Benzodiazepine Withdrawal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
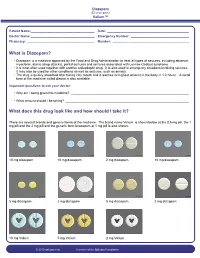
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Drug & Alcohol Testing Program
Pottawattmie County Drug & Alcohol Testing Program Appendix A Table of Contents POLICY STATEMENT ...................................................................................................................................... 3 SCOPE ............................................................................................................................................................ 4 EDUCATION AND TRAINING .......................................................................................................................... 4 DESIGNATED EMPLOYER REPRESENTATIVE (DER): ....................................................................................... 5 DUTY TO COOPERATE ................................................................................................................................... 5 EMPLOYEE ADMISSION OF ALCOHOL AND CONTROLLED SUBSTANCE USE: (49 CFR Part 382.121) ... 6 PROHIBITED DRUGS AND ILLEGALLY USED CONTROLLED SUBSTANCES: ..................................................... 7 PROHIBITED BEHAVIOR AND CONDUCT: ...................................................................................................... 8 DRUG & ALCOHOL TESTING REQUIREMENTS (49 CFR, Part 40 & 382) ............................................... 10 DRUG & ALCOHOL TESTING CIRCUMSTANCES (49 CFR Part 40 & 382) .............................................. 12 A. Pre-Employment Testing: .................................................................................................... 12 B. Reasonable Suspicion Testing: ......................................................................................... -

Uso Adecuado De BZD En Insomnio Y Ansiedad.Pdf
Vol. 6 Nº 1 · OCTUBRE 2014 BOLETÍN CANARIO DE USO RACIONAL DEL MEDICAMENTO DEL SCS Uso adecuado de BENZODIAZEPINAS en insomnio y ansiedad. SUMARIO PERFIL FARMACOLÓGICO DE LAS BZD (Tabla 1). - INTRODUCCIÓN 1 - PERFIL FARMACOLÓGICO DE LAS BENZODIAZEPINAS 1 No todas las BZD son iguales, ni tienen las mismas indicaciones. - BENZODIAZEPINAS EN EL INSOMNIO 2 Conocer algunos aspectos sobre su perfil farmacológico es esencial para realizar una prescripción adecuada y segura. - BENZODIAZEPINAS EN LA ANSIEDAD 4 - RECOMENDACIONES PARA SUSPENDER 5 Por lo general las BZD se absorben muy bien por vía oral, mientras TRATAMIENTOS CON BZD que la vía intramuscular presenta una absorción lenta e irregular, por - BIBLIOGRAFÍA 7 lo que no suele ser muy recomendada. En situaciones de emergencia (convulsiones) es preferible utilizar la vía endovenosa. INTRODUCCIÓN Inicio de acción y vida media: el inicio de acción es distinto según el principio activo y constituye un criterio fundamental en la selección de Las benzodiazepinas (BZD) son psicofármacos que actúan aumentan- las BZD. Puede ser: de inicio rápido (0,5-1 h), de utilidad en el insomnio do la acción del ácido gammaaminobutírico (GABA), principal neuro- de conciliación y en crisis de ansiedad; de inicio intermedio (1-3 h) o transmisor inhibidor del sistema nervioso central. Tienen indicaciones de inicio lento (> 3 h), preferibles en insomnio de mantenimiento o terapéuticas diversas, y auque su uso más habitual es en el tratamien- despertar precoz y en la ansiedad generalizada. to de la ansiedad e insomnio, también se utilizan en la inducción a la anestesia, en el tratamiento de las crisis comiciales, en el síndrome La vida media de las BZD es otro de los criterios de selección y puede 5 de abstinencia alcohólica, como tratamiento coadyuvante de de dolor ser : corta (< 6 h); intermedia (6-24 h) y larga (> 24 h). -

Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam
Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam Tjiauw-Ling Tan, MD, Edward 0. Bixler, PhD, Anthony Kales, MD, Roger J. Cadieux, MD, and Amy L. Goodman, MD Hershey, Pennsylvania A psychiatric syndrome characterized by agita Sleep Disorders Clinic. He began taking triazolam tion, paranoid ideation, depersonalization, and de at bedtime in a 0.5-mg dose eight months before pression, as well as paresthesias and hyperacusis, his referral. Although the drug was effective ini has been attributed to administration of triazolam tially, tolerance developed, causing the patient to (Halcion).1 The occurrence of these reactions led gradually increase the dosage until eventually he to the removal of the drug from the market in the was taking a total of 1.5 mg nightly. Netherlands. Isolated behavioral side effects that The physical examination revealed no contribu include amnesia2-4 and hallucinations5 have also tory conditions. However, assessment of the pa been reported with administration of triazolam. tient’s mental status revealed that he was extreme Rebound insomnia6 and early morning insom ly guarded and suspicious and preoccupied with nia,7 both associated with increases in daytime his sleeplessness to the degree that this hypochon anxiety,7,8 are withdrawal syndromes known driacal concern had a delusional quality. He also to occur with rapidly eliminated benzodiazepine described two episodes indicating memory impair hypnotics such as triazolam. Rebound insomnia ment; both incidents occurred in the late afternoon consists of a marked increase in wakefulness and involved preparing to eat certain foods, which above baseline levels following drug withdrawal. -

Guidelines for the Forensic Analysis of Drugs Facilitating Sexual Assault and Other Criminal Acts
Vienna International Centre, PO Box 500, 1400 Vienna, Austria Tel.: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org Guidelines for the Forensic analysis of drugs facilitating sexual assault and other criminal acts United Nations publication Printed in Austria ST/NAR/45 *1186331*V.11-86331—December 2011 —300 Photo credits: UNODC Photo Library, iStock.com/Abel Mitja Varela Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Guidelines for the forensic analysis of drugs facilitating sexual assault and other criminal acts UNITED NATIONS New York, 2011 ST/NAR/45 © United Nations, December 2011. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. List of abbreviations . v Acknowledgements .......................................... vii 1. Introduction............................................. 1 1.1. Background ........................................ 1 1.2. Purpose and scope of the manual ...................... 2 2. Investigative and analytical challenges ....................... 5 3 Evidence collection ...................................... 9 3.1. Evidence collection kits .............................. 9 3.2. Sample transfer and storage........................... 10 3.3. Biological samples and sampling ...................... 11 3.4. Other samples ...................................... 12 4. Analytical considerations .................................. 13 4.1. Substances encountered in DFSA and other DFC cases .... 13 4.2. Procedures and analytical strategy...................... 14 4.3. Analytical methodology .............................. 15 4.4. -

MEDICATION GUIDE RESTORIL™ (Res-Tə-Ril) (Temazepam) Capsules
MEDICATION GUIDE RESTORIL™ (res-tə-ril) (temazepam) Capsules, C-IV What is the most important information I should know about RESTORIL? RESTORIL is a benzodiazepine medicine. Taking benzodiazepines with opioid medicines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, breathing problems (respiratory depression), coma and death. After taking RESTORIL, you may get up out of bed while not being fully awake and do an activity that you do not know you are doing. The next morning, you may not remember that you did anything during the night. You have a higher chance for doing these activities if you drink alcohol or take other medicines that make you sleepy with RESTORIL. Reported activities include: o driving a car (“sleep-driving”) o making and eating food o talking on the phone o having sex o sleep-walking Call your healthcare provider right away if you find out that you have done any of the above activities after taking RESTORIL. Do not take RESTORIL unless you are able to stay in bed a full night (7 to 8 hours) before you must be active again. Do not take more RESTORIL than prescribed. What is RESTORIL? RESTORIL is a prescription sleep medicine. RESTORIL is used in adults for the short-term (usually 7 to 10 days) treatment of a sleep problem called insomnia. Symptoms of insomnia include trouble falling asleep and waking up often during the night. RESTORIL is a federal controlled substance (C-IV) because it can be abused or lead to dependence. Keep RESTORIL in a safe place to prevent misuse and abuse. -

Neonatal Drug Withdrawal Abstract
Guidance for the Clinician in Rendering Pediatric Care CLINICAL REPORT Neonatal Drug Withdrawal Mark L. Hudak, MD, Rosemarie C. Tan, MD,, PhD, THE abstract COMMITTEE ON DRUGS, and THE COMMITTEE ON FETUS AND Maternal use of certain drugs during pregnancy can result in transient NEWBORN neonatal signs consistent with withdrawal or acute toxicity or cause KEY WORDS opioid, methadone, heroin, fentanyl, benzodiazepine, cocaine, sustained signs consistent with a lasting drug effect. In addition, hos- methamphetamine, SSRI, drug withdrawal, neonate, abstinence pitalized infants who are treated with opioids or benzodiazepines to syndrome provide analgesia or sedation may be at risk for manifesting signs ABBREVIATIONS of withdrawal. This statement updates information about the clinical CNS—central nervous system — presentation of infants exposed to intrauterine drugs and the thera- DTO diluted tincture of opium ECMO—extracorporeal membrane oxygenation peutic options for treatment of withdrawal and is expanded to include FDA—Food and Drug Administration evidence-based approaches to the management of the hospitalized in- 5-HIAA—5-hydroxyindoleacetic acid fant who requires weaning from analgesics or sedatives. Pediatrics ICD-9—International Classification of Diseases, Ninth Revision — – NAS neonatal abstinence syndrome 2012;129:e540 e560 SSRI—selective serotonin reuptake inhibitor INTRODUCTION This document is copyrighted and is property of the American fi Academy of Pediatrics and its Board of Directors. All authors Use and abuse of drugs, alcohol, and tobacco contribute signi cantly have filed conflict of interest statements with the American to the health burden of society. The 2009 National Survey on Drug Use Academy of Pediatrics. Any conflicts have been resolved through and Health reported that recent (within the past month) use of illicit a process approved by the Board of Directors. -

Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW
Guideline Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW Summary To provide the most up-to-date knowledge and current level of best practice for the treatment of withdrawal from alcohol and other drugs such as heroin, and other opioids, benzodiazepines, cannabis and psychostimulants. Document type Guideline Document number GL2008_011 Publication date 04 July 2008 Author branch Centre for Alcohol and Other Drugs Branch contact (02) 9424 5938 Review date 18 April 2018 Policy manual Not applicable File number 04/2766 Previous reference N/A Status Active Functional group Clinical/Patient Services - Pharmaceutical, Medical Treatment Population Health - Pharmaceutical Applies to Area Health Services/Chief Executive Governed Statutory Health Corporation, Board Governed Statutory Health Corporations, Affiliated Health Organisations, Affiliated Health Organisations - Declared Distributed to Public Health System, Ministry of Health, Public Hospitals Audience All groups of health care workers;particularly prescribers of opioid treatments Secretary, NSW Health Guideline Ministry of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW space Document Number GL2008_011 Publication date 04-Jul-2008 Functional Sub group Clinical/ Patient Services - Pharmaceutical Clinical/ Patient Services - Medical Treatment Population Health - Pharmaceutical -

Substance Abuse and Dependence
9 Substance Abuse and Dependence CHAPTER CHAPTER OUTLINE CLASSIFICATION OF SUBSTANCE-RELATED THEORETICAL PERSPECTIVES 310–316 Residential Approaches DISORDERS 291–296 Biological Perspectives Psychodynamic Approaches Substance Abuse and Dependence Learning Perspectives Behavioral Approaches Addiction and Other Forms of Compulsive Cognitive Perspectives Relapse-Prevention Training Behavior Psychodynamic Perspectives SUMMING UP 325–326 Racial and Ethnic Differences in Substance Sociocultural Perspectives Use Disorders TREATMENT OF SUBSTANCE ABUSE Pathways to Drug Dependence AND DEPENDENCE 316–325 DRUGS OF ABUSE 296–310 Biological Approaches Depressants Culturally Sensitive Treatment Stimulants of Alcoholism Hallucinogens Nonprofessional Support Groups TRUTH or FICTION T❑ F❑ Heroin accounts for more deaths “Nothing and Nobody Comes Before than any other drug. (p. 291) T❑ F❑ You cannot be psychologically My Coke” dependent on a drug without also being She had just caught me with cocaine again after I had managed to convince her that physically dependent on it. (p. 295) I hadn’t used in over a month. Of course I had been tooting (snorting) almost every T❑ F❑ More teenagers and young adults die day, but I had managed to cover my tracks a little better than usual. So she said to from alcohol-related motor vehicle accidents me that I was going to have to make a choice—either cocaine or her. Before she than from any other cause. (p. 297) finished the sentence, I knew what was coming, so I told her to think carefully about what she was going to say. It was clear to me that there wasn’t a choice. I love my T❑ F❑ It is safe to let someone who has wife, but I’m not going to choose anything over cocaine. -

Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin Healthcare
Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin healthcare 4/22/2020 Overview benzodiazepines • Examples of benzos and benzo like drugs • Indications for benzos • Pharmacology of benzos • Side effects and contraindications • Benzo withdrawal • Benzo tapers 12/06/2018 Sedative/Hypnotics • Benzodiazepines • Alcohol • Z-drugs (Benzo-like sleeping aids) • Barbiturates • GHB • Propofol • Some inhalants • Gabapentin? Pregabalin? 12/06/2018 Examples of benzodiazepines • Midazolam (Versed) • Triazolam (Halcion) • Alprazolam (Xanax) • Lorazepam (Ativan) • Temazepam (Restoril) • Oxazepam (Serax) • Clonazepam (Klonopin) • Diazepam (Valium) • Chlordiazepoxide (Librium) 4/22/2020 Sedatives: gaba stimulating drugs have incomplete “cross tolerance” 12/06/2018 Effects from sedative (Benzo) use • Euphoria/bliss • Suppresses seizures • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Sleep inducing • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 Tolerance to benzo effects? • Effects quickly diminish with repeated use (weeks) • Euphoria/bliss • Suppresses seizures • Effects incompletely diminish with repeated use • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Seep inducing • Durable effects with repeated use • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 If you understand this pharmacology you can figure out the rest... • Potency • 1 mg diazepam <<< 1 mg alprazolam • Duration of action • Half life differences • Onset of action • Euphoria, clinical utility in acute -

Benzodiazepines
Benzodiazepines Using benzodiazepines in Children and Adolescents Overview Benzodiazepines are group of medications used to treat several different conditions. Some examples of these medications include: lorazepam (Ativan®); clonazepam (Rivotril®); alprazolam (Xanax®) and oxazepam (Serax®). Other benzodiazepine medications are available, but are less commonly used in children and adolescents. What are benzodiazepines used for? Benzodiazepines may be used for the following conditions: • anxiety disorders: generalized anxiety disorder; social anxiety disorder; post-traumatic stress disorder (PTSD); panic attacks/disorder; excessive anxiety prior to surgery • sleep disorders: trouble sleeping (insomnia); waking up suddenly with great fear (night terrors); sleepwalking • seizure disorders (epilepsy) • alcohol withdrawal • treatment of periods of extreme slowing or excessive purposeless motor activity (catatonia) Your doctor may be using this medication for another reason. If you are unclear why this medication is being prescribed, please ask your doctor. How do benzodiazepines work? Benzodiazepines works by affecting the activity of the brain chemical (neurotransmitter) called GABA. By enhancing the action of GABA, benzodiazepines have a calming effect on parts of the brain that are too excitable. This in turn helps to manage anxiety, insomnia, and seizure disorders. How well do benzodiazepines work in children and adolescents? When used to treat anxiety disorders, benzodiazepines decrease symptoms such as nervousness, fear, and excessive worrying. Benzodiazepines may also help with the physical symptoms of anxiety, including fast or strong heart beat, trouble breathing, dizziness, shakiness, sweating, and restlessness. Typically, benzodiazepines are prescribed to manage anxiety symptoms that are uncomfortable, frightening or interfere with daily activities for a short period of time before conventional anti-anxiety treatments like cognitive-behavioural therapy or anti-anxiety takes effect.