulfamoxole, Trimethoprim, Sulfamethoxazole, Erythromycin, Josamycin, Lincomycin, Spiramycin, Tilmicosin, Tylosin A, Gamithromycin, Tildipirosin, Tulathromycin, Virginiamycin, Pirlimycin, Acetyltylosin-2-O, Tylvalosin, Valnemulin, Rifampicin, Dapsone, Chlortetracycline, Epichlortetracycline, Epitetracycline, Oxytetracycline, Epioxytetracycline, Doxycycline,Tetracycline, Phenoxymethylpenicillin, Benzylpenicillin, Amoxicillin, Ampicillin, Dicloxacillin, Cloxacillin, Nafcillin, Oxacillin, Cefalexin, Cefalonium, Cefapirin, Cefoperazone, Desacetylcefapirin, Cefazolin, Cefquinome, Ceftiofur. S2 1,2-dichlorobenzene, 16ß-hydroxystanozolol, 17a-nortestosterone, 17a-trenbolone, 17ß-estradiol, 17ß-trenbolone, 2 4 6-triaminopyrimidine-5-carbonitrile, 2 4-dimethylaniline, 2ß-hydroxy-N- deethyltiamulin, 2ß-hydroxytiamulin, 3-O-acetyltylosin, 4 4'-dinitrocarbanilide/Nicarbazin (500) , 4- demethylgriseofulvin, 4-methylaminoantipyrine, 5-hydroxyflunixin, 5-hydroxythiabendazole, 6- demethylgriseofulvin, 8a-hydroxymutilin, 8a-hydroxy-N-deethyltiamulin, 8a-hydroxytiamulin, Abamectin B1a, Acepromazine, Acetylisovaleryltylosin, Acyclovir, AHD, Aklomide, -

Non-Clinical Review(S) Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209830Orig1s000 NON-CLINICAL REVIEW(S) DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH PHARMACOLOGY/TOXICOLOGY NDA REVIEW AND EVALUATION Application number: 209830 Supporting document/s: 1, 4, 9, 19 Applicant’s letter date: 8/31/17, 11/6/17, 11/22/17, 3/12/18 CDER stamp date: 8/31/17, 11/6/17, 11/22/17, 3/12/18 Product: ARISTADA INITIO Aripiprazole lauroxil NanoCrystal® Dispersion (AL-NCD, aripiprazole lauroxil nano and ALKS 9072N) Indication: As a starting dose to initiate ARISTADA® (aripiprazole lauroxil) treatment for schizophrenia (b) (4) Applicant: Alkermes, Inc. Review Division: Psychiatry Products Reviewer: Amy M. Avila, PhD Supervisor/Team Leader: Aisar Atrakchi, PhD Division Director: Mitchell Mathis, MD Project Manager: Kofi Ansah, PharmD Template Version: September 1, 2010 Disclaimer Except as specifically identified, all data and information discussed below and necessary for approval of NDA 209830 are owned by Alkermes or are data for which Alkermes has obtained a written right of reference. Any information or data necessary for approval of NDA 209830 that Alkermes does not own or have a written right to reference constitutes one of the following: (1) published literature, or (2) a prior FDA finding of safety or effectiveness for a listed drug, as reflected in the drug’s approved labeling. Any data or information described or referenced below from reviews or publicly available summaries of a previously approved application is for descriptive purposes only and is not relied upon for approval of NDA 209830. -

Orientation for New Clinicians
PROFESSIONAL AFFAIRS ORIENTATION FOR NEW CLINICIANS TABLE OF CONTENTS SCORE: CLINICAL ORIENTATION ........................................................................................... 4 I. SCHEDULE ........................................................................................................................ 5 A. QGenda ......................................................................................................................... 5 B. Weekly Schedule .......................................................................................................... 5 C. OR Daily Schedule ....................................................................................................... 5 D. Anesthesia Daily Call Team ......................................................................................... 6 II. ELECTRONIC MEDICAL RECORD ............................................................................... 6 A. BIDMC Portal: ............................................................................................................. 6 B. Anesthesia Intranet ....................................................................................................... 6 C. Perioperative Information Management System (PIMS) ............................................. 7 D. Talis: ............................................................................................................................. 7 E. Online Medical Record (OMR): .................................................................................. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

National Industrial Hemp Strategy
National Industrial Hemp Strategy Prepared for: Manitoba Agriculture, Food and Rural Initiative Agriculture and Agri-Food Canada Contract Number: ARDI III B-27 March 30th, 2008 George Brook, Partner 293 Duncairn Ave. Ottawa, ON, Canada K1Z 7H1 Email: [email protected] Phone / Cell: 613-863-5119 Fax: 613-249-7064 TAG Project Team: George Brook, Kristopher Liljefors, David Brook, Andy Stewart National Industrial Hemp Strategy ii March 2008 Executive Summary Growth of the Canadian Industrial Hemp Sector The history of hemp cultivation is as old as the history of civilization. In North America, hemp was a crucial crop during the colonial period, and it continued to be produced right up to and through the Second World War. A combination of regulatory pressures and changing public perceptions around drug use led to the disappearance of domestic hemp cultivation in North America in the years following WW II. In 1998, Canada joined the large international community of hemp producers by permitting the production of industrial hemp, under a carefully monitored regulatory process. While the growth of the Canadian industrial hemp sector over the past decade has been uneven and at times fraught with challenges, as would be expected from a fledgling industry, there is considerable cause for optimism: The market for hemp seed materials for human health, nutrition, and personal care applications is strong and growing. Market price for a drum of conventionally grown hemp oil is approximately $1600 Cdn, with organic hem oil fetching in the neighbourhood of $2500 a drum (Spring 2008). A favourable court decision in 2004 re-opened the US market, which had been effectively closed in 2000 by the US Drug Enforcement Agency (DEA).