Vitamin B12 Deficiency Sally P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recent Insights Into the Role of Vitamin B12 and Vitamin D Upon Cardiovascular Mortality: a Systematic Review
Acta Scientific Pharmaceutical Sciences (ISSN: 2581-5423) Volume 2 Issue 12 December 2018 Review Article Recent Insights into the Role of Vitamin B12 and Vitamin D upon Cardiovascular Mortality: A Systematic Review Raja Chakraverty1 and Pranabesh Chakraborty2* 1Assistant Professor, Bengal School of Technology (A College of Pharmacy), Sugandha, Hooghly, West Bengal, India 2Director (Academic), Bengal School of Technology (A College of Pharmacy),Sugandha, Hooghly, West Bengal, India *Corresponding Author: Pranabesh Chakraborty, Director (Academic), Bengal School of Technology (A College of Pharmacy), Sugandha, Hooghly, West Bengal, India. Received: October 17, 2018; Published: November 22, 2018 Abstract since the pathogenesis of several chronic diseases have been attributed to low concentrations of this vitamin. The present study Vitamin B12 and Vitamin D insufficiency has been observed worldwide at all stages of life. It is a major public health problem, throws light on the causal association of Vitamin B12 to cardiovascular disorders. Several evidences suggested that vitamin D has an effect in cardiovascular diseases thereby reducing the risk. It may happen in case of gene regulation and gene expression the vitamin D receptors in various cells helps in regulation of blood pressure (through renin-angiotensin system), and henceforth modulating the cell growth and proliferation which includes vascular smooth muscle cells and cardiomyocytes functioning. The present review article is based on identifying correct mechanisms and relationships between Vitamin D and such diseases that could be important in future understanding in patient and healthcare policies. There is some reported literature about the causative association between disease (CAD). Numerous retrospective and prospective studies have revealed a consistent, independent relationship of mild hyper- Vitamin B12 deficiency and homocysteinemia, or its role in the development of atherosclerosis and other groups of Coronary artery homocysteinemia with cardiovascular disease and all-cause mortality. -

Scurvy Due to Selective Diet in a Seemingly Healthy 4-Year-Old Boy Andrew Nastro, MD,A,G,H Natalie Rosenwasser, MD,A,B Steven P
Scurvy Due to Selective Diet in a Seemingly Healthy 4-Year-Old Boy Andrew Nastro, MD,a,g,h Natalie Rosenwasser, MD,a,b Steven P. Daniels, MD,c Jessie Magnani, MD,a,d Yoshimi Endo, MD,e Elisa Hampton, MD,a Nancy Pan, MD,a,b Arzu Kovanlikaya, MDf Scurvy is a rare disease in developed nations. In the field of pediatrics, it abstract primarily is seen in children with developmental and behavioral issues, fDivision of Pediatric Radiology and aDepartments of malabsorptive processes, or diseases involving dysphagia. We present the Pediatrics and cRadiology, NewYork-Presbyterian/Weill Cornell Medical Center, New York, New York; bDivision of case of an otherwise developmentally appropriate 4-year-old boy who Pediatric Rheumatology and eDepartment of Radiology, developed scurvy after gradual self-restriction of his diet. He initially Hospital for Special Surgery, New York, New York; and d presented with a limp and a rash and was subsequently found to have anemia Division of Neonatal-Perinatal Medicine, University of Michigan, Ann Arbor, Michigan gDepartment of Pediatrics, and hematuria. A serum vitamin C level was undetectable, and after review of NYU School of Medicine, New York, New York hDepartment of the MRI of his lower extremities, the clinical findings supported a diagnosis of Pediatrics, Bellevue Hospital Center, New York, New York scurvy. Although scurvy is rare in developed nations, this diagnosis should be Dr Nastro helped conceptualize the case report, considered in a patient with the clinical constellation of lower-extremity pain contributed to writing the introduction, initial presentation, hospital course, and discussion, and or arthralgias, a nonblanching rash, easy bleeding or bruising, fatigue, and developed the laboratory tables while he was anemia. -

Family Practice
THE JOURNAL OF FAMILY PRACTICE Emmanuel Andrès, MD, B12 deficiency: A look beyond Laure Federici, MD, Stéphan Affenberger, MD pernicious anemia Department of Internal Medicine, Diabetes and Metabolic Diseases, Food-B12 malabsorption—not pernicious anemia—is the Hôpitaux Universitaires de Strasbourg, leading cause of B12 malabsorption. It’s also very subtle Strasbourg, France emmanuel.andres @chru-strasbourg.fr Practice recommendations such as its link to Helicobacter pylori • Mild, preclinical B deficiency infection and long-term antacid and bi- Josep Vidal-Alaball, MD 12 Department of General is associated with food-B12 guanide use. It also requires that you Practice, Cardiff University, malabsorption more often than consider not only a patient’s serum B12 United Kingdom with pernicious anemia. (C) ® Dowdenlevels, but his Health homocysteine Media and meth - Noureddine Henoun ylmalonic acid levels, since they are con- Loukili, PhD • The classic treatment for B 12 Department of Hygiene and deficiency—particularly when the sidered more sensitive indicators of co- 6 Fight against Nosocomial cause is not a dietaryCopyright deficiency—isFor personalbalamin deficiency. use Keyingonly in on these Infections, Hôpital Calmette, 100 to 1000 mcg per month of indicators early will ensure prompt treat- CHRU de Lille, Lille, France cyanocobalamin, IM. (B) ment, which typically includes intramus- cular injections of the vitamin, but which Jacques Zimmer, MD, PhD • Oral crystalline cyanocobalamin could revolve around a more convenient Laboratoire is an effective treatment for food- d’Immunogénétique- option: oral B12. Allergologie, Centre de B12 malabsorption, though it’s Recherche Public de la Santé effectiveness in the long term has (CRP-Santé) de Luxembourg, not been demonstrated. -

Nutrition 102 – Class 3
Nutrition 102 – Class 3 Angel Woolever, RD, CD 1 Nutrition 102 “Introduction to Human Nutrition” second edition Edited by Michael J. Gibney, Susan A. Lanham-New, Aedin Cassidy, and Hester H. Vorster May be purchased online but is not required for the class. 2 Technical Difficulties Contact: Erin Deichman 574.753.1706 [email protected] 3 Questions You may raise your hand and type your question. All questions will be answered at the end of the webinar to save time. 4 Review from Last Week Vitamins E, K, and C What it is Source Function Requirement Absorption Deficiency Toxicity Non-essential compounds Bioflavonoids: Carnitine, Choline, Inositol, Taurine, and Ubiquinone Phytoceuticals 5 Priorities for Today’s Session B Vitamins What they are Source Function Requirement Absorption Deficiency Toxicity 6 7 What Is Vitamin B1 First B Vitamin to be discovered 8 Vitamin B1 Sources Pork – rich source Potatoes Whole-grain cereals Meat Fish 9 Functions of Vitamin B1 Converts carbohydrates into glucose for energy metabolism Strengthens immune system Improves body’s ability to withstand stressful conditions 10 Thiamine Requirements Groups: RDA (mg/day): Infants 0.4 Children 0.7-1.2 Males 1.5 Females 1 Pregnancy 2 Lactation 2 11 Thiamine Absorption Absorbed in the duodenum and proximal jejunum Alcoholics are especially susceptible to thiamine deficiency Excreted in urine, diuresis, and sweat Little storage of thiamine in the body 12 Barriers to Thiamine Absorption Lost into cooking water Unstable to light Exposure to sunlight Destroyed -
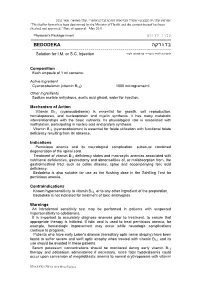
בדודקה BEDODEKA ------להזרקה לתוך השריר או מתחת לעור Solution for I.M
"פורמט עלון זה נקבע ע"י משרד הבריאות ותוכנו נבדק ואושר". עלון מאושר: מאי 2011. “This leaflet format has been determined by the Ministry of Health and the content thereof has been checked and approved.” Date of approval: May 2011. עלון לרופא Physician's Package Insert ========================================================================== בדודקה BEDODEKA --------------------------------------------------------------------- להזרקה לתוך השריר או מתחת לעור Solution for I.M. or S.C. Injection Composition Each ampoule of 1 ml contains: Active Ingredient Cyanocobalamin (vitamin B12) 1000 micrograms/ml Other Ingredients Sodium acetate anhydrous, acetic acid glacial, water for injection. Mechanism of Action Vitamin B12 (cyanocobalamin) is essential for growth, cell reproduction, hematopoiesis, and nucleoprotein and myelin synthesis. It has many metabolic interrelationships with the basic nutrients. Its physiological role is associated with methylation, participating in nucleic acid and protein synthesis. Vitamin B12 (cyanocobalamin) is essential for folate utilization with functional folate deficiency resulting from its absence. Indications Pernicious anemia and its neurological complication, subacute combined degeneration of the spinal cord. Treatment of vitamin B12 deficiency states and macrocytic anemias associated with nutritional deficiencies, gastrectomy and abnormalities of, or malabsorption from, the gastrointestinal tract such as celiac disease, sprue and accompanying folic acid deficiency. Bedodeka is also suitable for use as the flushing dose in the Schilling Test for pernicious anemia. Contraindications Known hypersensitivity to vitamin B12, or to any other ingredient of the preparation. Bedodeka is not indicated for treatment of toxic amblyopias. Warnings An intradermal sensitivity test may be performed in patients with suspected hypersensitivity to cobalamins. It is important to accurately diagnose anemias prior to treatment, to ensure that appropriate therapy is initiated. -

Detailed Investigations of Proximal Tubular Function in Imerslund-Grasbeck Syndrome
Detailed investigations of proximal tubular function in Imerslund-Grasbeck syndrome. Tina Storm, Christina Zeitz, Olivier Cases, Sabine Amsellem, Pierre Verroust, Mette Madsen, Jean-François Benoist, Sandrine Passemard, Sophie Lebon, Iben Jønsson, et al. To cite this version: Tina Storm, Christina Zeitz, Olivier Cases, Sabine Amsellem, Pierre Verroust, et al.. Detailed in- vestigations of proximal tubular function in Imerslund-Grasbeck syndrome.. BMC Medical Genetics, BioMed Central, 2013, 14 (1), pp.111. 10.1186/1471-2350-14-111. inserm-00904107 HAL Id: inserm-00904107 https://www.hal.inserm.fr/inserm-00904107 Submitted on 13 Nov 2013 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Storm et al. BMC Medical Genetics 2013, 14:111 http://www.biomedcentral.com/1471-2350/14/111 RESEARCHARTICLE Open Access Detailed investigations of proximal tubular function in Imerslund-Gräsbeck syndrome Tina Storm1, Christina Zeitz2,3,4, Olivier Cases2,3,4, Sabine Amsellem2,3,4, Pierre J Verroust1,2,3,4, Mette Madsen1, Jean-François Benoist6, Sandrine Passemard7,8, Sophie Lebon8, Iben Møller Jønsson9, Francesco Emma10, Heidi Koldsø11, Jens Michael Hertz12, Rikke Nielsen1, Erik I Christensen1* and Renata Kozyraki2,3,4,5* Abstract Background: Imerslund-Gräsbeck Syndrome (IGS) is a rare genetic disorder characterised by juvenile megaloblastic anaemia. -

VI.2 Elements for a Public Summary VI.2.1 Overview of Disease Epidemiology Vitamin B12 Deficiency Can Have a Number of Possible
VI.2 Elements for a public summary VI.2.1 Overview of disease epidemiology Vitamin B12 deficiency can have a number of possible causes. Typically it occurs in people whose digestive systems do not adequately absorb the vitamin from the foods they eat. This can be caused by: Pernicious anemia, a condition in where there is a lack of a protein called intrinsic factor. The protein, which is made in the stomach, is necessary for vitamin B12 absorption. Other causes can be gastritis, surgery in which part of the stomach and/or small intestine is removed or conditions affecting the small intestine. Vitamin B12 deficiency can also occur in pregnancy and with long- term use of acid-reducing drugs. VI.2.2 Summary of treatment benefits A deficiency of vitamin B12 (cobalamin) is manifested by fatigue, weakness, mood fluctuations, memory loss, limb weakness, difficulty walking, tingling, and paralysis. Drug treatment involves the administration of vitamin B12 by injection. If the deficiency of vitamin B12 (cobalamin) depends on the underlying disease being resolved, the vitamin supplementation continues until normal levels of vitamin B12 are achieved. If the deficiency state cannot be resolved (e.g. inadequate secretion of intrinsic factor, genetic abnormalities related to the site absorption, etc.) therapy should be continued for life. VI.2.3 Unknowns relating to treatment benefits None. VI.2.4 Summary of safety concerns Risk What is known Preventability Damage to the optic nerve Optic nerve atrophy/blindness The product should be used (atrophy)/blindness in is a risk associated with with caution. patients with Leber´s disease treatment with (a disease that affects the hydroxocobalamin in patients optic nerve and often causes with Leber´s disease. -
Detailed Investigations of Proximal Tubular Function in Imerslund-Gräsbeck Syndrome
Storm et al. BMC Medical Genetics 2013, 14:111 http://www.biomedcentral.com/1471-2350/14/111 RESEARCH ARTICLE Open Access Detailed investigations of proximal tubular function in Imerslund-Gräsbeck syndrome Tina Storm1, Christina Zeitz2,3,4, Olivier Cases2,3,4, Sabine Amsellem2,3,4, Pierre J Verroust1,2,3,4, Mette Madsen1, Jean-François Benoist6, Sandrine Passemard7,8, Sophie Lebon8, Iben Møller Jønsson9, Francesco Emma10, Heidi Koldsø11, Jens Michael Hertz12, Rikke Nielsen1, Erik I Christensen1* and Renata Kozyraki2,3,4,5* Abstract Background: Imerslund-Gräsbeck Syndrome (IGS) is a rare genetic disorder characterised by juvenile megaloblastic anaemia. IGS is caused by mutations in either of the genes encoding the intestinal intrinsic factor-vitamin B12 receptor complex, cubam. The cubam receptor proteins cubilin and amnionless are both expressed in the small intestine as well as the proximal tubules of the kidney and exhibit an interdependent relationship for post-translational processing and trafficking. In the proximal tubules cubilin is involved in the reabsorption of several filtered plasma proteins including vitamin carriers and lipoproteins. Consistent with this, low-molecular-weight proteinuria has been observed in most patients with IGS. The aim of this study was to characterise novel disease-causing mutations and correlate novel and previously reported mutations with the presence of low-molecular-weight proteinuria. Methods: Genetic screening was performed by direct sequencing of the CUBN and AMN genes and novel identified mutations were characterised by in silico and/or in vitro investigations. Urinary protein excretion was analysed by immunoblotting and high-resolution gel electrophoresis of collected urines from patients and healthy controls to determine renal phenotype. -

AMN Directs Endocytosis of the Intrinsic Factor‐Vitamin B12
Traffic 2010; 11: 706–720 © 2010 John Wiley & Sons A/S doi:10.1111/j.1600-0854.2010.01042.x AMN Directs Endocytosis of the Intrinsic Factor-Vitamin B12 Receptor Cubam by Engaging ARH or Dab2 Gitte Albinus Pedersen1,†, Souvik tubules of the kidney, cubam is involved in reabsorption Chakraborty2,†, Amie L. Steinhauser2, of various proteins from the glomerular ultrafiltrate (for 2 1,∗ example albumin, transferrin, apolipoprotein A-I and vita- Linton M. Traub and Mette Madsen min D-binding protein), thereby reducing proteinuria (5–8). The cubam complex has been shown to play an impor- 1 tant role during fetal development in rodents (2,4), but Department of Medical Biochemistry, University of presently its role in the human yolk sac is unclear. Aarhus, Ole Worms Alle,´ Bldg. 1170-1171, DK-8000 Aarhus C, Denmark ∼ 2Department of Cell Biology and Physiology, University of Cubilin is an 460-kDa protein composed of a short Pittsburgh School of Medicine, Pittsburgh, PA 15213, N-terminal region followed by eight epidermal growth USA factor (EGF)-like repeats and 27 contiguous CUB *Corresponding author: Mette Madsen, domains (9,10). The cubilin protein includes no identifiable [email protected] transmembrane region or classical signals for endocytosis. †These authors contributed equally to this study. These features are, however, found in the other cubam partner, AMN, which is an ∼45-kDa type I transmembrane Cubam is a multi-ligand receptor involved in dietary protein containing two putative internalization signals of uptake of intrinsic factor-vitamin B12 in the small intestine the FXNPXF type within its cytosolic domain (1,11,12). -

Iron Deficiency and the Anemia of Chronic Disease
Thomas G. DeLoughery, MD MACP FAWM Professor of Medicine, Pathology, and Pediatrics Oregon Health Sciences University Portland, Oregon [email protected] IRON DEFICIENCY AND THE ANEMIA OF CHRONIC DISEASE SIGNIFICANCE Lack of iron and the anemia of chronic disease are the most common causes of anemia in the world. The majority of pre-menopausal women will have some element of iron deficiency. The first clue to many GI cancers and other diseases is iron loss. Finally, iron deficiency is one of the most treatable medical disorders of the elderly. IRON METABOLISM It is crucial to understand normal iron metabolism to understand iron deficiency and the anemia of chronic disease. Iron in food is largely in ferric form (Fe+++ ) which is reduced by stomach acid to the ferrous form (Fe++). In the jejunum two receptors on the mucosal cells absorb iron. The one for heme-iron (heme iron receptor) is very avid for heme-bound iron (absorbs 30-40%). The other receptor - divalent metal transporter (DMT1) - takes up inorganic iron but is less efficient (1-10%). Iron is exported from the enterocyte via ferroportin and is then delivered to the transferrin receptor (TfR) and then to plasma transferrin. Transferrin is the main transport molecule for iron. Transferrin can deliver iron to the marrow for the use in RBC production or to the liver for storage in ferritin. Transferrin binds to the TfR on the cell and iron is delivered either for use in hemoglobin synthesis or storage. Iron that is contained in hemoglobin in senescent red cells is recycled by binding to ferritin in the macrophage and is transferred to transferrin for recycling. -

Iron Deficiency Anemia: Evaluation and Management MATTHEW W
Iron Deficiency Anemia: Evaluation and Management MATTHEW W. SHORT, LTC, MC, USA, and JASON E. DOMAGALSKI, MAJ, MC, USA Madigan Healthcare System, Tacoma, Washington Iron deficiency is the most common nutritional disorder worldwide and accounts for approxi- mately one-half of anemia cases. The diagnosis of iron deficiency anemia is confirmed by the findings of low iron stores and a hemoglobin level two standard deviations below normal. Women should be screened during pregnancy, and children screened at one year of age. Supple- mental iron may be given initially, followed by further workup if the patient is not responsive to therapy. Men and postmenopausal women should not be screened, but should be evaluated with gastrointestinal endoscopy if diagnosed with iron deficiency anemia. The underlying cause should be treated, and oral iron therapy can be initiated to replenish iron stores. Paren- teral therapy may be used in patients who cannot tolerate or absorb oral preparations. (Am Fam Physician. 2013;87(2):98-104. Copyright © 2013 American Academy of Family Physicians.) ▲ Patient information: ron deficiency anemia is diminished red causes of microcytosis include chronic A handout on iron defi- blood cell production due to low iron inflammatory states, lead poisoning, thalas- ciency anemia, written by 1 the authors of this article, stores in the body. It is the most com- semia, and sideroblastic anemia. is available at http://www. mon nutritional disorder worldwide The following diagnostic approach is rec- aafp.org/afp/2013/0115/ I and accounts for approximately one-half of ommended in patients with anemia and is p98-s1.html. Access to anemia cases.1,2 Iron deficiency anemia can outlined in Figure 1.2,6-11 A serum ferritin level the handout is free and unrestricted. -

The Relationship Between Serum Vitamin D Level, Anemia, and Iron Deficiency in Preschool Children
HAYDARPAŞA NUMUNE MEDICAL JOURNAL DOI: 10.14744/hnhj.2019.48278 Haydarpasa Numune Med J 2019;59(3):220–223 ORIGINAL ARTICLE hnhtipdergisi.com The Relationship Between Serum Vitamin D Level, Anemia, and Iron Deficiency in Preschool Children Ömer Kartal, Orhan Gürsel Department of Pediatric Hematology and Oncology, Gulhane Training and Research Hospital, Ankara, Turkey Abstract Introduction: Vitamin D deficiency and iron deficiency are the most common nutritional pandemic problems worldwide at all levels of society. In some studies, vitamin D has been shown to have an effect on erythropoiesis. The objective of this study was to investigate the relationship between serum vitamin D level, hemogram parameters, and serum iron level in preschool children. Methods: The study group comprised 108 children aged between 2 and 5 years who visited a single pediatric hematology polyclinic between August 2014 and August 2017and whose serum vitamin D level and iron parameters were evaluated. The patients were divided into 3 groups according to the hemoglobin value, serum ferritin level, and transferrin saturation index calculation: iron deficiency, iron deficiency anemia, and a control group. Vitamin D deficiency, insufficiency, and normal cate- gories were also used based on assessment of the serum vitamin D level. Results: There were 41 children in the iron deficiency group, 32 classified as iron deficiency anemia, and 35 age- and sex- mated controls. The vitamin D level was statistically significant between the groups (p<0.05). Discussion and Conclusion: According to our findings, vitamin D deficiency and insufficiency were prevalent, especially in children with iron deficiency anemia. It is recommended that the serum vitamin D level of children with iron deficiency ane- mia should be checked and vitamin D-fortified food consumption should be increased.