Dehydroepiandrosterone and Erectile Function: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
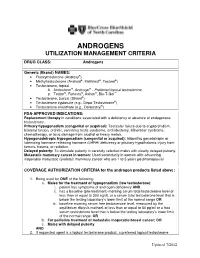
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis
ORIGINAL ARTICLE Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis Ana E. Espinosa De Ycaza, Robert A. Rizza, K. Sreekumaran Nair, and Michael D. Jensen Division of Endocrinology, Endocrine Research Unit, Mayo Clinic, Rochester, Minnesota 55905 Downloaded from https://academic.oup.com/jcem/article/101/4/1719/2804555 by guest on 24 September 2021 Context: Dehydroepiandrosterone (DHEA) and T hormones are advertised as antiaging, antiobe- sity products. However, the evidence that these hormones have beneficial effects on adipose tissue metabolism is limited. Objective: The objective of the study was to determine the effect of DHEA and T supplementation on systemic lipolysis during a mixed-meal tolerance test (MMTT) and an iv glucose tolerance test (IVGTT). Design: This was a 2-year randomized, double-blind, placebo-controlled trial. Setting: The study was conducted at a general clinical research center. Participants: Sixty elderly women with low DHEA concentrations and 92 elderly men with low DHEA and bioavailable T concentrations participated in the study. Interventions: Elderly women received 50 mg DHEA (n ϭ 30) or placebo (n ϭ 30). Elderly men received 75 mg DHEA (n ϭ 30),5mgT(nϭ 30), or placebo (n ϭ 32). Main Outcome Measures: In vivo measures of systemic lipolysis (palmitate rate of appearance) during a MMTT or IVGTT. Results: At baseline there was no difference in insulin suppression of lipolysis measured during MMTT and IVGTT between the treatment groups and placebo. For both sexes, a univariate analysis showed no difference in changes in systemic lipolysis during the MMTT or IVGTT in the DHEA group and T group when compared with placebo. -

Reproductive DHEA-S
Reproductive DHEA-S Analyte Information - 1 - DHEA-S Introduction DHEA-S, DHEA sulfate or dehydroepiandrosterone sulfate, it is a metabolite of dehydroepiandrosterone (DHEA) resulting from the addition of a sulfate group. It is the sulfate form of aromatic C19 steroid with 10,13-dimethyl, 3-hydroxy group and 17-ketone. Its chemical name is 3β-hydroxy-5-androsten-17-one sulfate, its summary formula is C19H28O5S and its molecular weight (Mr) is 368.5 Da. The structural formula of DHEA-S is shown in (Fig.1). Fig.1: Structural formula of DHEA-S Other names used for DHEA-S include: Dehydroisoandrosterone sulfate, (3beta)-3- (sulfooxy), androst-5-en-17-one, 3beta-hydroxy-androst-5-en-17-one hydrogen sulfate, Prasterone sulfate and so on. As DHEA-S is very closely connected with DHEA, both hormones are mentioned together in the following text. Biosynthesis DHEA-S is the major C19 steroid and is a precursor in testosterone and estrogen biosynthesis. DHEA-S originates almost exclusively in the zona reticularis of the adrenal cortex (Fig.2). Some may be produced by the testes, none is produced by the ovaries. The adrenal gland is the sole source of this steroid in women, whereas in men the testes secrete 5% of DHEA-S and 10 – 20% of DHEA. The production of DHEA-S and DHEA is regulated by adrenocorticotropin (ACTH). Corticotropin-releasing hormone (CRH) and, to a lesser extent, arginine vasopressin (AVP) stimulate the release of adrenocorticotropin (ACTH) from the anterior pituitary gland (Fig.3). In turn, ACTH stimulates the adrenal cortex to secrete DHEA and DHEA-S, in addition to cortisol. -

Safety Data Sheet
SAFETY DATA SHEET SECTION 1: PRODUCT IDENTIFICATION PRODUCT NAME DHEA (Prasterone) (Micronized) PRODUCT CODE 0733 SUPPLIER MEDISCA Inc. Tel.: 1.800.932.1039 | Fax.: 1.855.850.5855 661 Route 3, Unit C, Plattsburgh, NY, 12901 3955 W. Mesa Vista Ave., Unit A-10, Las Vegas, NV, 89118 6641 N. Belt Line Road, Suite 130, Irving, TX, 75063 MEDISCA Pharmaceutique Inc. Tel.: 1.800.665.6334 | Fax.: 514.338.1693 4509 Rue Dobrin, St. Laurent, QC, H4R 2L8 21300 Gordon Way, Unit 153/158, Richmond, BC V6W 1M2 MEDISCA Australia PTY LTD Tel.: 1.300.786.392 | Fax.: 61.2.9700.9047 Unit 7, Heritage Business Park 5-9 Ricketty Street, Mascot, NSW 2020 EMERGENCY PHONE CHEMTREC Day or Night Within USA and Canada: 1-800-424-9300 NSW Poisons Information Centre: 131 126 USES Adjuvant; Androgen SECTION 2: HAZARDS IDENTIFICATION GHS CLASSIFICATION Toxic to Reproduction (Category 2) PICTOGRAM SIGNAL WORD Warning HAZARD STATEMENT(S) Reproductive effector, prohormone. Suspected of damaging fertility or the unborn child. May cause harm to breast-fed children. Causes serious eye irritation. Causes skin and respiratory irritation. Very toxic to aquatic life with long lasting effects. AUSTRALIA-ONLY HAZARDS Not Applicable. PRECAUTIONARY STATEMENT(S) Prevention Wash thoroughly after handling. Obtain special instructions before use. Do not handle until all safety precautions have been read and understood. Do not breathe dusts or mists. Do not eat, drink or smoke when using this product. Avoid contact during pregnancy/while nursing. Wear protective gloves, protective clothing, eye protection, face protection. Avoid release to the environment. Response IF ON SKIN (HAIR): Wash with plenty of water. -

Adverse Effects of Anabolic-Androgenic Steroids: a Literature Review
healthcare Review Adverse Effects of Anabolic-Androgenic Steroids: A Literature Review Giuseppe Davide Albano 1,†, Francesco Amico 1,†, Giuseppe Cocimano 1, Aldo Liberto 1, Francesca Maglietta 2, Massimiliano Esposito 1, Giuseppe Li Rosi 3, Nunzio Di Nunno 4, Monica Salerno 1,‡ and Angelo Montana 1,*,‡ 1 Legal Medicine, Department of Medical, Surgical and Advanced Technologies, “G.F. Ingrassia”, University of Catania, 95123 Catania, Italy; [email protected] (G.D.A.); [email protected] (F.A.); [email protected] (G.C.); [email protected] (A.L.); [email protected] (M.E.); [email protected] (M.S.) 2 Department of Clinical and Experimental Medicine, University of Foggia, 71122 Foggia, Italy; [email protected] 3 Department of Law, Criminology, Magna Graecia University of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of History, Society and Studies on Humanity, University of Salento, 73100 Lecce, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-095-3782153 † These authors contributed equally to this work. ‡ These authors share last authorship. Abstract: Anabolic-androgenic steroids (AASs) are a large group of molecules including endoge- nously produced androgens, such as testosterone, as well as synthetically manufactured derivatives. AAS use is widespread due to their ability to improve muscle growth for aesthetic purposes and athletes’ performance, minimizing androgenic effects. AAS use is very popular and 1–3% of US inhabitants have been estimated to be AAS users. However, AASs have side effects, involving all organs, tissues and body functions, especially long-term toxicity involving the cardiovascular system Citation: Albano, G.D.; Amico, F.; and the reproductive system, thereby, their abuse is considered a public health issue. -

Steroid Sulfatase Stimulates Intracrine Androgen Synthesis and Is a Therapeutic Target for Advanced Prostate Cancer
Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Steroid sulfatase stimulates intracrine androgen synthesis and is a therapeutic target for advanced prostate cancer Cameron M. Armstrong1*, Chengfei Liu1*, Liangren Liu1,2*, Joy C. Yang1, Wei Lou1, Ruining Zhao1,3, Shu Ning1, Alan P. Lombard1, Jinge Zhao1, Leandro S D'Abronzo1, Christopher P. Evans1,4, Pui-Kai Li5, Allen C. Gao1, 4, 6,7 Running title: Targeting steroid sulfatase for advanced prostate cancer Key words: Prostate cancer, steroid sulfatase, resistance, intracrine androgen synthesis, adrenal androgens 1Department of Urologic Surgery, University of California Davis, CA, USA 2Present address: Department of Urology, West China Hospital, Sichuan University, China 3Present address: Department of Urology, General Hospital of Ningxia Medical University, China 4UC Davis Comprehensive Cancer Center, University of California Davis, CA, USA 5Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, The Ohio State University, Columbus, OH, USA 6VA Northern California Health Care System, Sacramento, CA, USA 7Corresponding author: Allen Gao, University of California Davis, 4645 2nd Avenue, Sacramento, CA 95817, USA. Phone: 916-734-8718, email: [email protected] *These authors contributed equally to the work. Conflict of interest: PKL and ACG are co-inventors of a patent application of the selected small molecule inhibitors of steroid sulfatase. 1 Downloaded from clincancerres.aacrjournals.org on October 1, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Steroids and Other Appearance and Performance Enhancing Drugs (Apeds) Research Report
Research Report Revised Febrero 2018 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Table of Contents Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Introduction What are the different types of APEDs? What is the history of anabolic steroid use? Who uses anabolic steroids? Why are anabolic steroids misused? How are anabolic steroids used? What are the side effects of anabolic steroid misuse? How does anabolic steroid misuse affect behavior? What are the risks of anabolic steroid use in teens? How do anabolic steroids work in the brain? Are anabolic steroids addictive? How are anabolic steroids tested in athletes? What can be done to prevent steroid misuse? What treatments are effective for anabolic steroid misuse? Where can I get further information about steroids? References Page 1 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Esta publicación está disponible para su uso y puede ser reproducida, en su totalidad, sin pedir autorización al NIDA. Se agradece la citación de la fuente, de la siguiente manera: Fuente: Instituto Nacional sobre el Abuso de Drogas; Institutos Nacionales de la Salud; Departamento de Salud y Servicios Humanos de los Estados Unidos. Introduction Appearance and performance enhancing drugs (APEDs) are most often used by males to improve appearance by building muscle mass or to enhance athletic performance. Although they may directly and indirectly have effects on a user’s mood, they do not produce a euphoric high, which makes APEDs distinct from other drugs such as cocaine, heroin, and marijuana. However, users may develop a substance use disorder, defined as continued use despite adverse consequences. -

The Effects of Dehydroepiandrosterone Sulfate on Counterregulatory Responses During Repeated Hypoglycemia in Conscious Normal Rats Darleen A
The Effects of Dehydroepiandrosterone Sulfate on Counterregulatory Responses During Repeated Hypoglycemia in Conscious Normal Rats Darleen A. Sandoval, Ling Ping, Ray Anthony Neill, Sachiko Morrey, and Stephen N. Davis ⅐ ؊1 ⅐ ؊1 We previously determined that both antecedent hy- mol/l kg min ; P < 0.05). In summary, day-1 poglycemia and elevated cortisol levels blunt neu- antecedent hypoglycemia blunted neuroendocrine and roendocrine and metabolic responses to subsequent metabolic responses to next-day hypoglycemia. How- hypoglycemia in conscious, unrestrained rats. The adre- ever, simultaneous DHEA-S infusion during antecedent nal steroid dehydroepiandrosterone sulfate (DHEA-S) hypoglycemia preserved neuroendocrine and metabolic has been shown in several studies to oppose corticoste- counterregulatory responses during subsequent hypo- roid action. The purpose of this study was to determine glycemia in conscious rats. Diabetes 53:679–686, 2004 if DHEA-S could preserve counterregulatory responses during repeated hypoglycemia. We studied 40 male Sprague-Dawley rats during a series of 2-day protocols. he Diabetes Control and Complications Trial Day 1 consisted of two 2-h episodes of 1) hyperinsuline- mic (30 pmol ⅐ kg؊1 ⅐ min؊1) euglycemia (6.2 ؎ 0.2 established that intensive glucose control in type ANTE EUG), 2) hyperinsulinemic eug- 1 diabetic patients can slow the progression or ;12 ؍ mmol/l; n -plus simultaneous Tsignificantly reduce the onset of diabetic micro (8 ؍ lycemia (6.0 ؎ 0.1 mmol/l; n intravenous infusion of DHEA-S (30 mg/kg; ANTE EUG vascular complications (e.g., retinopathy, nephropathy, ؉ DHEA-S), 3) hyperinsulinemic hypoglycemia (2.8 ؎ neuropathy) (1). Unfortunately, the study also established ANTE HYPO), or 4) hyperinsulinemic that intensive glucose treatment causes an approximate ;12 ؍ mmol/l; n 0.1 -with simulta- threefold increase in the frequency of severe hypoglyce (8 ؍ hypoglycemia (2.8 ؎ 0.1 mmol/l; n neous intravenous infusion of DHEA-S (30 mg/kg; ANTE mia (2). -

DHEA Sulfate, and Aging: Contribution of the Dheage Study to a Sociobiomedical Issue
Dehydroepiandrosterone (DHEA), DHEA sulfate, and aging: Contribution of the DHEAge Study to a sociobiomedical issue Etienne-Emile Baulieua,b, Guy Thomasc, Sylvie Legraind, Najiba Lahloue, Marc Rogere, Brigitte Debuiref, Veronique Faucounaug, Laurence Girardh, Marie-Pierre Hervyi, Florence Latourj, Marie-Ce´ line Leaudk, Amina Mokranel, He´ le` ne Pitti-Ferrandim, Christophe Trivallef, Olivier de Lacharrie` ren, Stephanie Nouveaun, Brigitte Rakoto-Arisono, Jean-Claude Souberbiellep, Jocelyne Raisonq, Yves Le Boucr, Agathe Raynaudr, Xavier Girerdq, and Franc¸oise Foretteg,j aInstitut National de la Sante´et de la Recherche Me´dicale Unit 488 and Colle`ge de France, 94276 Le Kremlin-Biceˆtre, France; cInstitut National de la Sante´et de la Recherche Me´dicale Unit 444, Hoˆpital Saint-Antoine, 75012 Paris, France; dHoˆpital Bichat, 75877 Paris, France; eHoˆpital Saint-Vincent de Paul, 75014 Paris, France; fHoˆpital Paul Brousse, 94804 Villejuif, France; gFondation Nationale de Ge´rontologie, 75016 Paris, France; hHoˆpital Charles Foix, 94205 Ivry, France; iHoˆpital de Biceˆtre, 94275 Biceˆtre, France; jHoˆpital Broca, 75013 Paris, France; kCentre Jack-Senet, 75015 Paris, France; lHoˆpital Sainte-Perine, 75016 Paris, France; mObservatoire de l’Age, 75017 Paris, France; nL’Ore´al, 92583 Clichy, France; oInstitut de Sexologie, 75116 Paris, France; pHoˆpital Necker, 75015 Paris, France; qHoˆpital Broussais, 75014 Paris, France; and rHoˆpital Trousseau, 75012 Paris, France Contributed by Etienne-Emile Baulieu, December 23, 1999 The secretion and the blood levels of the adrenal steroid dehydro- number of consumers. Extravagant publicity based on fantasy epiandrosterone (DHEA) and its sulfate ester (DHEAS) decrease pro- (‘‘fountain of youth,’’ ‘‘miracle pill’’) or pseudoscientific asser- foundly with age, and the question is posed whether administration tion (‘‘mother hormone,’’ ‘‘antidote for aging’’) has led to of the steroid to compensate for the decline counteracts defects unfounded radical assertions, from superactivity (‘‘keep young,’’ associated with aging. -

Receptor Af®Nity and Potency of Non-Steroidal Antiandrogens: Translation of Preclinical ®Ndings Into Clinical Activity
Prostate Cancer and Prostatic Diseases (1998) 1, 307±314 ß 1998 Stockton Press All rights reserved 1365±7852/98 $12.00 http://www.stockton-press.co.uk/pcan Review Receptor af®nity and potency of non-steroidal antiandrogens: translation of preclinical ®ndings into clinical activity GJCM Kolvenbag1, BJA Furr2 & GRP Blackledge3 1Medical Affairs, Zeneca Pharmaceuticals, Wilmington, DE, USA; 2Therapeutic Research Department, and 3Medical Research Department, Zeneca Pharmaceuticals, Alderley Park, Maccles®eld, Cheshire, UK The non-steroidal antiandrogens ¯utamide (Eulexin1), nilutamide (Anandron1) and bicalutamide (Casodex1) are widely used in the treatment of advanced prostate cancer, particularly in combination with castration. The naturally occurring ligand 5a-DHT has higher binding af®nity at the androgen receptor than the non-steroidal antiandrogens. Bicalutamide has an af®nity two to four times higher than 2-hydroxy¯utamide, the active metabolite of ¯utamide, and around two times higher than nilutamide for wild-type rat and human prostate androgen receptors. Animal studies have indicated that bicalutamide also exhi- bits greater potency in reducing seminal vesicle and ventral prostate weights and inhibiting prostate tumour growth than ¯utamide. Although preclinical data can give an indication of the likely clinical activity, clinical studies are required to determine effective, well-tolerated dosing regimens. As components of combined androgen blockade (CAB), controlled studies have shown survival bene®ts of ¯utamide plus a luteinising hormone-releasing hormone analogue (LHRH-A) over LHRH-A alone, and for nilutamide plus orchiectomy over orchiectomy alone. Other studies have failed to show such survival bene®ts, including those comparing ¯utamide plus orchiectomy with orchiectomy alone, and nilutamide plus LHRH-A with LHRH-A alone.