Annual Report and Annual Accounts 2019/20 Enclosure D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Planters of the Commonwealth : a Study of the Emigrants And
THE PLANTERS OF THE COMMONWEALTH A Study of the Emigrants and Emigration in COLONIALTIMES:to which are added Lists of Passengers to BOSTON and to the BAY CoLoNY; the SHIPS which brought them; their English Homes, and the Places of their Settlement in MASSACHUSETTS I62o—I64.o_ By CHARLES EDWARD BANKS Meméer 0f the MASSACHUSETTSHISTORICAL SOCIETY and of the AMERICAN ANTIQUARIAN SOCIETY Wit};Illustrations BOSTON Printed by ‘The Riverside Press for HOUGHTONMIFFLIN COMPANYin PARK STREET near the COMMON MDCCCCXXX '\ ‘-m-425:2/9"“ ‘T/9ePlanter: of t/ae Commonwealth "’'‘‘=‘%a-'--aua1...4”‘...: SIR JOHN POPHAM Chief Justice of England Who, in 1606, sent the first colony of emigrants to New England COPYRIGHT, I930, BY CHARLES E. BANKS ALL RIGHTSTHIS RESERVED BOOK OR PARTSINCLUDING THEREOF THE RIGHTIN ANY TO FORM REPRODUCE ‘ Respectfully Dedicated to SHERMAN LELAND WHIPPLE, ESQ. Chairman of the Founders’ Memorial Committee of Boston Whose Interest in the Early History Of Massachusetts and its Planters Is responsiblefor the compilation of this volume ILLUSTRATIONS SIR JOHN POPHAM, ZET. 68 Frontispiece From a portrait painted in 1600 PAGE or WINTHROP JOURNAL NOTING THE ARRIVAL OF FOUR MINISTERS AND SIR HENRY VANE ON THE ABIGAIL MAP or ENGLAND SHOWING THE NUMBER 01-‘EMIGRANTS FROM EACH COUNTY 14 MAP OF ENGLAND SHOWING COUNTIES FROMWHICH THE HEAV IEST EMIGRATION TOOK PLACE I8 PAGE OF RECORDS FOR APRIL, 1632, SHOWING A LIST or PAS SENGERS FOR NEW ENGLAND 42 PAGE OF WINTHROP JOURNAL NOTING THE ARRIVAL or THE WILLIAM AND FRANCIS IN 1632 96 THE FIRST -

Section O Plot Names Inscriptions Notes OA OA5 Margaret Arthurs Edging, North: (1808-1910) MARGARET ARTHURS BORN 1808 DIED JANUARY 17TH 1910
Lyncombe & Widcombe and St James’ Cemetery – Memorials Widcombe Association Section O Plot Names Inscriptions Notes OA OA5 Margaret Arthurs Edging, north: (1808-1910) MARGARET ARTHURS BORN 1808 DIED JANUARY 17TH 1910 Reuben Arthurs (1848- Edging, south: 1939) REUBEN ARTHURS BORN 184[8] DIED MARCH 20TH 1939 Lucy Arthurs (1865- Edging, east: 1943) LUCY ARTHURS ND Edging. BORN 1865 DIED 22 OCT. 1943 The birth of Reuben Arthurs was registered 1848/Q4 Chippenham. The marriage of Reuben Arthurs to Emily Linsey/Cook at St Swithin’s, Walcot, was registered 1877/Q1 Bath. In the 1881 census at 1 Bedford Street, Walcot, Bath: Reuben Arthurs, aged 32, journeyman baker, born at Chippenham (Wilts), wife Emily, aged 29, born at Camerton (Som), two children and a niece. The death of Emily Arthurs, aged 40, was registered 1891/Q4 Bath. Buried in Locksbrook Cemetery (Walcot section). The marriage of Reuben Arthurs to Lucy Cook was registered 1894/Q4 Bath. The death of Margaret Arthurs, aged 101, was registered 1910/Q1 Bath. In the 1911 census at Rowde House, Kingston Road, Bath: Reuben Arthurs, aged 62, journey baker, born at Chippeneham (Wilts, wife Lucy, aged 44, married 17 years 1 child, children: Ethel Margaret, aged 16, born at Bath, and Emily, aged 27, single, confectioner’s assistant, born at Bath, and two boarders. From the National Probate Calendar 1939: ARTHURS Reuben of Rowde House Kingston-road Bath died 20 March 1939 Probate Bristol 3 April to Lucy Arthurs widow. Effects £165 5s. 8d. The death of Lucy Arthurs, aged 78, was registered 1943.Q4 Bath. -
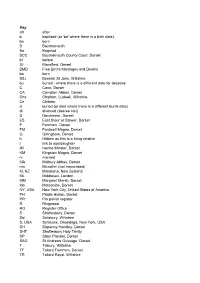
Or 'Ba' Where There Is a Birth Date
Key aft after b baptised (or 'ba' where there is a birth date) bo born B Bournemouth Ba Bagshot BCC Bournemouth County Court, Dorset bf before Bl Blandford, Dorset BMD Free Births Marriages and Deaths bo born BSJ Berwick St John, Wiltshire bu buried - where there is a different date for decease C Cann, Dorset CA Compton Abbas, Dorset Cha Charlton, Ludwell, Wiltshire Ch Chittern d buried (or died where there is a different burial date) di divorced (decree nisi) D Dorchester, Dorset ES East Stour or Stower, Dorset F Farnham, Dorset FM Fontmell Magna, Dorset G Gillingham, Dorset h Hidden as this is a living relative I link to son/daughter IM Iwerne Minster, Dorset KM Kingston Magna, Dorset m married MA Melbury Abbas, Dorset mic Microfilm (not transcribed) M, NZ Matakana, New Zealand ML Middlesex, London MM Margaret Marsh, Dorset Mo Motcombe, Dorset NY, USA New York City, United States of America PH Piddle Hinton, Dorset PPr Pre parish register R Ringwood RO Register Office S Shaftesbury, Dorset Sal Salisbury, Wiltshire S, USA Syracuse, Onondaga, New York, USA SH Sixpenny Handley, Dorset SHT Shaftesbury Holy Trinity SP Stour Provost, Dorset SAG St Andrews Gussage, Dorset T Tisbury, Wiltshire TF Tollard Farnham, Dorset TR Tollard Royal, Wiltshire USA United States of America W Wimborne, Dorset WW West Witton, Yorkshire Y Yeovil, Somerset Further work necessary / to check Adams family (Elizabeth) Elizabeth Adams m 5/5/1762 Corsham John Ruddle bo 19/7 ba 27/7/1735 Corsham, Wiltshire b bf 1744 not Cor d 15/11/1814 Corsham (age 86) d 19/1/1789 Corsham I Thomas Adams m 9/8/1730 Tormarton & Littleton, Eliza Tutt m 30/9/1740 Corsham (2nd) Elizabeth Silverthorn b bf 1712 Gloucestershire (1st) b bf 1712 b bf 1720 d 7/11 bu 10/11/1775 Corsham d 1737-40 d aft 1775 I William Adams m bf 1691 (Susan ?) ? b bf 1665 b bf 1665 d 1691 Corsham d aft 1691 Elizabeth Adams (1735-1814) Children of John and Elizabeth Ruddle - Thomas 1763 (bu 1763), Thomas 1764, Betty 1765 (bu 1766), Mary 1766, William 1768, Elizabeth 1770, John 1771 (bu 1773), John (bu 1775). -

The Planters of the Commonwealth; a Study of the Emigrants And
The Planters of the Commonwealth THIS EDITION CONSISTS OF SEVEN HUNDRED AND EIGHTY- SEVEN NUMBERED COPIES PRINTED AT THE RIVERSIDE PRESS, CAMBRIDGE, MASSACHUSETTS, U.S.A., IN I93O. SEVEN HUNDRED AND FIFTY OF THESE ARE FOR SALE. THIS IS NUMBER. f<l JC SIR JOHN POPHAM Chief Justice of England Who, in 1606, sent the first colony of emigrants to New England THE PLANTERS OF THE COMMONWEALTH A Study of the Emigrants and Emigration in Colonial Times: to which are added Lists of Passengers to Boston and to the Bay Colony; the Ships which brought them; their English Homes, and the Places of their Settlement in Massachusetts 1620—1640 By CHARLES EDWARD BANKS Member of the Massachusetts Historical Society and of the American Antiquarian Society With Illustrations BOSTON Printed by The Riverside Press for Houghton Mifflin Company in Park Street near the Common mdccccxxx COPYRIGHT, 1930, BY CHARLES E. BANKS ALL RIGHTS RESERVED INCLUDING THE RIGHT TO REPRODUCE THIS BOOK OR PARTS THEREOF IN ANY FORM 289137 Respectfully Dedicated to SHERMAN LELAND WHIPPLE, Esq. Chairman of the Founders’ Memorial Committee of Boston Whose Interest in the Early History of Massachusetts and its Planters Is responsible for the compilation of this volume PREFACE WHEN Englishmen left their island to emigrate to the North American continent, to begin a new life in the unexplored wilderness, they adopted a name for themselves by which they were generally known in the first century of their experiment. The places to which they went were called ‘plantations.’ Bradford’s ‘History’ is of the ‘ Plimmoth Plantation ’ — not the Plymouth Colony — and the various settlements in Virginia bore the name of planta¬ tions until within the memory of the present generation. -

LONDON METROPOLITAN ARCHIVES Page 1 HARBEN BEQUEST
LONDON METROPOLITAN ARCHIVES Page 1 HARBEN BEQUEST HB Reference Description Dates Early deeds HB/A/001 Chirograph Indented. Grant 5 Ed II 1. Brother Peter, Prior of the Hospital of St. [1311/12] Katherine next the Tower and the brethren and sisters there. 2. Sir Adam de Chiuenynggis. Piece of land in the parish of Blessed Mary of 'Newenton extra Barram de Suthwerk' near the land of Robert de Cober. Witnesses--Sir John Joce, Richard clericus de 'Suthwark,' Roger de Pulter, Henry de Hatton, Nicholas de Anton, John de Hatton, Simon de Bernwell, Walter de Milword, John le Bruer, Nicholas de Stafhurst, William clericus. HB/A/002 Chirograph Indented. Acknowledgment of 15 Ed II undertaking by way of Mortgage [1321/22] 1. Gilbert de Balsham, Saddler of London. 2. Adam de Cheueninggis, son of Sir Adam de Cheueninggis. Land at 'Newenton extra Barram de Suthwerk.' Witnesses--Richard de Langeford, Henry Graspeys, Simon de Bernewell, Thomas le Barber, Henry le Taillur, William called le Melleward, Godfrey Pourte, Henry de Hactone, Ralph clericus. HB/A/003 Grant 50 Ed III 1. William de Melton, chaplain. 2. William Boys [1376/77] of County Dorset, Godfrey Chauflour, Adam lady, tailor of London. Tenement, land etc. in the lane and parish of St. Clement near the street of 'Candelwykstrete' in the ward of 'Lumbardstrete.' Near the tenements of John Fraunceys and Walter Osekyn, Belonged formerly to William leght and Sarre his wife. Witnesses--John Chichester, Thomas Clench, Simon Crowe, Thomas atte Barnet, Richard atte Dych. LONDON METROPOLITAN ARCHIVES Page 2 HARBEN BEQUEST HB Reference Description Dates HB/A/004 Grant 2 Hen IV 1. -

Phillimore's Dorset Marriage Registes Volume 1 Marriages at Powerstock and West Milton, 1568 to 1812 Marriages at Milton Abbey
Phillimore’s Dorset Marriage Registes Volume 1 Marriages at Powerstock and West Milton, 1568 to 1812 Marriages at Milton Abbey, 1559-1812 Marriages at Beaminster, 1686-1812 Marriages at Mapperton, 1669-1812 Marriages at Cattistock, 1558-1812 Marriages at Bothenhampton, 1636-1812 Marriages at Walditch, 1738-1812 Marriages at Bradpole, 1695-1812 Marriages at North Poorton, 1761-1812 Marriages at Chilfrome, 1709-1812 Marriages at Powerstock and West Milton. 1568 to 1812 Note - To the Parish and Liberty of Powerstock is added the Chapelry of West Milton. Volume 1. is a parchment roll of twenty leaves dating from 1568 , when John Blackmore was Vicar. This goes to 1608 , and is evidently a beautifully written copy of some earlier book. Vol. 2. begins 1608 and ends 1717. 66 pages, parchment--Marriages, 1715 , Burials, 1715 , bound in calf, in good preservation, also contains lists of collections by 'brief.' A gap in Baptisms from 25 Mar 1648 , to 8 Sep 1650 ; in Burials, 7 Mar 1643 , to 16 Apr 1651 ; only one marriage between 1644 and 1651. From 1632 the Baptisms, Marriages, and Burials are separate. Vol. 3, 1717 to 1748 --Bapts., Marr., Bur. From 1754 to 1787 , Bapt. and Bur., only. Parchment, stiff cover, bound in vellum, 84 pp. Vol. 4., 1754 - 1791 --Paper, bound in sheep; Banns and Marriages. Vol. 5. 1749 - 1753 --Bapt., Marr., Bur. Parchment, 72 pp. Vol. 6., 1787 - 1812 --Bapt. and Burials. Parchment, bound in sheep; 36 pp. Volume 1.- Parchment Roll. Roberte Orcharde & Katherine Wrixon 27 Sep 1568 John Perke & Elizabeth Hiskocke 9 Jan 1568 Barnard Maber & Agnes Wryxon 8 May 1569 Stephen Dowch & Joane Baron 20 Jan 1569 John Kingsbury & Alice Samway 21 Jan 1569 Richard Tisser & Elene Oxford 5 Aug 1570 Nichas Crandon & Joane Bartrom 17 Sep 1570 Robt. -

A Selection of Christian Places of Worship
T.G . Abercrombie W.H. Alleyn and Mansell Al'EC (Martin Purdy, Ken Fisher, Austin and Paley Places of Christian Worship 1914-1990: • Wallneuk Church, North Croft St, • Epiphany, Merstham, urrey. [955 Gary Dyhouse) • Christ Church, Thornton, Lancashire. Paisley. 19[3-[5. B • St Bartholomew, Barking Rd, East [9[4 (chancel). Rest Leach, Rhodes H. Anderson Ham, LB Newham. [977-83 and Walker 1963. A Selection of Christian Places ofWorship Frank Abbey and Harrison • St Mary, Little Chart, Kent. [955 • StMark, Forest Gate, [.B Newham. • St Mark, Basford, Staffs. 1914. West • St Francis Fixby, Huddersfield. [954- [986-7 end 1969-71 by Charles Lewis. R. Rowand Anderson, William 5 • St Matthias, Canning Town, LB • St Michael and All Angels, Ashton ELAIN HARWOOD & ANDREW FOSTER H. Kininmonth and A.F.B. Paul on-Ribble. Preston. West end, 19[5. Edward Adams Newham . [983-8 • Drylaw Hall/Church, Edinburgh. [957 • St Michael and All Angels, Romford • All Saints, Station Rd, Becconsall, • Congregational church, Gatley, • Brucefield Church, E. Main St, Rd, Manor Park, LB Newham. [990 Lancs. [925-6 Cheshire. [938 Whitburn, W. Lothian. [962 • StMark, TollgateRd, Beckton. LB • St Stephen-on-the-Cliffs. Blackpool, Lancs. 1925-6 Stanley Adshead and Stanley C. • Craigsbank Church, Craigs Bank, Newham. [986-{) Edinburgh. 1964-7 • Chancel, Pennington-in-Furness, Ramsey • St Stephen. Copeland Rd. • See also William H. Kininmonth Walthamstow, LB Waltham Forest. Cumbria. 1925-6 • $t Anselm, Kennington Cross, LB [988-94 • St Hilda, Bilsborrow, Lancs. 1926-7 Lambeth. [9[3-33.11 W.E. Ellery Anderson • St Bede, Bryndale Ave, Brandwood • St Luke, Orrell.