Congestive Heart Failure Coding & Documentation Guide, February 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ischemic Cardiomyopathy: Symptoms, Causes, & Treatment
Ischemic Cardiomyopathy Ischemic cardiomyopathy is a condition that occurs when the heart muscle is weakened due to insufficient blood flow to the heart's muscle. This inhibits the heart's ability to pump blood and can lead to heart failure. What Is Ischemic Cardiomyopathy? Ischemic cardiomyopathy (IC) is a condition that occurs when the heart muscle is weakened. In this condition, the left ventricle, which is the main heart muscle, is usually enlarged and dilated. This condition can be a result of a heart attack or coronary artery disease, a narrowing of the arteries. These narrowed arteries keep blood from reaching portions of your heart. The weakened heart muscle inhibits your heart’s ability to pump blood and can lead to heart failure. Symptoms of IC include shortness of breath, chest pain, and extreme fatigue. If you have IC symptoms, you should seek medical care immediately. Treatment depends on how much damage has been done to your heart. Medications and surgery are often required. You can improve your long-term outlook by making certain lifestyle changes, such as maintaining a healthy diet and avoiding high-risk behaviors, including smoking. Symptoms of Ischemic Cardiomyopathy You can have early-stage heart disease with no symptoms. As the arteries narrow further and blood flow becomes impaired, you may experience a variety of symptoms, including: shortness of breath extreme fatigue dizziness, lightheadedness, or fainting chest pain and pressure (angina) heart palpitations weight gain swelling in the legs and feet (edema) and abdomen difficulty sleeping cough or congestion caused by fluid in the lungs If you have these symptoms, seek emergency medical care or call 9-1-1. -
ICD-10-CM Documentation and Coding Best Practices
ICD-10-CM Documentation and Coding Best Practices Cardiomyopathy Cardiomyopathy refers to diseases of the heart muscle, which can become enlarged, thick or rigid. In rare cases, cardiac muscle tissue can be replaced with scar tissue. As the condition worsens, the heart becomes weaker and less able to pump blood through the body or to maintain a normal electrical rhythm. Causes Risk factors that can increase the possibility of developing cardiomyopathy include: coronary artery disease, a history of heart attack (s), viral infections that cause heart inflammation, long-term hypertension or alcoholism, obesity, and diabetes to name a few. However, in most cases the exact cause is usually unknown (called primary or idiopathic cardiomyopathy). Symptoms Some patients will never have symptoms; others will not develop them until later in the disease. Symptoms can include: • Fatigue • Shortness of b reath or trouble breathing (dyspnea) • Dizziness, lightheadedness or fainting • Swelling in the ankles, feet, legs, abdomen and neck veins Treatment Treatment depends on the type of cardiomyopathy, the severity of symptoms, and the patient’s age and overall health. • Lifestyle changes can help manage condition(s) that may be causing cardiomyopathy. Recommendations include: o Consuming a heart healthy diet, engaging in physical activity, losing excess weight, giving up smoking, avoiding alcohol and illegal drugs, getting enough sleep, and reducing stress • Medicines may be p rescribed to: o Lower blood pressure (ACE inhibitors, angiotensin II receptor blo ckers, beta blockers, calcium channel blockers ) o Slow the heart rate (beta blockers, calcium channel blockers, digoxin) o Prevent arrhythmias (antiarrhythmics) o Remove excess fluid and sodium (diuretics) o Prevent blood clots (anticoagulants) • Alcohol septal ablation • Surgery o Septal myectomy – option for severe cases of obstructive hypertrophic cardiomyopathy Surgically implanted devices o . -

The Pulmonary Manifestations of Left Heart Failure*
The Pulmonary Manifestations of Left Heart Failure* Brian K. Gehlbach, MD; and Eugene Geppert, MD Determining whether a patient’s symptoms are the result of heart or lung disease requires an understanding of the influence of pulmonary venous hypertension on lung function. Herein, we describe the effects of acute and chronic elevations of pulmonary venous pressure on the mechanical and gas-exchanging properties of the lung. The mechanisms responsible for various symptoms of congestive heart failure are described, and the significance of sleep-disordered breathing in patients with heart disease is considered. While the initial clinical evaluation of patients with dyspnea is imprecise, measurement of B-type natriuretic peptide levels may prove useful in this setting. (CHEST 2004; 125:669–682) Key words: Cheyne-Stokes respiration; congestive heart failure; differential diagnosis; dyspnea; pulmonary edema; respiratory function tests; sleep apnea syndromes Abbreviations: CHF ϭ congestive heart failure; CSR-CSA ϭ Cheyne-Stokes respiration with central sleep apnea; CPAP ϭ continuous positive airway pressure; Dlco ϭ diffusing capacity of the lung for carbon monoxide; DM ϭ membrane conductance; FRC ϭ functional residual capacity; OSA ϭ obstructive sleep apnea; TLC ϭ total lung ϭ ˙ ˙ ϭ capacity; VC capillary volume; Ve/Vco2 ventilatory equivalent for carbon dioxide early 5 million Americans have congestive heart For a detailed review of the pathophysiology of N failure (CHF), with 400,000 new cases diag- high-pressure pulmonary edema, the reader is re- nosed each year.1 Unfortunately, despite the consid- ferred to several excellent recent reviews.2–4 erable progress that has been made in understanding the pathophysiology of pulmonary edema, the pul- monary complications of this condition continue to The Pathophysiology of Pulmonary challenge the bedside clinician. -

Ischemic Mitral Regurgitation: a Multifaceted Syndrome with Evolving Therapies
biomedicines Review Ischemic Mitral Regurgitation: A Multifaceted Syndrome with Evolving Therapies Mattia Vinciguerra 1,* , Francesco Grigioni 2, Silvia Romiti 1 , Giovanni Benfari 3,4, David Rose 5 , Cristiano Spadaccio 5,6, Sara Cimino 1, Antonio De Bellis 7 and Ernesto Greco 1 1 Department of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, 00161 Rome, Italy; [email protected] (S.R.); [email protected] (S.C.); [email protected] (E.G.) 2 Unit of Cardiovascular Sciences, Department of Medicine Campus Bio-Medico, University of Rome, 00128 Rome, Italy; [email protected] 3 Division of Cardiology, Department of Medicine, University of Verona, 37219 Verona, Italy; [email protected] 4 Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN 55905, USA 5 Lancashire Cardiac Centre, Blackpool Victoria Hospital, Blackpool FY3 8NP, UK; [email protected] (D.R.); [email protected] (C.S.) 6 Institute of Cardiovascular and Medical Sciences, University of Glasgow, Glasgow G12 8QQ, UK 7 Department of Cardiology and Cardiac Surgery, Casa di Cura “S. Michele”, 81024 Maddaloni, Caserta, Italy; [email protected] * Correspondence: [email protected] Abstract: Dysfunction of the left ventricle (LV) with impaired contractility following chronic ischemia or acute myocardial infarction (AMI) is the main cause of ischemic mitral regurgitation (IMR), leading to moderate and moderate-to-severe mitral regurgitation (MR). The site of AMI exerts a specific Citation: Vinciguerra, M.; Grigioni, influence determining different patterns of adverse LV remodeling. In general, inferior-posterior F.; Romiti, S.; Benfari, G.; Rose, D.; AMI is more frequently associated with regional structural changes than the anterolateral one, which Spadaccio, C.; Cimino, S.; De Bellis, is associated with global adverse LV remodeling, ultimately leading to different phenotypes of IMR. -

Ischemic Cardiomyopathy: Contemporary Clinical Management
Chapter 7 Ischemic Cardiomyopathy: Contemporary Clinical Management BurhanBurhan Sheikh Alkar, Sheikh Alkar, Gustav MattssonGustav Mattsson and PeterPeter Magnusson Magnusson Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.76723 Abstract Ischemic cardiomyopathy, disease of the heart muscle due to coronary artery disease, is the most common cardiomyopathy. It is often difficult to discern the etiology of heart failure, and often there are multiple underlying causes. Ischemic cardiomyopathy most often pres - ents with a dilated morphology with wall motion defects and a history of previous myocar - dial infarction or confirmed coronary artery disease. Mechanisms of myocardial depression in ischemia are necrosis of myocardial cells resulting in irreversible loss of function or reversible damage, either short term through myocardial stunning or long term through hibernation. In ischemic cardiomyopathy, echocardiography may be extended with stress testing or other imaging modalities such as myocardial scintigraphy and cardiac magnetic resonance tomography. Coronary angiography is often considered a gold standard; how - ever, other modalities such as positron emission tomography can be needed to detect small vessel disease. Cardiac revascularization, through percutaneous coronary intervention and coronary artery bypass grafting, both in acute coronary syndrome and in stable coronary artery disease, relieves symptoms and improves prognosis. Therapy should aspire to treat ischemia, arrhythmias in addition to heart failure management, which includes device therapy with cardiac resynchronization therapy, implantable cardioverter defibrillators, and mechanical support as bridging or destination therapy in end-stage disease. Keywords: cardiomyopathy, coronary artery disease, heart failure, ischemic, myocardial infarction 1. Introduction Disease of the heart muscle, cardiomyopathy, appears in various disease manifestations, which are often either poorly defined or difficult to distinguish in clinical practice. -

Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting
Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting Steven R Bailey MD MSCAI, FACC, FAHA,FACP Professor and Chair, Department of Medicine Malcolm Feist Chair of Interventional Cardiology LSU Health Shreveport Professor Emeritus, UH Health San Antonio [email protected] SRB March 2020 Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company • Grant/Research Support • None • Consulting Fees/Honoraria • BSCI, Abbot DSMB • Intellectual Property Rights • UTHSCSA • Other Financial Benefit • CCI Editor In Chief SRB March 2020 The 30,000 Ft View Maria SRB March 2020 SRB March 2020 Mitral Stenosis • The most common etiology of MS is rheumatic fever, with a latency of approximately 10 to 20 years after the initial streptococcal infection. Symptoms usually appear in adulthood • Other etiologies are rare but include: congenital MS radiation exposure atrial myxoma mucopolysaccharidoses • MS secondary to calcific annular disease is increasingly seen in elderly patients, and in patients with advanced chronic kidney disease. SRB March 2020 Mitral Stenosis • Mitral stenosis most commonly results from rheumatic heart disease fusion of the valve leaflet cusps at the commissures thickening and shortening of the chordae calcium deposition within the valve leaflets • Characteristic “fish-mouth” or “hockey stick” appearance on the echocardiogram (depending on view) SRB March 2020 Mitral Stenosis: Natural History • The severity of symptoms depends primarily on the degree of stenosis. • Symptoms often go unrecognized by patient and physician until significant shortness of breath, hemoptysis, or atrial fibrillation develops. -
Currentstateofknowledgeonaetiol
European Heart Journal (2013) 34, 2636–2648 ESC REPORT doi:10.1093/eurheartj/eht210 Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Downloaded from Alida L. P. Caforio1†*, Sabine Pankuweit2†, Eloisa Arbustini3, Cristina Basso4, Juan Gimeno-Blanes5,StephanB.Felix6,MichaelFu7,TiinaHelio¨ 8, Stephane Heymans9, http://eurheartj.oxfordjournals.org/ Roland Jahns10,KarinKlingel11, Ales Linhart12, Bernhard Maisch2, William McKenna13, Jens Mogensen14, Yigal M. Pinto15,ArsenRistic16, Heinz-Peter Schultheiss17, Hubert Seggewiss18, Luigi Tavazzi19,GaetanoThiene4,AliYilmaz20, Philippe Charron21,andPerryM.Elliott13 1Division of Cardiology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 2Universita¨tsklinikum Gießen und Marburg GmbH, Standort Marburg, Klinik fu¨r Kardiologie, Marburg, Germany; 3Academic Hospital IRCCS Foundation Policlinico, San Matteo, Pavia, Italy; 4Cardiovascular Pathology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 5Servicio de Cardiologia, Hospital U. Virgen de Arrixaca Ctra. Murcia-Cartagena s/n, El Palmar, Spain; 6Medizinische Klinik B, University of Greifswald, Greifswald, Germany; 7Department of Medicine, Heart Failure Unit, Sahlgrenska Hospital, University of Go¨teborg, Go¨teborg, Sweden; 8Division of Cardiology, Helsinki University Central Hospital, Heart & Lung Centre, -

View Pdf Copy of Original Document
Phenotype definition for the Vanderbilt Genome-Electronic Records project Identifying genetics determinants of normal QRS duration (QRSd) Patient population: • Patients with DNA whose first electrocardiogram (ECG) is designated as “normal” and lacking an exclusion criteria. • For this study, case and control are drawn from the same population and analyzed via continuous trait analysis. The only difference will be the QRSd. Hypothetical timeline for a single patient: Notes: • The study ECG is the first normal ECG. • The “Mildly abnormal” ECG cannot be abnormal by presence of heart disease. It can have abnormal rate, be recorded in the presence of Na-channel blocking meds, etc. For instance, a HR >100 is OK but not a bundle branch block. • Y duration = from first entry in the electronic medical record (EMR) until one month following normal ECG • Z duration = most recent clinic visit or problem list (if present) to one week following the normal ECG. Labs values, though, must be +/- 48h from the ECG time Criteria to be included in the analysis: Criteria Source/Method “Normal” ECG must be: • QRSd between 65-120ms ECG calculations • ECG designed as “NORMAL” ECG classification • Heart Rate between 50-100 ECG calculations • ECG Impression must not contain Natural Language Processing (NLP) on evidence of heart disease concepts (see ECG impression. Will exclude all but list below) negated terms (e.g., exclude those with possible, probable, or asserted bundle branch blocks). Should also exclude normalization negations like “LBBB no longer present.” -
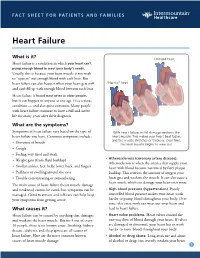
Heart Failure
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

Heart Disease and Diseases of the Circulatory System in Westchester
Westchester County 2016.01 Department of Health KEEP HEALTHY @wchealthdept AND Community Health Assessment Data Update GET #keephealthy THE STATS Heart Disease and Diseases of the Circulatory System in Westchester In this issue: Heart disease as a Heart disease is the number one cause of death in Westchester County. leading cause of death in Westchester county In 2012, heart disease accounted for 2,113 deaths or 31% of all deaths Deaths due to heart disease across different in the county. Adding in 490 deaths due to stroke and other diseases population and risk of the circulatory system, total deaths from circulatory disease are groups 60% higher than the next leading cause of death - cancer. Hospitalizations due to cardiovascular disease- related conditions, Selected Causes of Death in Westchester County, 2012 including diseases of the heart Emergency room visits 2% 3% 7% due to cardiovascular disease-related 3% conditions Selected risk factors 4% that contribute to Heart Disease, cardiovascular disease 4% in Westchester county 31% 5% 9% Cerebrovascular Jiali Li, Ph.D. Director of Disease (Stroke), Research & Evaluation Neoplasms 5% Planning & Evaluation (Cancer), 24% Other Circulatory, Renee Recchia, MPH 3% Acting Deputy Commissioner of Administration Heart Disease Cerebrovascular Disease (Stroke) Project Staff: Other Circulatory Neoplasms (Cancer) Bonnie Lam, MPH Respiratory Diseases External Causes (e.g. accidents) Medical Data Analyst Communicable Diseases Nervous System Diseases Milagros Venuti, MPA Digestive System Diseases -

Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: the First Report from Korea
Journal of Clinical Medicine Article Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: The First Report from Korea Ah Young Kim 1,2 , Jo Won Jung 1,2, Se Yong Jung 1,2 , Jae Il Shin 1,2 , Lucy Youngmin Eun 1,2 , Nam Kyun Kim 3 and Jae Young Choi 1,2,* 1 Division of Pediatric Cardiology, Center for Congenital Heart Disease, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul 03722, Korea; [email protected] (A.Y.K.); [email protected] (J.W.J.); [email protected] (S.Y.J.); [email protected] (J.I.S.); [email protected] (L.Y.E.) 2 Department of Pediatrics, Yonsei University College of Medicine, Seoul 03722, Korea 3 Department of Pediatrics, Emory University, Atlanta, GA 30322, USA; [email protected] * Correspondence: [email protected] Received: 25 July 2020; Accepted: 24 August 2020; Published: 26 August 2020 Abstract: Percutaneous pulmonary valve implantation (PPVI) is used to treat pulmonary stenosis (PS) or pulmonary regurgitation (PR). We described our experience with PPVI, specifically valve-in-valve transcatheter pulmonary valve replacement using the Melody valve and novel self-expandable systems using the Pulsta valve. We reviewed data from 42 patients undergoing PPVI. Twenty-nine patients had Melody valves in mostly bioprosthetic valves, valved conduits, and homografts in the pulmonary position. Following Melody valve implantation, the peak right ventricle-to-pulmonary artery gradient decreased from 51.3 11.5 to 16.7 3.3 mmHg and right ventricular systolic pressure ± ± fell from 70.0 16.8 to 41.3 17.8 mmHg. -

Cardiovascular Disease: a Costly Burden for America. Projections
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA PROJECTIONS THROUGH 2035 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american table of contents INTRODUCTION ...................................................................................5 ABOUT THIS STUDY ................................................................................................... 6 WHAT IS CVD? ......................................................................................................... 6 Atrial Fibrillation Congestive Heart Failure Coronary Heart Disease High Blood Pressure Stroke PROJECTIONS: PREVALENCE OF CVD .............................................................7 Latest Projections Age, Race, Sex – Differences That Matter PROJECTIONS: COSTS OF CVD ................................................................. 8-11 The Cost Generators: Aging Baby Boomers Medical Costs Breakdown Direct Costs + Indirect Costs RECOMMENDATIONS .............................................................................13-14 Research Prevention Affordable Health Care 3 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american Introduction Cardiovascular disease (CVD) has been the leading killer In addition, CVD has become our nation’s costliest chronic of Americans for decades. In years past, a heart attack disease. In 2014, stroke and heart