Guidelines for Diagnosing and Managing Thyroid Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Beyond the Fixed Setpoint of the Hypothalamus–Pituitary–Thyroid Axis
E Fliers and others Hypothalamus–pituitary– 171:5 R197–R208 Review thyroid axis MECHANISMS IN ENDOCRINOLOGY Beyond the fixed setpoint of the hypothalamus–pituitary–thyroid axis Eric Fliers1, Andries Kalsbeek1,2 and Anita Boelen1 Correspondence should be addressed 1Department of Endocrinology and Metabolism, Academic Medical Center, University of Amsterdam, 1105 AZ to E Fliers Amsterdam, The Netherlands and 2Hypothalamic Integration Mechanisms, Netherlands Institute for Neuroscience, Email Amsterdam, The Netherlands e.fl[email protected] Abstract The hypothalamus–pituitary–thyroid (HPT) axis represents a classical example of an endocrine feedback loop. This review discusses dynamic changes in HPT axis setpoint regulation, identifying their molecular and cellular determinants, and speculates about their functional role. Hypothalamic thyrotropin-releasing hormone neurons were identified as key components of thyroid hormone (TH) setpoint regulation already in the 1980s, and this was followed by the demonstration of a pivotal role for the thyroid hormone receptor beta in negative feedback of TH on the hypothalamic and pituitary level. Gradually, the concept emerged of the HPT axis setpoint as a fixed entity, aiming at a particular TH serum concentration. However, TH serum concentrations appear to be variable and highly responsive to physiological and pathophysiological environmental factors, including the availability or absence of food, inflammation and clock time. During food deprivation and inflammation, TH serum concentrations decrease without a concomitant rise in serum TSH, reflecting a deviation from negative feedback regulation in the HPT axis. Surprisingly, TH action in peripheral organs in these conditions cannot be simply predicted by decreased serum TH concentrations. Instead, diverse environmental stimuli have differential effects on local TH metabolism, e.g. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Thyroid and Polycystic Ovary Syndrome
S Gabersˇcˇek and others Thyroid and PCOS 172:1 R9–R21 Review MECHANISMS IN ENDOCRINOLOGY Thyroid and polycystic ovary syndrome Simona Gabersˇcˇek1,2, Katja Zaletel1, Verena Schwetz3, Thomas Pieber3, Barbara Obermayer-Pietsch3 and Elisabeth Lerchbaum3 Correspondence should be addressed to 1Department of Nuclear Medicine, University Medical Centre Ljubljana, Zalosˇka 7, 1525 Ljubljana, Slovenia, B Obermayer-Pietsch 2Faculty of Medicine, University of Ljubljana, Vrazov trg 2, 1104 Ljubljana, Slovenia and 3Division of Endocrinology Email and Metabolism, Department of Internal Medicine, Medical University of Graz, Auenbruggerplatz 15, barbara.obermayer@ 8036 Graz, Austria medunigraz.at Abstract Thyroid disorders, especially Hashimoto’s thyroiditis (HT), and polycystic ovary syndrome (PCOS) are closely associated, based on a number of studies showing a significantly higher prevalence of HT in women with PCOS than in controls. However, the mechanisms of this association are not as clear. Certainly, genetic susceptibility contributes an important part to the development of HT and PCOS. However, a common genetic background has not yet been established. Polymorphisms of the PCOS-related gene for fibrillin 3 (FBN3) could be involved in the pathogenesis of HT and PCOS. Fibrillins influence the activity of transforming growth factor beta (TGFb). Multifunctional TGFb is also a key regulator of immune tolerance by stimulating regulatory T cells (Tregs), which are known to inhibit excessive immune response. With lower TGFb and Treg levels, the autoimmune processes, well known in HT and assumed in PCOS, might develop. In fact, lower levels of TGFb1 were found in HT as well as in PCOS women carrying allele 8 of D19S884 in the FBN3 gene. -

Thyroid Disease
Thyroid Disease Thyroid disease occurs when the thyroid (a small, butterfly-shaped gland in the front of your neck) does not produce the right amount of thyroid hormone. These hormones control how your body uses energy. If you are feeling fatigued, notice skin or hair changes, or have hoarseness or pain, your doctor may conduct a physical exam and order blood tests. If these tests indicate a problem, your doctor may order thyroid scan and uptake, thyroid biopsy, or imaging tests to help diagnose and evaluate a thyroid condition. Treatment will depend on the specific nature of your thyroid condition and its underlying cause. What is thyroid disease? The thyroid is a small, butterfly-shaped gland in the front of your neck that wraps around your windpipe (trachea). The two halves of the thyroid gland are connected in the middle by a thin layer of tissue known as the isthmus. The thyroid gland uses iodine (mostly absorbed from food) to produce hormones that control how your body uses energy. Nearly every organ in the body is affected by the function of the thyroid gland. The pituitary gland and hypothalamus, an area at the base of the brain, control the rate at which the thyroid produces and releases these hormones. The main function of the thyroid gland is to release a hormone called thyroxine or T4, which is converted into a hormone called T3. Both of these hormones circulate in the bloodstream and help regulate your metabolism. The amount of T4 produced by the thyroid gland is determined by a hormone produced by the pituitary gland called TSH or thyroid-stimulating hormone. -

Primary Hyperparathyroidism
Primary Hyperparathyroidism The parathyroid glands are 4 glands that reside within the thyroid glands: there are two parathyroid glands attached to each thyroid gland. The thyroid/parathyroid glands lie on either side of the trachea (wind pipe) about midway down the neck. The job of the parathyroid glands is to regulate calcium in the body. They secrete a hormone called parathyroid hormone (PTH), and this hormone draws calcium out of the bone where it is stored, as well as acting on the kidney and intestine to increase blood calcium. This is a normal process in response to fluctuations in blood calcium levels. The calcium in the blood is regulated by PTH (increases blood calcium) and calcitonin (a hormone secreted by the thyroid gland to decrease calcium) in order to keep it within a normal range. When the calcium gets too high or too low, symptoms arise. The most common symptoms of high calcium are increased thirst and urination. Other signs include: lethargy, weakness, diarrhea, inappetance, weight loss, tremors or stiffness. In about 50% of dogs with high calcium, urinary stones +/- urinary tract infection is present. Tumors (enlargement) of the parathyroid gland are typically not malignant, but they do over-secrete PTH. In 90% of cases only one of the four glands is enlarged. By one gland enlarging and over-secreting PTH, the three other glands typically shrink and temporarily stop functioning. Parathyroid tumors are suspected based on consistent blood work that shows elevated or normal PTH in the face of elevated calcium (the normal feedback mechanism would mean that when calcium is high, PTH is not needed and therefore is low). -

Hypothyroidism and Pregnancy: What Should I Know?
Fact Sheet From ReproductiveFacts.org The Patient Education Website of the American Society for Reproductive Medicine Hypothyroidism and pregnancy: what should I know? What is hypothyroidism? to protect you against bacterial and viral infections. Sometimes, Hypothyroidism (underactive thyroid) is when the thyroid gland however, the immune system can make antibodies against produces less thyroid hormone than it should. The thyroid gland is your own body—such as against your thyroid. T4 is a hormone found in the lower part of the throat and partially wraps around the produced directly by the thyroid gland. It is typically low in patients upper windpipe (trachea). with hypothyroidism. An autoantibody is an antibody that attacks the cells and tissues of the organism that made it. Thyroid What does the thyroid gland do? autoantibodies are seen in patients with Hashimoto’s (autoimmune) The thyroid gland produces two hormones: triiodothyronine (T3) thyroiditis. and thyroxine (T4). These hormones play an important role in metabolism. Metabolism is the body’s ability to transform food How does hypothyroidism affect my fertility and into energy. The thyroid gland is controlled (regulated) by thyroid- my baby if I become pregnant? stimulating hormone (TSH). TSH is produced by the pituitary gland, Hypothyroidism can prevent the release of the egg from the ovary which is located in the brain. (ovulation). Typically, for women who have periods (menstruate) each month, an egg is released from the ovary each month. What are the symptoms of hypothyroidism? But women who have hypothyroidism may release an egg less When the thyroid gland produces less thyroid hormone than it frequently or not at all. -

Endocrine System with Special Reference to Thyroid Gland
Odisha Review December - 2012 Endocrine System With Special Reference to Thyroid Gland Soma Mishra Endocrine system consisting of a group of ductless glands viz. pituitary, thyroid, parathyroid, pineal, thymus, gonads, pancreas, adrenal etc. plays a very vital role in governing human behavior. Thyroid is one of the most important glands that control body’s metabolism and calcium level. It secretes iodothyronines that are (tri-iodo- thyronine, thyroxine) and calcitonin. Its secretion is mainly regulated by TRH (thyrotropin releasing hormone) and TSH (thyroid stimulating hormone). It helps in growth (physical, sexual, mental) – development- metamorphosis and calorigenesis- metabolism. The status of thyroid gland may be Euthyroid or Hypothyroid or Hyperthyroid. Hypothyroidism includes cretinism in children and myxoedema in adults. Common causes of hyperthyroid state are Grave’s disease, multinodular goiter, thyroiditis, etc. Any enlargement of thyroid gland, regardless of cause, is called goiter. Some common investigations for Introduction thyroid diseases are estimation of serum T3, T4 The endocrine system or hormonal system and TSH, cholesterol, radioiodine uptake, thyroid is a complex system composed of a group of imaging, etc. Common drug used in ductless glands known as endocrine glands that hypothyroidism is eltroxin, hyperthyroidism is pour their secretions i.e. hormones directly into carbimazole and iodine supplementation in goiter. blood for passage to different body organs known This paper presents a full picture of thyroid gland, as target organs in order to control their its functioning, disorders, and treatments which is functioning, metabolism, cell permeability, growth, very significant for human survival. differentiation and stress conditions. 54 December - 2012 Odisha Review The endocrine system includes the Diseases of the endocrine system result pituitary gland, thyroid gland, parathyroid glands, from too much or too little hormone secretion or adrenal gland, pancreas, ovaries and testes. -

A Seasonal Study of Pinealocytes in the 13-Lined Ground Squirrel, Spermophilus Tridecemlineatus J
A seasonal study of pinealocytes in the 13-lined ground squirrel, Spermophilus tridecemlineatus J. A. Mcnulty, Teresa A. Dombrowski, Wilma A. Spurrier To cite this version: J. A. Mcnulty, Teresa A. Dombrowski, Wilma A. Spurrier. A seasonal study of pinealocytes in the 13- lined ground squirrel, Spermophilus tridecemlineatus. Reproduction Nutrition Développement, 1980, 20 (3A), pp.665-672. hal-00897671 HAL Id: hal-00897671 https://hal.archives-ouvertes.fr/hal-00897671 Submitted on 1 Jan 1980 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. A seasonal study of pinealocytes in the 13-lined ground squirrel, Spermophilus tridecemlineatus J. A. McNULTY, Teresa A. DOMBROWSKI, Wilma A. SPURRIER Departments of Anatomy and Physiology, Loyola University Stritch School of Medicine, 2160 S. First Avenue, Maywood, Illinois 60153 USA. Summary. A quantitative histological study of pinealocytes in the 13-lined ground squir- rel, Spermophilus tridecemlineatus, was conducted over a period of one year. Consistent and statistically significant seasonal differences were found in nuclear and nucleolar dimensions suggesting a circannual rhythm in the metabolism of these cells. Annual peaks occurred during hibernation, whereas the nadirs occurred during the period of sexual activity. -

Background Information
November 18, 2013 INFORMATION ON THE C-8 (PFOA) MEDICAL MONITORING PROGRAM SCREENING TESTS PREPARED BY THE MEDICAL PANEL FOR THE C-8 CLASS MEMBERS The Medical Panel has made recommendations about medical screening tests that C-8 Class Members could have done to find out if they have any of the Probable Link Conditions identified by the Science Panel. This document is about the Medical Monitoring Program. For each of the Probable Link conditions, the document explains who is eligible to have the screening tests and the possible benefits and risks of the screening tests. The Medical Panel wants you to understand the benefits and risks of the tests, so you can decide whether you want to have the tests done. We encourage you to read about the tests and discuss this information with the doctor who can do the screening tests. Background Information In February 2005, the West Virginia Circuit Court approved a Settlement Agreement in a class action lawsuit entitled Jack Leach et al. v. E.I. du Pont de Nemours and Co., Civil Action No. 01-C-608. The suit was about release of a chemical known as C-8, also known as PFOA, from DuPont's Washington Works facility located in Wood County, West Virginia. “Class Members” are current or former residents of the communities affected by release of C-8. The Settlement had several parts. The Settlement Agreement established a Science Panel to investigate possible links between exposure to C-8 and any diseases. The Panel’s research found that C-8 exposure was probably linked to high cholesterol, thyroid disease, ulcerative colitis, testicular cancer, kidney cancer, and high blood pressure during pregnancy. -
Thyroid Cancer Resource List
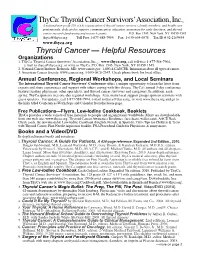
ThyCa: Thyroid Cancer Survivors’ Association, Inc.SM A national non-profit 501 (c)(3) organization of thyroid cancer survivors, family members, and health care professionals, dedicated to support, communication, education, awareness for early detection, and thyroid cancer research fundraising and research grants P.O. Box 1545, New York, NY 10159-1545 [email protected] Toll Free 1-877-588-7904 Fax: 1-630-604-6078 Tax ID # 52-2169434 www.thyca.org Thyroid Cancer — Helpful Resources Organizations 1. ThyCa: Thyroid Cancer Survivors’ Association, Inc.SM, www.thyca.org, call toll-free 1-877-588-7904, e-mail to [email protected], or write to ThyCa, P.O. Box 1545, New York, NY 10159-1545. 2. National Cancer Institute, Bethesda, MD. www.cancer.gov. 1-800-4-CANCER. Information about all types of cancer. 3. American Cancer Society. www.cancer.org. 1-800-ACS-2345. Check phone book for local office. Annual Conference, Regional Workshops, and Local Seminars The International Thyroid Cancer Survivors' Conference offers a unique opportunity to learn the latest from experts and share experiences and support with others coping with this disease. ThyCa's annual 3-day conference features leading physicians, other specialists, and thyroid cancer survivors and caregivers. In addition, each spring, ThyCa sponsors free one-day regional workshops. Also, many local support groups sponsor seminars with guest speakers. For updates, call 1-877-588-7904, e-mail to [email protected], or visit www.thyca.org and go to the links titled Conferences/Workshops and Calendar from the home page. Free Publications—Flyers, Low-Iodine Cookbook, Booklets ThyCa provides a wide variety of free materials to people and organizations worldwide. -

Thyroid Function Tests WHAT IS the THYROID GLAND? T4 and T3 Circulate Almost Entirely Bound to Specific Transport Proteins
AMERICAN THYROID ASSOCIATION® www.thyroid.org Thyroid Function Tests WHAT IS THE THYROID GLAND? T4 and T3 circulate almost entirely bound to specific transport proteins. If the levels of these transport proteins The thyroid gland is a butterfly-shaped endocrine gland changes, there can be changes in how much bound that is normally located in the lower front of the neck. T4 and T3 is measured. This frequently happens during The thyroid’s job is to make thyroid hormones, which are pregnancy and with the use of birth control pills. The “free” secreted into the blood and then carried to every tissue T4 or T3 is the hormone that is unbound and able to enter in the body. Thyroid hormones help the body use energy, and affect the body tissues. stay warm and keep the brain, heart, muscles, and other organs working as they should. TESTS HOW DOES THE THYROID GLAND FUNCTION? Blood tests to measure these hormones are readily available and widely used, but not all are useful in all situations. Tests The major thyroid hormone secreted by the thyroid to evaluate thyroid function include the following: gland is thyroxine, also called T4 because it contains four iodine atoms. To exert its effects, T4 is converted to TSH TESTS triiodothyronine (T3) by the removal of an iodine atom. This The best way to initially test thyroid function is to occurs mainly in the liver and in certain tissues where T3 measure the TSH level in a blood sample. Changes in acts, such as in the brain. The amount of T4 produced by TSH can serve as an “early warning system” – often the thyroid gland is controlled by another hormone, which occurring before the actual level of thyroid hormones in is made in the pituitary gland located at the base of the the body becomes too high or too low. -

Underactive Thyroid Gland
AMERICAN THYROID ASSOCIATION® www.thyroid.org Hypothyroidism WHAT IS THE THYROID GLAND? WHAT CAN YOU EXPECT OVER THE LONG TERM? The thyroid gland is a butterfly-shaped endocrine gland There is no cure for hypothyroidism, and most patients that is normally located in the lower front of the neck. have it for life. There are exceptions: many patients with The thyroid’s job is to make thyroid hormones, which are viral thyroiditis have their thyroid function return to normal, secreted into the blood and then carried to every tissue as do some patients with thyroiditis after pregnancy. in the body. Thyroid hormone helps the body use energy, Hypothyroidism may become more or less severe, and stay warm and keep the brain, heart, muscles, and other your dose of thyroxine may need to change over time. You organs working as they should. have to make a lifetime commitment to treatment. But if you take your pills every day and work with your doctor WHAT IS HYPOTHYROIDISM? to get and keep your thyroxine dose right, you should Hypothyroidism is an underactive thyroid gland. be able to keep your hypothyroidism well controlled Hypothyroidism means that the thyroid gland can’t make throughout your life. Your symptoms should disappear and enough thyroid hormone to keep the body running the serious effects of low thyroid hormone should improve. normally. People are hypothyroid if they have too little If you keep your hypothyroidism well-controlled, it will not thyroid hormone in the blood. Common causes are shorten your life span. autoimmune disease, such as Hashimoto’s thyroiditis, surgical removal of the thyroid, and radiation treatment.