Movement Disorders Are Listed in Table 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physiology of Basal Ganglia Disorders: an Overview
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES SILVERSIDES LECTURE Physiology of Basal Ganglia Disorders: An Overview Mark Hallett ABSTRACT: The pathophysiology of the movement disorders arising from basal ganglia disorders has been uncer tain, in part because of a lack of a good theory of how the basal ganglia contribute to normal voluntary movement. An hypothesis for basal ganglia function is proposed here based on recent advances in anatomy and physiology. Briefly, the model proposes that the purpose of the basal ganglia circuits is to select and inhibit specific motor synergies to carry out a desired action. The direct pathway is to select and the indirect pathway is to inhibit these synergies. The clinical and physiological features of Parkinson's disease, L-DOPA dyskinesias, Huntington's disease, dystonia and tic are reviewed. An explanation of these features is put forward based upon the model. RESUME: La physiologie des affections du noyau lenticulaire, du noyau caude, de I'avant-mur et du noyau amygdalien. La pathophysiologie des desordres du mouvement resultant d'affections du noyau lenticulaire, du noyau caude, de l'avant-mur et du noyau amygdalien est demeuree incertaine, en partie parce qu'il n'existe pas de bonne theorie expliquant le role de ces structures anatomiques dans le controle du mouvement volontaire normal. Nous proposons ici une hypothese sur leur fonction basee sur des progres recents en anatomie et en physiologie. En resume, le modele pro pose que leurs circuits ont pour fonction de selectionner et d'inhiber des synergies motrices specifiques pour ex£cuter Taction desiree. La voie directe est de selectionner et la voie indirecte est d'inhiber ces synergies. -

Clinical Rating Scale for Pantothenate Kinase-Associated Neurodegeneration: a Pilot Study
RESEARCH ARTICLE Clinical Rating Scale for Pantothenate Kinase-Associated Neurodegeneration: A Pilot Study Alejandra Darling, MD,1 Cristina Tello, PhD,2 Marı´a Josep Martı´, MD, PhD,3 Cristina Garrido, MD,4 Sergio Aguilera-Albesa, MD, PhD,5 Miguel Tomas Vila, MD,6 Itziar Gaston, MD,7 Marcos Madruga, MD,8 Luis Gonzalez Gutierrez, MD,9 Julio Ramos Lizana, MD,10 Montserrat Pujol, MD,11 Tania Gavilan Iglesias, MD,12 Kylee Tustin,13 Jean Pierre Lin, MD, PhD,13 Giovanna Zorzi, MD, PhD,14 Nardo Nardocci, MD, PhD,14 Loreto Martorell, PhD,15 Gustavo Lorenzo Sanz, MD,16 Fuencisla Gutierrez, MD,17 Pedro J. Garcı´a, MD,18 Lidia Vela, MD,19 Carlos Hernandez Lahoz, MD,20 Juan Darı´o Ortigoza Escobar, MD,1 Laura Martı´ Sanchez, 1 Fradique Moreira, MD ,21 Miguel Coelho, MD,22 Leonor Correia Guedes,23 Ana Castro Caldas, MD,24 Joaquim Ferreira, MD,22,23 Paula Pires, MD,24 Cristina Costa, MD,25 Paulo Rego, MD,26 Marina Magalhaes,~ MD,27 Marı´a Stamelou, MD,28,29 Daniel Cuadras Palleja, MD,30 Carmen Rodrı´guez-Blazquez, PhD,31 Pablo Martı´nez-Martı´n, MD, PhD,31 Vincenzo Lupo, PhD,2 Leonidas Stefanis, MD,28 Roser Pons, MD,32 Carmen Espinos, PhD,2 Teresa Temudo, MD, PhD,4 and Belen Perez Duenas,~ MD, PhD1,33* 1Unit of Pediatric Movement Disorders, Hospital Sant Joan de Deu, Barcelona, Spain 2Unit of Genetics and Genomics of Neuromuscular and Neurodegenerative Disorders, Centro de Investigacion Prı´ncipe Felipe, Valencia, Spain 3Neurology Department, Hospital Clı´nic de Barcelona, Institut d’Investigacions Biomediques IDIBAPS. -

Pathophysiology of Dysarthria in Cerebral Palsy
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.44.11.1013 on 1 November 1981. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1981 ;44:1013-1019 Pathophysiology of dysarthria in cerebral palsy PETER D NEILSON, NICHOLAS J O'DWYER From The Spastic Centre Research Unit, Department of Neurology, The Prince Henry Hospital and School of Medicine, University of New South Wales SUMMARY Electromyograms were recorded with hooked-wire electrodes from sixteen lip, tongue and jaw muscles in six normal and seven cerebral palsied adult subjects during a variety of speech and non-speech tasks. The recorded patterns of muscle activity fail to support a number of theories concerning the pathophysiology of dysarthria in cerebral palsy. There was no indication of weakness in individual articulator muscles. There was no evidence of uncontrolled sustained background activity or of abnormal tonic stretch reflex responses in lip or tongue muscles. Primitive or patho- logical reflexes could not be elicited by orofacial stimulation. No imbalance between positive and negative oral responses was observed. The view that random involuntary movement disrupts essentially normal voluntary control in athetosis was not supported. Each cerebral palsied subject displayed an idiosyncratic pattern of abnormal muscle activity which was reproduced across repeti- guest. Protected by copyright. tions of the same phrase, indicating a consistent defect in motor programming. There has been little experimental verification of disruption of the voluntary control of speech muscles existing theories concerning the pathophysiology of by random involuntary activity of the type associated dysarthria in cerebral palsy. The present study with athetosis.6 12 15 provides electromyographic (EMG) data in the light EMG studies of the speech musculature in cerebral of which these theories can be examined. -

Radiologic-Clinical Correlation Hemiballismus
Radiologic-Clinical Correlation Hemiballismus James M. Provenzale and Michael A. Schwarzschild From the Departments of Radiology (J.M.P.), Duke University Medical Center, Durham, and f'leurology (M.A.S.), Massachusetts General Hospital, Boston Clinical History derived from the Greek word meaning "to A 65-year-old recently retired surgeon in throw," because the typical involuntary good health developed disinhibited behavior movements of the affected limbs resemble over the course of a few months, followed by the motions of throwing ( 1) . Such move onset of unintentional, forceful flinging move ments usually involve one side of the body ments of his right arm and leg. Magnetic res (hemiballismus) but may involve one ex onance imaging demonstrated a 1-cm rim tremity (monoballism), both legs (parabal enhancing mass in the left subthalamic lism), or all the extremities (biballism) (2, 3). region, which was of high signal intensity on The motions are centered around the shoul T2-weighted images (Figs 1A-E). Positive der and hip joints and have a forceful, flinging serum human immunodeficiency virus anti quality. Usually either the arm or the leg is gen and antibody titers were found, with predominantly involved. Although at least mildly elevated cerebrospinal fluid toxo some volitional control over the affected plasma titers. Anti-toxoplasmosis treatment limbs is still maintained, the involuntary with sulfadiazine and pyrimethamine was be movements typically can be checked by the gun, with resolution of the hemiballistic patient for only a few moments ( 1). The movements within a few weeks and decrease movements are usually continuous but may in size of the lesion. -
Movement Disorders Program & the Murray Center for Research on Parkinson's Disease & Related Disorders
Movement Disorders Medical University of South Carolina MUSC Health Movement DisordersMovement Disorders Program Program Program & The Murray 96 Jonathan Lucas Street, and the Murray Center for Research on Parkinson’sSuite Disease 301 CSB, MSC and 606 Related Disorders Center for Research on Charleston, SC 29425 Parkinson’s Disease & Related Disorders muschealth.org 843-792-3221 Changing What’s Possible “Our focus is providing patients with the best care possible, from treatment options to the latest technology and research. We have an amazing team of experts that provides compassionate care to each individual that we see.” — Dr. Vanessa Hinson Getting help from the MUSC Health Movement Disorders Program Millions of Americans suffer from movement disorders. These are typically characterized by involuntary movements, shaking, slowness of movement, or uncontrollable muscle contractions. As a result, day to day activities like walking, dressing, dining, or writing can become challenging. The MUSC Health Movement Disorders Program offers a comprehensive range of services, from diagnostic testing and innovative treatments to rehabilitation and follow-up support. Our team understands that Parkinson’s disease and other movement disorders can significantly impact quality of life. Our goal is to provide you and your family continuity of care with empathy and compassion throughout the treatment experience. Please use this guide to learn more about Diseases Treated – information about the disorders and symptoms you might feel Specialty Procedures – treatments that show significant improvement for many patients Research – opportunities to participate in clinical trials at the MUSC Health Movement Disorders Program Profiles – MUSC Health movement disorder specialists We are dedicated to finding the cure for disabling movement disorders and to help bring about new treatments that can improve our patients’ lives. -

Cerebral Palsy
Cerebral Palsy Cerebral palsy encompasses a group of non-progressive and non-contagious motor conditions that cause physical disability in various facets of body movement. Cerebral palsy is one of the most common crippling conditions of childhood, dating to events and brain injury before, during or soon after birth. Cerebral palsy is a debilitating condition in which the developing brain is irreversibly damaged, resulting in loss of motor function and sometimes also cognitive function. Despite the large increase in medical intervention during pregnancy and childbirth, the incidence of cerebral palsy has remained relatively stable for the last 60 years. In Australia, a baby is born with cerebral palsy about every 15 hours, equivalent to 1 in 400 births. Presently, there is no cure for cerebral palsy. Classification Cerebral palsy is divided into four major classifications to describe different movement impairments. Movements can be uncontrolled or unpredictable, muscles can be stiff or tight and in some cases people have shaky movements or tremors. These classifications also reflect the areas of the brain that are damaged. The four major classifications are: spastic, ataxic, athetoid/dyskinetic and mixed. In most cases of cerebral palsy, the exact cause is unknown. Suggested possible causes include developmental abnormalities of the brain, brain injury to the fetus caused by low oxygen levels (asphyxia) or poor circulation, preterm birth, infection, and trauma. Spastic cerebral palsy leads to increased muscle tone and inability for muscles to relax (hypertonic). The brain injury usually stems from upper motor neuron in the brain. Spastic cerebral palsy is classified depending on the region of the body affected; these include: spastic hemiplegia; one side being affected, spastic monoplegia; a single limb being affected, spastic triplegia; three limbs being affected, spastic quadriplegia; all four limbs more or less equally affected. -

Hunting Down a Case of Progressive Movement Disorder, Dementia, and Genetic Anticipation – a Case Report on Huntington’S Disease
Madhavi et al (2020): r A case report of Huntington’s disease Nov 2020 Vol. 23 Issue 21 HUNTING DOWN A CASE OF PROGRESSIVE MOVEMENT DISORDER, DEMENTIA, AND GENETIC ANTICIPATION – A CASE REPORT ON HUNTINGTON’S DISEASE 1*Dr. K.Vani Madhavi, 2Dr. Anand Acharya, 3Dr Vijaya Vishnu 1,3Department of SPM, 2Department of Pharmacology , 1,2,3Konaseema Institute of medical Sciences Research Foundation, Amalapuram, Andhra Pradesh, India *corresponding author: 1Dr. K.Vani Madhavi E-Mail: [email protected] Abstract The Huntington Disease HD is a progressive, fatal, highly penetrant autosomal dominant disease considered by involuntary choreiform movements. A developing number of reformists generative conditions mirror the introduction of Huntington's ailment (HD). Separating between these HD-like conditions is vital once a patient by blend of development problems, psychological decrease, social irregularities and infection course demonstrates negative to the hereditary testing for HD causative transformations, that is, IT15 quality trinucleotide-rehash extension. The disparity finding of HD-like conditions is intricate and might prompt superfluous and exorbitant examinations. We suggest guidelines for this differential determination zeroing in on a predetermined number of clinical highlights ('warnings') that can be distinguished over precise clinical assessment, assortment of recorded information and a couple of routine auxiliary examinations. Present highlights incorporate the traditional foundation of the patient, the contribution of the facio-bucco-lingual and cervical region with development problem, the co-event of cerebellar highlights and seizures, the occurrence of exceptional stride examples and eye development irregularities, and an atypical movement of ailment. Extra assistance may get from the intellectual social introduction of the patient, just as by a limited amount of subordinate examinations, chiefly MRI and routine blood tests. -

Anatomical, Biological, and Surgical Features of Basal Gangliaanatomical, Biological, and Surgical Features of Basal Ganglia
DOI: 10.5772/intechopen.68851 Provisional chapter Chapter 7 Anatomical, Biological, and Surgical Features of Basal Anatomical,Ganglia Biological, and Surgical Features of Basal Ganglia Nuket Gocmen Mas, Harun Muayad Said, NuketMurat GocmenTosun, Nilufer Mas, HarunYonguc, Muayad Yasemin Said, Soysal Muratand Hamit Tosun, Selim Nilufer Karabekir Yonguc, Yasemin Soysal and HamitAdditional Selim information Karabekir is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.68851 Abstract Basal ganglia refers to the deep gray matter masses on the deeply telencephalon and encompasses a group of nuclei and it influence the information in the extrapyramidal system. In human they are related with numerous significant functions controlled by the nervous system. Gross anatomically, it is comprised of different parts as the dorsal stria- tum that are consisted of the caudate nucleus and putamen and ventral striatum which includes the nucleus accumbens, olfactory tubercle, globus pallidus, substantia nigra, and subthalamic nucleus. Nucleus accumbens, is also associated with reward circuits and has two parts; the nucleus accumbens core and the nucleus accumbens shell. Neurological diseases are characterized through the obvious pathology of the basal ganglia, and there are important findings explaining striatal neurodegeneration on human brain. Some of these diseases are induced by bacterial and/or viral infections. Surgical interference can be one alternative for neuronal disease treatment like Parkinson’s Disease or Thiamine Responsive Basal Ganglia Disease or Wilson’s Disease, respectively in addition to the vas- cular or tumor surgery within this area. Extensive knowledge on the morphological basis of diseases of the basal ganglia along with motor, behavioral and cognitive symptoms can contribute significantly to the optimization of the diagnosis and later patient’s treatment. -

Part Ii – Neurological Disorders
Part ii – Neurological Disorders CHAPTER 14 MOVEMENT DISORDERS AND MOTOR NEURONE DISEASE Dr William P. Howlett 2012 Kilimanjaro Christian Medical Centre, Moshi, Kilimanjaro, Tanzania BRIC 2012 University of Bergen PO Box 7800 NO-5020 Bergen Norway NEUROLOGY IN AFRICA William Howlett Illustrations: Ellinor Moldeklev Hoff, Department of Photos and Drawings, UiB Cover: Tor Vegard Tobiassen Layout: Christian Bakke, Division of Communication, University of Bergen E JØM RKE IL T M 2 Printed by Bodoni, Bergen, Norway 4 9 1 9 6 Trykksak Copyright © 2012 William Howlett NEUROLOGY IN AFRICA is freely available to download at Bergen Open Research Archive (https://bora.uib.no) www.uib.no/cih/en/resources/neurology-in-africa ISBN 978-82-7453-085-0 Notice/Disclaimer This publication is intended to give accurate information with regard to the subject matter covered. However medical knowledge is constantly changing and information may alter. It is the responsibility of the practitioner to determine the best treatment for the patient and readers are therefore obliged to check and verify information contained within the book. This recommendation is most important with regard to drugs used, their dose, route and duration of administration, indications and contraindications and side effects. The author and the publisher waive any and all liability for damages, injury or death to persons or property incurred, directly or indirectly by this publication. CONTENTS MOVEMENT DISORDERS AND MOTOR NEURONE DISEASE 329 PARKINSON’S DISEASE (PD) � � � � � � � � � � � -
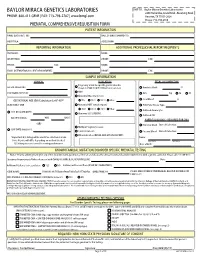
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Reliability of MRI in Detection and Differentiation of Acute Neonatal/Pediatric Encephalopathy Causes Among Neonatal/ Pediatric Intensive Care Unit Patients Tamir A
Hassan and Mohey Egyptian Journal of Radiology and Nuclear Medicine Egyptian Journal of Radiology (2020) 51:62 https://doi.org/10.1186/s43055-020-00173-7 and Nuclear Medicine RESEARCH Open Access Reliability of MRI in detection and differentiation of acute neonatal/pediatric encephalopathy causes among neonatal/ pediatric intensive care unit patients Tamir A. Hassan* and Nesreen Mohey Abstract Background: Causes of encephalopathy in neonates/pediatrics include hypoxic-ischemic injury (which is the most frequent cause and is defined as any impairment to the brain caused by insufficient blood flow and oxygenation), trauma, metabolic disorders, and congenital and infectious diseases. The aim of this study is to evaluate the value of MRI in detection and possible differentiation of different non-traumatic, non-infectious causes of acute neonatal/ pediatric encephalopathy among NICU/PICU patients. Results: This retrospective study included 60 selected patients according to the study inclusion and exclusion criteria; all presented with positive MRI findings for non-traumatic, non-infectious acute brain injury. Females (32, 53.3%) were affected more than males (28, 46.7%) with a mean age of 1.1 ± 1.02 years; all presented with variable neurological symptoms and signs that necessitate neonatal intensive care unit/pediatric intensive care unit (NICU/ PICU) admission. The final diagnosis of the study group patients were hypoxic ischemia injury (HII) in 39 patients (65%), metachromatic leukodystrophy in 6 patients (10%), biotin-thiamine-responsive basal ganglia disease (BTBGD) and Leigh disease each in 4 patients (6.7%), periventricular leukomalacia (PVL) in 3 patients (5%), and mitochondrial encephalopathy with lactic acidosis and stroke-like episodes syndrome (MELAS) and non-ketotic hyperglycinemia (NKH) each in 2 patients (3.3%). -

Para/Post Infectious Recovering Encephalitis with Localized Basal
INDIAN PEDIATRICS VOLUME 34-AUGUST 1997 Para/Post Infectious Recovering sity lesions of the caudate and putamen in Encephalitis with Localized Basal 3 (Fig. 1), of the gl6bus pallidus in 1, and Ganglia Involvement thalamus and mid brain in one. MRI was done in 7 children, including the 3 with normal CT scans, and showed increased V.P. Udani signal intensity on T2 weighted images in V.R. Dharnidharka the caudate and putamen (Fig. 2) in all ex- A.R. Gajendragadkar cept one. Involvement was bilateral in 5 and unilateral in one. One child had a CT Neurological dysfunction in children done at the time of illness which was ab- associated with bilateral hypodense lesions normal and then recovered to such an ex- of the basal ganglia is seen in disorders like tent that her MRI after 1 year was totally Huntington's chorea, Wilson's disease, normal. Two illustrative cases are de- Hallervorden Spatz syndrome, Leigh's dis- scribed below. ease, infantile striatal necrosis, hypoxia, ischemia and various intoxications(l). Case 1: A 10-year-old male child was re- Goutieres and Aicardi described in 1982 a ferred from another city with a history of new neuroradiological syndrome charac- febrile illness 1 month earlier, during terized by a rapid clinical onset of striatal which he developed alterations in sensori- symptoms following an infectious illness, um, became unconscious and developed associated with similar hypodense basal weakness in all 4 limbs. He slowly im- ganglia lesions, but with a far better out- proved in consciousness but remained come than seen with the conditions men- quadriplegic.