Community & Family Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

E55a Oil & Gas
a E55A OIL & GAS Essar Oil Limited Date :28.03.2016 Divisional Office SCO, Plot No. - 9, 1st Floor, New Colony Mor, Old Rly. Road, Ref. No.: Haryana/ NOC/Ujina/WL Gurgaon -'122001, Haryana To, Corporate ldentity Number: 1111 00GJl 989P1C03211 6 The Officer ln charge T +91 124 651 4999 email: eolmarketing@essar conr Wild Life Department www essaroil co in Mewat (Haryana) Subject: "NOC for use of forest land for installation of proposed Retail Outlet/ Petrol Pump in Diversion of forest land 0.0152 Hac. for access to the Proposed Petrol Pump of Essar Oil Ltd. Along at KM Stone No 32 (RHS) Chainage 32.889 at Khewat No. 1234, Khatauni No. 1410, Kila No. L24ll23l8-Ol,t39ll3(7-13), Village - Ujina, on Hodel-Nuh Road (RHS), Tehsil- Nuh, District - Mewat, Haryana ." Dear Sir, We propose to install new Retail Outlet/ Petrol Pump in Diversion of forest land 0.0152 Hac. for access to the Proposed Petrol Pump of Essar Oil Ltd. Along at KM Stone No 32 (RHS) Chainage 32.889 at Khewat No. 1234, Khatauni No. 1410, Kila No. I24/123(8-0\, I39/13(7-L3), Village - Ujina, on Hodel-Nuh Road (RHS), Tehsil - Nuh, District - Mewat, Haryana as per enclosed layout plan. This is to apprise you that there is no animal/ Bird Sanctuary is existing in the above identified site. Also there is no danger to the fauna so hereby we request you to kindly arrange to issue NOC for the proposed Retail Outlet/ Petrol Pump on the site under reference. Copy of layout plan of above mentioned site, is attached for your ready reference. -

A Clinicopathological Analysis of Granulomatous
JK SCIENCE ORIGINAL ARTICLE A Clinicopathological Analysis of Granulomatous Dermatitis : 4 Year Retrospective Study Jyotsna Suri, Subhash Bhardwaj, Rita Kumari, Shailija Kotwal Abstract The present study was carried out with an attempt to study the incidence of granulomatous dermatitis in hospital based population and to classify and compare the granulomatous dermatitis on the basis of histopathology and find the etiology. This is a four year retrospective study done on the data available in the dermatopathology section of department of pathology. The cases diagnosed as granulomatous dermatitis were retrieved, clinical data and the histopathological features compared to know the incidence of various etiologies of GD. Out of 310 cases of GD with male to female ratio 2.03:1, leprosy comprised major reported etiology (n-244) followed by tuberculosis (n-44), sarcoidosis (n-4), Leshmania Donovani (n-14)) granuloma annulare (n-1) and 3 granulomatous lesions not further classified. Infections form the commonest form of GD out of which leprosy forms the major group. Role of histopathology(H&E and special stains) is very important in confirming the diagnosis of granulomatous dermatitis . Key Words Granuloma, Dermatitis, Inflammatory, Tissue Injury Introduction Granuloma is defined as a focal chronic inflammatory dermatitis presents a diagnostic challenge, many a times. response to tissue injury, characterised by focal, compact The granulomatous dermatitis comprise a large family collection of inflammatory cells, principally of the activated sharing the common histological denominator of histiocytes, modified epitheloid macrophages & granulomas formation. Rightly said that in granulomatous multinucleate giant cells that may or may not be rimmed dermatitis, an identical histologic picture may be produced by lymphocytes and show central necrosis. -

INTERNATIONAL JOURNAL of LEPROSY Volume 72, Number 1 Printed in the U.S.A
INTERNATIONAL JOURNAL OF LEPROSY Volume 72, Number 1 Printed in the U.S.A. (ISSN 0148-916X) INTERNATIONAL JOURNAL OF LEPROSY and Other Mycobacterial Diseases VOLUME 72, NUMBER 1MARCH 2004 Relapses in Multibacillary Patients Treated with Multi-drug Therapy until Smear Negativity: Findings after Twenty Years1 Gift Norman, Geetha Joseph, and Joseph Richard2 ABSTRACT The Schieffelin Leprosy Research and Training Center at Karigiri, India participated in several of the World Health Organization (WHO) trials. The first trial on combined therapy in multi-bacillary leprosy was initiated in 1981. The main objectives of this field trial were to evaluate the efficacy of WHO recommended regimens in preventing relapses, especially drug resistance relapses. This paper reports on the relapses twenty years after patients were inducted into the WHO field trial. Between 1981 and 1982, 1067 borderline lepromatous and lepromatous patients were in- ducted into the WHO field trial for combined therapy in multi-bacillary leprosy trial. Among them, 357 patients were skin smear positive. During the follow-up in 2002, only 173 of them could be traced and assessed. The mean duration of follow-up was 16.4 ± 1.83 years. Two patients relapsed 14 and 15 years after being released from treatment, the relapse rate being 0.07 per 100 person years follow-up. Drug susceptibility tests done on one of the relapsed patients revealed drug sensitive organisms to all multi-drug therapy drugs. RÉSUMÉ Le centre de recherche et de formation de Schieffelin à Karigiri aux Indes a participé à plusieurs études cliniques sponsorisées par l’Organisation Mondiale de la Santé (OMS). -

Nuh) District, Haryana (India
Current World Environment Vol. 11(2), 388-398 (2016) Analysis of Water Level Fluctuations and TDS Variations in the Groundwater at Mewat (Nuh) District, Haryana (India) PRIYANKA1, GOpal KRISHAN2, LALIT MOHAN SHARMA3, BRIJESH KUMAR Yadav4 and N.C. GHOSH2 1TERI University, New Delhi India. 2National Institute of Hydrology, Roorkee, India. 3Sehgal Foundation, Gurgaon, India. 4IIT-Roorkee, Roorkee, India. http://dx.doi.org/10.12944/CWE.11.2.06 (Received: July 18, 2016; Accepted: August 02, 2016) ABSTRACT Groundwater is the major source for fulfilling the water needs of domestic and agricultural sectors in Mewat district, Haryana, India and its continuous use has put an enormous pressure on the groundwater resource, which along with low rainfall and variable geographical conditions lead to the declining water levels. The other problem of this area is high salinity which is reported intruding to the freshwater zone1. Taking into account the twin problem of declining water level and high salinity the study was taken up jointly by National Institute of Hydrology, Roorkee; Sehgal Foundation, Gurgaon and Indian Institute of Technology, Roorkee. Groundwater level and TDS (Total dissolved solids) data for pre-monsoon and post-monsoon seasons for the time period of 2011–2015 of 40 monitoring wells developed by Sehgal Foundation, Gurgaon was collected and analysed. It has been found that the groundwater level is decreasing in the area while TDS values show inconsistent trends during 2011-15. Further monitoring of the wells is continued to get the more information on water level and TDS which will help in facilitating the researchers in finding out the applicable solutions for the above problems in the Mewat, Haryana. -

Copyright by Mohammad Raisur Rahman 2008
Copyright by Mohammad Raisur Rahman 2008 The Dissertation Committee for Mohammad Raisur Rahman certifies that this is the approved version of the following dissertation: Islam, Modernity, and Educated Muslims: A History of Qasbahs in Colonial India Committee: _____________________________________ Gail Minault, Supervisor _____________________________________ Cynthia M. Talbot _____________________________________ Denise A. Spellberg _____________________________________ Michael H. Fisher _____________________________________ Syed Akbar Hyder Islam, Modernity, and Educated Muslims: A History of Qasbahs in Colonial India by Mohammad Raisur Rahman, B.A. Honors; M.A.; M.Phil. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August 2008 Dedication This dissertation is dedicated to the fond memories of my parents, Najma Bano and Azizur Rahman, and to Kulsum Acknowledgements Many people have assisted me in the completion of this project. This work could not have taken its current shape in the absence of their contributions. I thank them all. First and foremost, I owe my greatest debt of gratitude to my advisor Gail Minault for her guidance and assistance. I am grateful for her useful comments, sharp criticisms, and invaluable suggestions on the earlier drafts, and for her constant encouragement, support, and generous time throughout my doctoral work. I must add that it was her path breaking scholarship in South Asian Islam that inspired me to come to Austin, Texas all the way from New Delhi, India. While it brought me an opportunity to work under her supervision, I benefited myself further at the prospect of working with some of the finest scholars and excellent human beings I have ever known. -

Dictionary of Martyrs: India's Freedom Struggle
DICTIONARY OF MARTYRS INDIA’S FREEDOM STRUGGLE (1857-1947) Vol. 5 Andhra Pradesh, Telangana, Karnataka, Tamil Nadu & Kerala ii Dictionary of Martyrs: India’s Freedom Struggle (1857-1947) Vol. 5 DICTIONARY OF MARTYRSMARTYRS INDIA’S FREEDOM STRUGGLE (1857-1947) Vol. 5 Andhra Pradesh, Telangana, Karnataka, Tamil Nadu & Kerala General Editor Arvind P. Jamkhedkar Chairman, ICHR Executive Editor Rajaneesh Kumar Shukla Member Secretary, ICHR Research Consultant Amit Kumar Gupta Research and Editorial Team Ashfaque Ali Md. Naushad Ali Md. Shakeeb Athar Muhammad Niyas A. Published by MINISTRY OF CULTURE, GOVERNMENT OF IDNIA AND INDIAN COUNCIL OF HISTORICAL RESEARCH iv Dictionary of Martyrs: India’s Freedom Struggle (1857-1947) Vol. 5 MINISTRY OF CULTURE, GOVERNMENT OF INDIA and INDIAN COUNCIL OF HISTORICAL RESEARCH First Edition 2018 Published by MINISTRY OF CULTURE Government of India and INDIAN COUNCIL OF HISTORICAL RESEARCH 35, Ferozeshah Road, New Delhi - 110 001 © ICHR & Ministry of Culture, GoI No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. ISBN 978-81-938176-1-2 Printed in India by MANAK PUBLICATIONS PVT. LTD B-7, Saraswati Complex, Subhash Chowk, Laxmi Nagar, New Delhi 110092 INDIA Phone: 22453894, 22042529 [email protected] State Co-ordinators and their Researchers Andhra Pradesh & Telangana Karnataka (Co-ordinator) (Co-ordinator) V. Ramakrishna B. Surendra Rao S.K. Aruni Research Assistants Research Assistants V. Ramakrishna Reddy A.B. Vaggar I. Sudarshan Rao Ravindranath B.Venkataiah Tamil Nadu Kerala (Co-ordinator) (Co-ordinator) N. -

Wade Histoid Leprosy: Histological and Immunohistochemical Analysis
Lepr Rev (2013) 84, 176–185 Wade histoid Leprosy: histological and immunohistochemical analysis DANIELA A.M. DA COSTA*, MI´LVIA M.S.S. ENOKIHARA**, SUELY NONOGAKI***, SOLANGE M. MAEDA****, ADRIANA M. PORRO**** & JANE TOMIMORI**** *Medical resident, Escola Paulista de Medicina/UNIFESP, Sa˜o Paulo, Brazil **Department of Pathology, Escola Paulista de Medicina/UNIFESP, Sa˜o Paulo, Brazil ***Pathology Center, Instituto Adolfo Lutz, Sa˜o Paulo, Brazil ****Department of Dermatology, Escola Paulista de Medicina/UNIFESP, Brazil Accepted for publication 1 October 2013 Summary Histoid leprosy is a rare multibacillary form that presents with disseminated papule-nodular cutaneous lesions. To study the inflammatory infiltrate of the histoid form and to compare it with other lepromatous forms, we performed histological and immunohistochemical analysis on skin biopsies. Fifteen patients were included for histopathological analysis (10 histoid and five lepromatous) via the haematoxylin-eosin and Ziehl-Neelsen-Faraco stains. Thus, immunohistochemical techniques using immunoperoxidase assay were performed for: anti-BCG, anti-M. leprae, anti-CD8, anti-CD3, anti-CD20, anti-S100, anti-CD1a, anti-CD68 and anti- vimentin. Spindle cells were present in all histoid patients. A pseudocapsule was observed in half of both studied forms. A comparison using the Ziehl-Neelsen-Faraco stain to evaluate anti-BCG and anti-M.leprae showed no major differences. The CD3þ cells were more pronounced in the histoid form than the lepromatous form. There was greater immunoreactivity toward CD8þ cells in the histoid form, as well as the CD20þ cell count. A similar count of S100þ cells in the epidermis of both leprosy forms was observed. There was a slight increase of dendritic cells in the histoid patients in the superficial and deep dermis. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -
WR-CAPF-2019-Namelist-Engl.Pdf
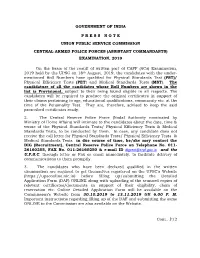
GOVERNMENT OF INDIA P R E S S N O T E UNION PUBLIC SERVICE COMMISSION CENTRAL ARMED POLICE FORCES (ASSISTANT COMMANDANTS) EXAMINATION, 2019 On the basis of the result of written part of CAPF (ACs) Examination, 2019 held by the UPSC on 18th August, 2019, the candidates with the under- mentioned Roll Numbers have qualified for Physical Standards Test (PST)/ Physical Efficiency Tests (PET) and Medical Standards Tests (MST). The candidature of all the candidates whose Roll Numbers are shown in the list is Provisional, subject to their being found eligible in all respects. The candidates will be required to produce the original certificates in support of their claims pertaining to age, educational qualifications, community etc. at the time of the Personality Test. They are, therefore, advised to keep the said prescribed certificates ready. 2. The Central Reserve Police Force (Nodal Authority nominated by Ministry of Home Affairs) will intimate to the candidates about the date, time & venue of the Physical Standards Tests/ Physical Efficiency Tests & Medical Standards Tests, to be conducted by them. In case, any candidate does not receive the call letter for Physical Standards Tests/ Physical Efficiency Tests & Medical Standards Tests in due course of time, he/she may contact the DIG (Recruitment), Central Reserve Police Force on Telephone No. 011- 26160255, FAX No. 011-26160250 & e-mail ID [email protected] and the U.P.S.C. through letter or Fax or email immediately, to facilitate delivery of communications to them promptly. 3. The candidates who have been declared qualified in the written examination are required to get themselves registered on the UPSC’s Website (https://upsconline.nic.in) before filling up/submitting the Detailed Application Form (DAF) ONLINE along with uploading of the scanned copies of relevant certificates/documents in support of their eligibility, claim of reservation etc. -

Department of School Education, Government of Haryana List of High and Sr.Sec
Department of School Education, Government of Haryana List of High and Sr.Sec. Schools,Nuh, District Nuh S.No School Type Location Name of DDO Code 1. 868 GSSS Ghasera Wajid Hussain 2. 869 GSSS Chhapera Dheeraj Singh 3. 882 GSSS Indri Mahender Singh 4. 6625 GSSS Nuh Deen Mohd. 5. 804 GSSS Malab Hasan Mohd 6. 705 GSSS Kairaka Changej Khan 7. 802 GSSS Akera Sunil Kumar 8. 706 GSSS Adbar Khalil Ahmed 9. 707 GSSS Sangail Virender 10. 795 GHS Alduka Urmil 11. 796 GSSS Feroz Pur Namak Sudesh Kumar 12. 797 GHS Ujina Jitender Kumar 13. 798 GGSSS Ujina Narender 14. 800 GGSSS Nuh Saddik Ahmed 15. 6055 GSSS Kamarsika Shyam Kumar 16. 801 GHS Meoli Om Parkash 17. 803 GHS Kurthala Raman 18. 808 GSSS Atta Barota Surender Kumar 19. 915 GSSS Gangoli Jahawar Dagar 20. 916 GHS Khera Khalilpur Dharambir 21. 918 GHS Bhiravati Surender 22. 6048 GHS Kotla Ajit Singh 23. 5869 GHS Alawalpur Nawab Khan 24. 814 GSSS Khor Basai Ramesh Kumar 25. 6060 GHS B.B. Pur Vidya Sagart 26. 713 GHS Manuwas Chokh Ram 27. 6031 GHS Tapkan Deepak 28. 948 GSSS Kherla Satvir Kundu 29. 815 GSSS Rewason Desh Raj 30. 6523 GGSSS Ghasera Satish Kumar 31. F.P.Jhirka 818 GSSS Agon Arun Kumar 9728456645 32. 875 GGSSS F.P.Jhirka Inderjeet Singh majoka 9050113597 33. 884 GSSS Ferozpur Jhirka Vishnu Kumar 9971394231 34. 871 GSSS Sakrash Aalamdeen 9416124398 35. 6088 GSSS Raniyala Satish kumar 9896661977 36. 881 GSSS Baded Anil Gautam 9466054202 37. 819 GSSS Biwan Lal Khan 9991507489 38. -

Histopathological Study of Granulomatous Dermatoses - a 2 Year Study at a Tertiary Hospital
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Histopathological Study of Granulomatous Dermatoses - A 2 Year Study at a Tertiary Hospital Velpula Nagesh Kumar1*, Kotta. Devender Reddy2**, N Ezhil Arasi3** 1Tutor, 2Associate Professor, 3Professor & Head, *Department of Pathology, Rajiv Gandhi Institute of Medical Sciences (RIMS), Govt. Medical Collage, Kadapa, Andhra Pradesh. **Department of Pathology, Osmania Medical Collage, Hyderabad, Telangana. Corresponding Author: Velpula Nagesh Kumar Received: 14/07/2016 Revised: 10/08/2016 Accepted: 11/08/2016 ABSTRACT Granulomatous inflammation is a type of chronic inflammation that has distinctive pattern of presentation with wide etiology and can involve any organ. Pathologists come across this lesion frequently and through knowledge of granulomatous lesions are very much essential to discriminate them from other lesions in the skin as they closely mimic each other. The aim of the present study is know the types of dermal granulomas, their prevalence, age and sex distribution, modes of presentation and histopathological spectrum. This prospective study was undertaken at Osmania General Hospital, Hyderabad from June 2012 to May 2014. A total of 620 skin biopsies were received at the Department of Pathology, histopathological sections of all the cases were critically analyzed and were classified on a “pattern based” approach according to Rabinowitz and Zaim et al. 172 cases were categorized histopathologically as granulomatous dermatoses. Granulomatous dermatoses were more common in males and the peak age of incidence was in 3rd decade. Incidence of Granulomatous dermatoses was 27.7% which was comparable with available literature. In the present study we found that Infections form an important cause of granulomatous dermatoses with majority of cases being leprosy followed by cutaneous tuberculosis and foreign body granulomas. -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Wade histoid leprosy revisited Permalink https://escholarship.org/uc/item/5d78t619 Journal Dermatology Online Journal, 22(2) Authors Coelho de Sousa, Virginia Laureano, Andre Cardoso, Jorge Publication Date 2016 DOI 10.5070/D3222030092 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 22 Number 1 February 2016 Case presentation Wade histoid leprosy revisited Virgínia Coelho de Sousa, André Laureano, Jorge Cardoso Dermatology Online Journal 22 (2): 8 Department of Dermatology and Venereology, Hospital de Santo António dos Capuchos – Centro Hospitalar de Lisboa Central, Lisboa, Portugal Correspondence: Virgínia Coelho de Sousa, MD Hospital de Santo António dos Capuchos – Centro Hospitalar de Lisboa Central, Lisboa, Portugal Alameda Santo António dos Capuchos, 1169-050 Lisboa, Portugal [email protected] +351926826029 Abstract An 18-year-old man presented with a 4-year history of erythematous patches on the trunk, followed 2-years later by multiple nodules, mostly located on the limbs, and distal paresthesias. Two close contacts were treated for leprosy during his childhood. Histopathological examination revealed a histiocytic infiltrate with acid-fast bacilli on Ziehl-Neelsen stain. The slit-skin and nasal smears showed numerous acid-fast bacilli. The correlation between clinical, epidemiological, histopathological, and microbiological features allowed the diagnosis of lepromatous leprosy, histoid variant. Multidrug therapy as recommended by the WHO was initiated. A rapid and sustained improvement was seen. Histoid leprosy is a rare manifestation of lepromatous leprosy, first described by Wade in 1960. Since then few cases have been reported, the majority of them from countries with a high prevalence of the disease.