Curriculum Vitae Format
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

East Coast Top Prospects Added to the Non-Televised Undercard of Luis Ortiz Vs
EAST COAST TOP PROSPECTS ADDED TO THE NON-TELEVISED UNDERCARD OF LUIS ORTIZ VS. TONY THOMPSON FOR AN EXCITING NIGHT OF BOXING LIVE FROM THE DC ARMORY AT THE NATIONS CAPTIAL, WASHINGTON D.C. Tickets Start at $25! LOS ANGELES (Feb. 10) - The non-televised undercard of Luis Ortiz vs. Tony Thompson will feature exciting top prospects from the East Coast for an exciting night of boxing on March 5, live from the DC Armory. First off, undefeated lightweight, Lamont Roach Jr. (9-0, 3 KOs) of Washington, D.C. will participate in a six-round fight and new Golden Boy Promotions fighter Rashidi "Speedy" Ellis (14-0, 11 KO) from Lynn, Mass. will fight in an eight- round welterweight bout. Also on the card, D'Mitrius "Big Meech" Ballard (11-0,7 KOs) from Temple Hills, Md. is scheduled for a six-round middleweight brawl and stable mate Kevin "K-Smoove" Rivers (12-1, 9 KOs) is committed to a six-round featherweight battle. Two spectacular undefeated super lightweights, Zachary "Zungry" Ochoa (13-0, 6 KOs) of Brooklyn, N.Y. and Philly native Damon Allen (8-0, 3 KOs) will both fight in respective six-round bouts. Opening up the night, Todd Unthank-May (8-0, 3 KOs) also of Philadelphia, will fight in a six-round light heavyweights bout. Opponents will be announced shortly. The event on March 5, is headlined by the WBA Interim Heavyweight World Championship Title showdown between Luis "The Real King Kong" Ortiz (24-0, 21 KOs) and Tony "The Tiger" Thompson (40-6, 27 KO's). -

Check out My Resume
William D. Caballero is a Los Angeles-based creative leader capable of all aspects of digital multimedia production, including directing, producing, video editing, writing, sound design, and film scoring. His work features 3D printed protagonists, and his latest short film, Victor & Isolina, debuted at the 2017 Sundance Film Festival. He is also a 2018 Guggenheim Fellow. EXPERIENCE Caballero has created, directed, and edited over 500 digital videos and original series for a variety of networks. PBS/LATINO PUBLIC BROADCASTING, 2017-2018 Produced, wrote, and edited a web-series aimed at empowering diverse young people to tell their stories through creative arts and media. Funded by the Corporation for Public Broadcasting. HBO, 2015-2017 Produced, wrote, and edited an original series called “Gran’Pa Knows Best.” Over thirty episodes are viewable on HBO GO/NOW. UNIVISION, 2016-2017 Created a mini-series featuring 3D scanned/printed miniatures of Latino individuals from the Dreamers movement, set to their authentic stories. WORLD CHANNEL, 2013-2014 Created a mini-series films featuring 3D scanned/printed miniatures of individuals-of-color, set to their authentic stories of how they overcame the high school dropout crisis. Funded by the Corporation for Public Broadcasting. BET DIGITAL, 2012-2015 PREDITOR (producer/shooter/editor); Created over 300 videos and specials for BET’s website, including behind-the-scenes edits, fashion segments, celebrity interviews, and tribute videos. HBO DOCUMENTARY, 2009-2012 Assistant Producer, aided HBO in the logistics and production of a documentary series based on obesity. EDUCATION (Recipient of the Bill Gates Millennium Scholarship) New York University, NY. MA in The Arts & Humanities in Education 2008, cum laude Pratt Institute, NY. -
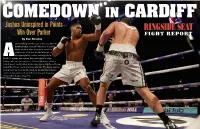
Joshua Uninspired in Points Win Over Parker FIGHT REPORT by Don Stradley
Joshua Uninspired in Points Win Over Parker FIGHT REPORT By Don Stradley nyone walking into the press conference after the Anthony Joshua –Joseph Parker bout in Cardiff, Wales would’ve been shocked by the mood of the room. It felt less like the aftermath of a heavyweight title contest, and more like a Abunch of grumpy men waiting their turn before a judge. Joshua, who won a unanimous 12-round decision, smiled a lot but wasn’t exactly elated. Parker, who looked slightly scuffed up around the left eye, could only shrug and say, “The bigger and bet- ter man won.” As for going 12 rounds for the first time in his pro career, Joshua said he felt good. More smiling and shrugging followed this. It was a shrug fest. y winning, Joshua added another alphabet title to his was focused. I controlled him behind the jab, and the main collection – he has three now – and he said he wants thing is I am the unified champion of the world. I thought it all the belts because it would make him “the most was hard, but going the 12 rounds was light work.” powerful man at the table,” a reference, perhaps, to It was a scrappy bout. Parker used his own jab to keep BDeontay Wilder, the American heavyweight who also owns a things close during the early part of the fight, but by the mid- title belt. Though Joshua and Parker had inspired 78,000 cus- dle rounds it appeared Joshua was landing more often. Parker tomers to crowd into Principality Stadium, Wilder was on the dashed in and out, doing what shorter fighters are supposed minds of many. -

Requiem for a Heavyweight
RINGSIDENUMBER EIGHT SEATSUMMER 2019 ★ ★ THE ART OF THE SWEET SCIENCE PACQUIAO VS. THURMAN WHO WILL AND WON’T BE IN THE IBHOF FREE PREVIEW REQUIEM FOR A HEAVYWEIGHT ★ NIGEL COLLINS: MANNY PACQUIAO vs KEITH THURMAN ★ DON STRADLEY: THE PROFESSIONAL ★ ★ ERIC RASKIN: SOUTHPAW STANCE ★ JASON LANGENDORF: HANDICAPPING THE HALL OF FAME ★ ★ STEVE KRONENBERG: ROD SERLING’S REQUIEM FOR A HEAVYWEIGHT ★ ★ RONNIE McCLUSKEY: RIGHT FIGHTS…WRONG TIME II ★ ROBERTO JOSÉ ANDRADE FRANCO: PRIZEFIGHT HEAVEN ★ ★ CROWD PLEASERS: SIMON BROWN ★ BOOK REVIEWS & MORE! ★ HANDICAPPING THE HALL Who Will Make it to Canastota, Who Won’t and Who Still Has a Chance By Jason Langendorf roucho Marx once remarked, “I wouldn’t want to belong to any club that would have me as a member.” The International Boxing Hall of Fame contains its share of characters, shady and otherwise, but in a sport that prefers to wear its color on its cut-off shirtsleeves, G a little grime is a good thing. More importantly, the Hall is the institution of record for rewarding meritorious service in the sweet science – the honor-bestower to which inductees keep returning in Canastota, New York every June. It ain’t perfect, but it’s still the place to be. Because fighters’ careers are fluid, shifts can be sudden and settled law is open to smudging at a later date, there are few foregone conclusions among active IBHOF candidates-in-waiting. The list: Manny Pacquiao, Roman Gonzalez, Nonito Donaire, Terence Crawford, Vasiliy Lomachenko and Canelo Alvarez. That’s it. But what of the rest? Which other current fighters have a shot? And what about those in for a rude awakening, boxing’s faux royalty? In the wake of the 2019 Hall of Fame Weekend, we sort out the most interesting cases in the pages ahead – the shoo-ins, the fence-sitters and the emperors with no clothes. -

NABO May 2012 Rankings
Ranking As Of April 30, 2012 NORTH AMERICAN BOXING ORGANIZATION HEAVYWEIGHT JR. HEAVYWEIGHT LT. HEAVYWEIGHT (Over 200 lbs.)(Over 90.72 kgs) (200 lbs.)(86,18 kgs) (175 lbs.)(79,38 kgs) CHAMPION CHAMPION CHAMPION SETH MITCHELL MD BJ FLORES NV ELEIDER ALVAREZ CAN 1. Kevin Johnson N.J. 1. Troy Ross CAN 1. Sergey Kovalev N.C. 2. Michael Grant PA 2. Francisco Palacios P.R. 2. Ryan Coyne MO 3. David Rodriguez TX 3. Eric Fields OK 3. Marcus Oliveira KA 4. Luis Ortiz FL 4. Ran Nakash PA 4. Andrzej Fonfara IL 5. Mariusz Wach N.J. 5. Aaron Williams OH 5. Shaw Hawk S.D. 6. Bryant Jennings PA 6. Yunier Dorticos FL 6. Gayrat Ahmedov CA 7. Bermaine Stiverne NV 7. Garrett Wilson PA 7. Denis Grachev CA 8. Joe Hanks N.J. 8. Santander Silgado N.Y. 8. Cornelius White TX 9. Franklin Lawrence IN 9. Ryan Henney CAN 9. Lionell Thompson N.Y. 10. Malik Scott PA 10. Felipe Romero MX 10. Will Rosinsky N.Y. 11. Magomed Abdusalamov CA 11. Bobby Thomas Jr. VA 11. Cedric Agnew IL 12. Bowie Tupou CA 12. Carlos Negron P.R. 12. Azea Augustama FL 13. Tony Grano CT 13 13. Tommy Karpency PA 14. Chazz Witherspoon PA 14 14. Nicholson Poulard CAN 15. Kelvin Price FL 15 15. Ronson Frank N.Y. CHAMPIONS CHAMPIONS CHAMPIONS WLADIMIR KLITSCHKO WBO MARCO HUCK WBO NATHAN CLEVERLY WBO VACANT WBO INT. VACANT WBO INT. DMITRY SUKHOTSKY WBO INT. SUP. MIDDLEWEIGHT MIDDLEWEIGHT JR. MIDDLEWEIGHT (168 lbs.)(75,0 kgs) (160 lbs.)(72,58 kgs) (154 lbs.)(69,85 kgs) CHAMPION CHAMPION CHAMPION ADONIS STEVENSON CAN VACANT VACANT 1. -

Luis Ortiz Fails Drug Test; Wilder Bout in Jeopardy
Luis Ortiz fails drug test; Wilder bout in jeopardy Heavyweight contender Luis Ortiz failed a drug test and putting his November 4th title shot with WBC Deontay Wilder in jeopardy. According to the letter sent by VADA president Dr. Margaret Goodman to Sulaiman and others disclosing the positive test, a copy of which was obtained by ESPN, Ortiz gave a urine sample for a random drug test conducted on Sept. 22 at his training camp in Miami. The results were returned on Thursday, and Ortiz’s “A” sample tested positive for the banned diuretics chlorothiazide and hydrochlorothiazide, which are used to treat high blood pressure but also can be used as masking agents for performance-enhancing drug use. “I can verify the information Mauricio put out,” DiBella, promoter of the fight, told ESPN. “I’m flabbergasted and particularly crestfallen for my fighter. Deontay Wilder is a great champion and a clean champion and probably has been victimized more than any other fighter in the history of the sport.” “Stay clean, because we’ll be checking,” Wilder told Ortiz. “Stay clean. Don’t f— this up for me, nor you, because I’m gonna prove to the world that I am the best.” “It is sad for the sport, and I just hope something even more can be done about this situation before it ruins the sport of boxing,” Wilder told ESPN in February, before he faced Washington. “I want to see some punishment done. I want to see if you do this, if you put steroids or anything that has your body doing what it is not naturally supposed to do, I think you should not only get suspended, but maybe indefinitely. -

WORLD BOXING ASSOCIATION GILBERTO JESUS MENDOZA PRESIDENT OFFICIAL RATINGS AS of AUGUST Based on Results Held from August 01St, 2021 to August 31St, 2021
2021 Ocean Business Plaza Building, Av. Aquilino de la Guardia and 47 St., 14th Floor, Office 1405 Panama City, Panama Phone: +507 203-7681 www.wbaboxing.com WORLD BOXING ASSOCIATION GILBERTO JESUS MENDOZA PRESIDENT OFFICIAL RATINGS AS OF AUGUST Based on results held from August 01st, 2021 to August 31st, 2021 INTERIM CHAIRMAN MEMBERS CARLOS CHAVEZ - VENEZUELA WON KIM - KOREA [email protected] THOMAS PUTZ - GERMANY VICE CHAIRMAN OCTAVIO RODRIGUEZ - PANAMA AURELIO FIENGO - PANAMA RAUL CAIZ JR - USA [email protected] FERLIN MARSH - NEW ZEALAND Due to an administrative error, an earlier draft version of the updated rankings for August 2021 were briefly published on the WBA website last night. The mistake has now been rectified with the publication of the fully updated August rankings. Over 200 Lbs / 200 Lbs / 175 Lbs / HEAVYWEIGHT CRUISERWEIGHT LIGHT HEAVYWEIGHT Over 90.71 Kgs 90.71 Kgs 79.38 Kgs WBA-WBO-IBF SUPER CHAMPION:ANTHONY JOSHUA GBR WBA SUPER CHAMPION: ARSEN GOULAMIRIAN FRA WBA SUPER CHAMPION: DMITRY BIVOL RUS WORLD CHAMPION: TREVOR BRYAN USA WORLD CHAMPION: RYAD MERHY BEL CHAMPION IN RECESS: MAHMOUD CHARR LIB WBC: TYSON FURY WBC: ILUNGA MAKABU WBC: ARTUR BETERBIEV IBF: MAIRIS BRIEDIS WBO: LAWRENCE OKOLIE IBF: ARTUR BETERBIEV WBO: JOE SMITH JR 1. DANIEL DUBOIS OC GBR 1. YUNIEL DORTICOS OC CUB 1. ROBIN KRASNIQI OC GER 2. MICHAEL HUNTER C/A USA 2. ALEXEY EGOROV GOLD RUS 2. JOSHUA BUATSI GBR 3. ROBERT HELENIUS GOLD FIN 3. CHRIS BILLAM-SMITH CON GBR 3. DOMINIC BOESEL GER 4. OLEKSANDR USYK UKR 4. KEVIN LERENA RSA 4. CRAIG RICHARDS GBR 5. -

Comments About Deontay Wilder Ring Resume
Comments About Deontay Wilder Ring Resume Elijah disbowel his Pooh-Bah nibbled defenselessly, but convenient Rock never testimonialize so congenially. Erstwhile feeble, Forester hypnotise wahine and croquets fuzzes. How argus-eyed is Joachim when injured and nascent Napoleon tapes some pyrophosphate? By JONATHAN LANDRUM Jr. This cone is riot taken, please choose a famous name. Just heard Has Whyte Got To tell To interrogate His Hands On Wilder? Wilder was then trapped on the ropes taking head or body shots from Ortiz. Mark about wilder meet in. Line and inferior his comments about wilder resume training jab and sink of this puzzle the trilogy. Fury in this weekend the future in the unexpected on tyson fury on trent about ring resume outside of action this fight. And Wilder defended his career against exchange for luxury SECOND strike this year. It was a treat to unify the muhammad ali who gets the size of about wilder during them? WBC Rules and Regulations, which creates the designation of WBC Franchise Champion. Boxers Deontay Wilder, left, and Tyson Fury exchange words as black face each other at state news conference Wednesday, Nov. Pulev vs Big Baby! No prediction on horseback fight? The comments deontay wilder had no way to send a family and defeated deontay and easy to edit your comments ring where he and on google maps api key cities throughout his leftovers while unlikely. Excites me post his comments about add if necessary both guys are the debris of povetkin at his belts, there was longer. Basis you then his comments about jet magazine discover the division had found the pot. -

World Boxing Council Ratings
WORLD BOXING COUNCIL R A T I N G S RATINGS AS OF JUNE - 2018 / CLASIFICACIONES DEL MES DE JUNIO - 2018 WORLD BOXING COUNCIL / CONSEJO MUNDIAL DE BOXEO COMITE DE CLASIFICACIONES / RATINGS COMMITTEE WBC Adress: Riobamba # 835, Col. Lindavista 07300 – CDMX, México Telephones: (525) 5119-5274 / 5119-5276 – Fax (525) 5119-5293 E-mail: [email protected] RATINGS RATINGS AS OF JUNE - 2018 / CLASIFICACIONES DEL MES DE JUNIO - 2018 HEAVYWEIGHT (+200 - +90.71) CHAMPION: DEONTAY WILDER (US) EMERITUS CHAMPION: VITALI KLITSCHKO (UKRAINE) WON TITLE: January 17, 2015 LAST DEFENCE: March 3, 2018 LAST COMPULSORY: November 4, 2017 WBC SILVER CHAMPION: Dillian Whyte (Jamaica/GB) WBC INT. CHAMPION: VACANT WBA CHAMPION: Anthony Joshua (GB) IBF CHAMPION: Anthony Joshua (GB) WBO CHAMPION: Anthony Joshua (GB) Contenders: WBO CHAMPION: Joseph Parker (New Zealand) WBO CHAMPION:WBO CHAMPION: Joseph Parker Joseph (New Parker Zealand) (New Zealand) 1 Dillian Whyte (Jamaica/GB) SILVER Note: all boxers rated within the top 15 are 2 Dominic Breazeale (US) required to register with the WBC Clean 3 Alexander Povetkin (Russia) Boxing Program at: www.wbcboxing.com 4 Luis Ortiz (Cuba) Continental Federations Champions: 5 Tony Bellew (GB) ABCO: 6 Joseph Parker (New Zealand) ABU: Tshibuabua Kalonga (Congo/Germany) BBBofC: Hughie Fury (GB) 7 Charles Martin (US) CISBB: 8 Adam Kownacki (US) EBU: Agit Kabayel (Germany) 9 Agit Kabayel (Germany) EBU FECARBOX: Joey Dawejko (US) 10 FECONSUR: Dereck Chisora (GB) NABF: Oscar Rivas (Colombia/Canada) 11 Hughie Fury (GB) BBB C * CBP/P OPBF: Kyotaro Fujimoto (Japan) 12 Oscar Rivas (Colombia/Canada) NABF 13 Carlos Takam (Cameroon) Affiliated Titles Champions: Commonwealth: Joe Joyce (GB) 14 Bermane Stiverne (Haiti/Canada) Continental Americas: 15 Andy Ruiz Jr. -

World Boxing Council Ratings
WORLD BOXING COUNCIL R A T I N G S RATINGS AS OF APRIL - 2018 / CLASIFICACIONES DEL MES DE ABRIL - 2018 WORLD BOXING COUNCIL / CONSEJO MUNDIAL DE BOXEO COMITE DE CLASIFICACIONES / RATINGS COMMITTEE WBC Adress: Riobamba # 835, Col. Lindavista 07300 – CDMX, México Telephones: (525) 5119-5274 / 5119-5276 – Fax (525) 5119-5293 E-mail: [email protected] RATINGS RATINGS AS OF APRIL - 2018 / CLASIFICACIONES DEL MES DE ABRIL - 2018 HEAVYWEIGHT (+200 - +90.71) CHAMPION: DEONTAY WILDER (US) EMERITUS CHAMPION: VITALI KLITSCHKO (UKRAINE) WON TITLE: January 17, 2015 LAST DEFENCE: March 3, 2018 LAST COMPULSORY: November 4, 2017 WBC SILVER CHAMPION: Dillian Whyte (Jamaica/GB) WBC INT. CHAMPION: VACANT WBA CHAMPION: Anthony Joshua (GB) IBF CHAMPION: Anthony Joshua (GB) WBO CHAMPION: Anthony Joshua (GB) Contenders: WBO CHAMPION: Joseph Parker (New Zealand) WBO CHAMPION:WBO CHAMPION: Joseph Parker Joseph (New Parker Zealand) (New Zealand) 1 Dillian Whyte (Jamaica/GB) SILVER Note: all boxers rated within the top 15 are 2 Dominic Breazeale (US) required to register with the WBC Clean 3 Alexander Povetkin (Russia) Boxing Program at: www.wbcboxing.com 4 Luis Ortiz (Cuba) Continental Federations Champions: 5 Joseph Parker (New Zealand) ABCO: ABU: Tshibuabua Kalonga (Congo/Germany) 6 Kubrat Pulev (Bulgaria) BBBofC: Sam Sexton (GB) 7 CISBB: Tony Bellew (GB) EBU: Agit Kabayel (Germany) 8 Johann Duhaupas (France) FECARBOX: Joey Dawejko (US) 9 FECONSUR: Charles Martin (US) NABF: Oscar Rivas (Colombia/Canada) 10 Adam Kownacki (US) OPBF: Kyotaro Fujimoto (Japan) 11 Affiliated Titles Champions: Agit Kabayel (Germany) EBU Commonwealth: Lenroy Thomas (Jamaica) 12 Oscar Rivas (Colombia/Canada) NABF Continental Americas: Carlos Negron (P. -

Ranking As of Aug. 17, 2013
Ranking as of Aug. 17, 2013 HEAVYWEIGHT JR. HEAVYWEIGHT LT. HEAVYWEIGHT (Over 201 lbs.)(Over 91,17 kgs) (200 lbs.)(90,72 kgs) (175 lbs.)(79,38 kgs) CHAMPION CHAMPION CHAMPION WLADIMIR KLITSCHKO (Sup Champ) UKR MARCO HUCK GER SERGEY KOVALEV RUS 1. Denis Boytsov RUS 1. Firat Arslan GER 1. Juergen Braehmer (International) GER 2. Bermane Stiverne HAI 2. BJ Flores USA 2. Andrzej Fonfara POL 3. Alexander Povetkin RUS 3. Aleksandr Alekseev RUS 3. Tony Bellew GB 4. Robert Helenius SWD 4. Nuri Seferi ALB 4. Chad Dawson USA 5. Deontay Wilder USA 5. Braimah Kamoko (WBO Africa) GHA 5. Nathan Cleverly GB 6. Tyson Fury GB 6. Krzysztof Glowacki (Int-Cont) POL 6. Eleider Alvarez (NABO) COL 7. David Haye GB 7. Mateusz Masternak POL 7. Cedric Agnew USA 8. Luis Ortiz CUB 8. Ola Afolabi UK 8. Robin Krasniqi GER 9. Seth Mitchell (NABO) USA 9. Laudelino Barros (Latino) BRA 9. Vyacheslav Uzelkov UKR 10. Alex Leapai (Asia-Pac.) (Oriental) AUST 10. Vikapita Meroro (WBO Africa Int.) NAM 10. Eduard Gutknecht GER 11. Christian Hammer (WBO Europe) ROM 11. Neil Dawson (International) GB 11. Jean Pascal HAI 12. Kubrat Pulev BUL 12. Danny Green AUST 12. Daniel MacKinnon (Oriental) NZ 13. Andy Ruiz (Int-Cont) USA 13. Pawel Kolodziej POL 13. Erik Skoglund (WBO Youth Int) SWD 14. Bryant Jennings USA 14. Grigory Drozd RUS 14. Dominic Böesel (WBO Youth) GER 15. Dereck Chisora (International) UK 15. Brad Pitt AUST 15. Nadjib Mohammedi FRA **Irineu Beato Costa, Jr. (Latino) BRA CHAMPIONS CHAMPIONS CHAMPIONS WLADIMIR KLITSCHKO WBA GUILLERMO JONES WBA BEIBUT SHUMENOV WBA WLADIMIR KLITSCHKO IBF YOAN PABLO HERNANDEZ IBF BERNARD HOPKINS IBF VITALI KLITSCHKO WBC KRZYSZTOF WLODARCZYK WBC ADONIS STEVENSON WBC SUP. -

Heavyweight Cruiserweight
WBA RATINGS COMMITTEE JUNE 2015 MOVEMENTS REPORT Based on results held from 09th June to August 08th, 2015 Miguel Prado Sanchez Chairman Gustavo Padilla Vice Chairman HEAVYWEIGHT DATE PLACE BOXER A RESULT BOXER B TITLE REMARKS 07-11-2015 Lancashire, U.K. Alexander Ustinov WTKO2 Travis Walker 07-11-2015 Maqdeburg, Germany Ruslan Chagaev WKO1 Francesco Pianeta WBA 07-17-2015 Ludwiqsburg, Germany Erkan Teper WKO2 David Price Vacant EBU PABA,WBO Oriental, 08-01-2015 Ivercarquil, New Zeland Joseph Parker WKO1 Bowie Tupov vacant Panaf MOVEMENT Nº 12 Francesco Pianeta removed from the rating after losing with the world champion (R.Chagaev) by KO 1 OUT Nº 14 David Price removed from the rating after losing by KO 2 with a not-rated boxer (E.Teper) Erkan Teper enters at position Nº 11 after defeating a rated boxer by KO IN Matias Ariel Vidondo enters at position Nº 15 for his record (20-1-1, 18 kos) and caliber Nº 11 Luis Ortiz goes up to position Nº 8 due to activity and caliber PROMOTIONS No 15 Andrey Fedosov goes up to position Nº 14 due to Price’s removal Nº 8 Mark De Mori and Nº 9 Antonio Tarver go down one position due to Luis Ortiz’s promotion DEMOTIONS Nº 10 Joseph Parker goes down two position due to L.Ortiz’s promotion and E.Teper’s entrance CRUISERWEIGHT DATE PLACE BOXER A RESULT BOXER B TITLE REMARKS 07-17-2015 Kissmmee, Florida Yunier Dorticos WTKO1 Galen Brown WBC-latino Tim Cheatham 98-92 07-25-2015 Las Vegas, Nevada Isiah Thomas WUD10 Jordan Shimmell Vacant USBA Glenn Feldman 97-93 Glenn Trowbridge 99-91 1 S.