Practical Approaches to Common Musculoskeletal Conditions In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OES Site Color Scheme 1
Nuisance Problems You will Grow to Love Thomas V Gocke, MS, ATC, PA-C, DFAAPA President & Founder Orthopaedic Educational Services, Inc. Boone, NC [email protected] www.orthoedu.com Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. 2 LEARNING GOALS At the end of this sessions you will be able to: • Recognize nuisance conditions in the Upper Extremity • Recognize nuisance conditions in the Lower Extremity • Recognize common Pediatric Musculoskeletal nuisance problems • Recognize Radiographic changes associates with common MSK nuisance problems • Initiate treatment plans for a variety of MSK nuisance conditions Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response* When does the Inflammatory response occur: • occurs when injury/infection triggers a non-specific immune response • causes proliferation of leukocytes and increase in blood flow secondary to trauma • increased blood flow brings polymorph-nuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to injured tissues *Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137 Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. -
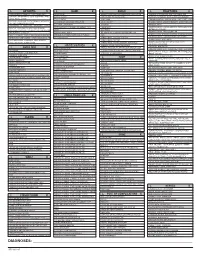
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report
SCIENTIFIC ARTICLE Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report Cassie Gyuricza, MD, Eva Umoh, BA, Scott W. Wolfe, MD We report a case of pulley rupture following repeated local corticosteroid injections for trigger digit. The treatment involved exploration, tenolysis, and reconstruction using the palmaris longus tendon. (J Hand Surg 2009;34A:1444–1448. © 2009 Published by Elsevier Inc. on behalf of the American Society for Surgery of the Hand.) Key words Corticosteroid, pulley rupture, trigger digit. RIGGER DIGIT, OR stenosing tenosynovitis,isa local corticosteroid injection through a lateral approach condition characterized by painful locking or at the proximal phalanx10 (0.5 mL local anesthetic and Tsnapping of a digit caused by mechanical im- 0.5 mL triamcinolone acetonide 40 mg/mL [Kenalog- pingement of the flexor tendon passing through a hy- 40, Bristol-Meyers Squibb Co, Princeton, NJ]). Her pertrophic A1 pulley. Initial conservative management symptoms of pain temporarily improved, but 4 months of trigger digits with various corticosteroid preparations later, the patient returned with recurrent pain and a is well described.1–4 Side effects, including subcutane- second local corticosteroid injection was administered, ous fat atrophy, pain, depigmentation of the skin, and again using the lateral approach. During the ensuing 8 transient elevation of urine and blood glucose levels in months, the patient had persistent pain and tenderness patients with diabetes, are generally mild and self- over the A2 pulley. The patient also developed pain at limiting.5,6 We are aware of 2 previously reported cases the A1 pulley, and a third injection (0.5 mL local of delayed flexor tendon rupture following corticoste- anesthetic and 0.5 mL triamcinolone acetonide 40 mg/ 7,8 roid injections for trigger digit thought to be the result mL) was given into the palmar surface overlying the A1 of intratendinous injection. -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

Opso Summer 2014
The Lower Extremity OPSO Summer Primary Care CME Conference August 15, 2014 K. Turner Slicho, DO Case Presentation 53-year-old Caucasian female complains of left sided SI pain described as an ache w/o radiation Initial onset of pain was 25 years ago, when her back “seized up” bending over to put her toddler to bed. Infrequent issues over the next 10-15 years, then began to be more problematic Now, constant pain over the last 2 years Numbness in a small area of left shin. Denies weakness, tingling Case Presentation Unable to sit for long periods, bend over, cross legs comfortably Does not lift her grandson Does not brush teeth bending over without holding the sink No longer exercising due to pain 15 chiropractic session with two different providers over 2 years with “absolutely zero effect” on her pain 12 physical therapy sessions with marginal effect Case Presentation PMHx: Unremarkable** FHx: Cancer, DM, Food Allergies, Meniere’s Disease, Restless leg syndrome, Ulcerative colitis PSHx: C-section 1990, Appendectomy 2009, Hernia repair 2005 Meds: Diclofenac 100mg BID Case Presentation X-Ray: L4-L5 degenerative changes. Normal pelvis and SI joints bilaterally MRI: mild degenerative changes L3-S1 without significant neuroforaminal or spinal stenosis Neurosurgical evaluation : non-surgical back Case Presentation Gen: NAD, A&O x 3 Neuro: 2+/4 DTR’s, Strength 5/5, no motor deficits, mild sensory loss in left superio-lateral shin Extremities: no edema, ecchymosis, peripheral pulses normal Case Presentation: Somatic Dysfunction findings Cervical: Left posterior OA facet restriction Lumbar: L5 ERSl, left iliolumbar ligament hypertonicity, mild left psoas spasm and left erector spinae m. -

2014 Newsletter – Winter
NEWS ISSUE 14 I WINTER 2014 Welcome to our Winter edition of Orthosports News Winter is the time when Alpine Injuries present themselves WHO ORTHOSPORTS – Dr Doron Sher covers the most common types of alpine ARE WE? LOCATIONS injuries. Dr Kwan Yeoh takes a look at Mallet Finger and Orthosports is > Concord 02 9744 2666 “Imaging of the knee” is covered by Dr Sher in our Key a professional > Hurstville 02 9580 6066 Examination Points Section. association of > Penrith 02 4721 7799 Many GPs have attended our Category 1 Education Modules; AOA Orthopaedic > Randwick 02 9399 5333 A USTRAL I A N ORTHOPA EDIC Surgeons based Or visit our website there are 4 remaining dates for our 2014 RACGP approved A S S O CIA T I O N modules. See page 4 for details. in Sydney. www.orthosports.com.au We hope you enjoy this issue – The Team at Orthosports elbow injuries and more comminuted clavicle fractures. Alpine Injuries Shoulder dislocation is also very common. Snowboarders do not usually injure their legs when both feet are attached Skiing and snowboarding are exhilarating sports. They to the board but injuries to the knee are not uncommon are physically demanding and require co-ordination, getting on and off lifts when only one foot is bound to the strength, fitness and lots of specialized equipment. More board (more common in beginners). If they do injure their people ski than snowboard and snowboarders are generally knee, it is almost always in a terrain park landing from younger than skiers. Skiing and snowboarding injuries a big jump. -

Top Hand, and Wrist Problems
12/10/2016 TOP HAND, AND WRIST Disclosures PROBLEMS: HOW TO • None SPOT THEM IN CLINIC Nicolas H. Lee, MS MD [email protected] UCSF Dept of Orthopaedic Surgery Assistant Clinical Professor Hand, Upper Extremity and Microvascular Surgery Dec. 10 th , 2016 Outline Outline • Carpal Tunnel Syndrome •Carpal Tunnel Syndrome • Trigger Finger • • Basal Joint arthritis Trigger Finger • Basal Joint arthritis • De Quervain tenosynovitis • De Quervain tenosynovitis • Mallet Finger • Mallet Finger • Ganglion cyst • Ganglion cyst 1 12/10/2016 Carpal Tunnel Syndrome • Compression of median nerve in carpal tunnel • Irritation of the nerve presents as numbness/pain 10 structures 9 flexor tendons Median nerve https://www.pinterest.com/pin/429812358163325007/ Anatomy (motor) Etiology 1. Idiopathic – most common 2. Anatomic – rare • Thenar Muscle (OAF) 3. Systemic – DM, hypothyroidism • Opponens Pollicis (deep) 4. **** Occupational Exposure • Abductor Pollicis Brevis (superficial) **** “A direct relationship between repetitive work • Flexor Pollicis Brevis activity (eg, keyboarding) and CTS has never been (superficial 1/2) objectively demonstrated.” 1 http://teachmeanatomy.info/upper-limb/muscles/hand/ 2 12/10/2016 Rare anatomic causes Carpal Tunnel Syndrome ● HPI – systemic risk factors Tenosynovitis CMC arthritis ◦ More common in: Ganglion Fracture 1) Diabetics 2) Hypothyroidism 3) Pregnancy (20-45%) Persistent Median artery Acromegaly Abnormal muscle Tumor Carpal Tunnel Syndrome ● CC: ◦ “I wake up at night and my hands are asleep” ◦ “I have to shake them to get the blood flowing again” ◦ “I have to run them under warm water and then I can go back to sleep” ◦ “Fingers go numb when I drive” ◦ “My hand goes numb when I use my cell phone” ◦ “I am always dropping things” Carpal Tunnel Syndrome Cranford, C.S. -

High Ankle Sprain
SYNDESMOSIS INJURY (HIGH ANKLE SPRAIN) A syndesmosis injury, also known as a high WHAT ARE THE SYMPTOMS ● Restore joint proprioception ankle sprain, is an injury to the ligaments OF A SYNDESMOSIS and balance at the top of your ankle. These high ankle INJURY? ● Restore normal function ligaments connect your tibia (shin bone) and ● Pain felt above the ankle that increases ● Walking fi bula (outside leg bone) to your calcaneum with outward rotation of the foot ● Running (heel bones), and form part of your ankle. ● Pain with walking and often signifi cant ● Jumping and landing The injury involves the syndesmosis, a bruising and swelling across the higher ● Speed and agility ligament that holds the lower part of your ankle rather than around the malleolus ● Sport-specifi c skills tibia and fi bula together just above your (ankle bones) ● Resume sport. ankle joint. ● Inability to perform a one-legged calf High ankle sprains are much less raise (going up onto your toes) Phase 1 of treatment is focused around common but are more disabling than your ● Feeling of instability/‘no confi dence’ pain relief and reducing infl ammation. traditional lower ankle sprain (when you jumping on the injured leg. This includes the RICE protocol - rest, ice, roll over the outside of your ankle). They compression and elevation. Treatments must be diagnosed early and appropriate The severity of the symptoms will depend may also include electrotherapy, strapping treatment started, which differs from a on the grade of ankle sprain. Patients with and gentle massage after the fi rst 48 hours. traditional ankle sprain, in order to get best a high ankle sprain without fracture may be Phase 2 of treatment, the therapist will results. -

Imaging of the Bursae
Editor-in-Chief: Vikram S. Dogra, MD OPEN ACCESS Department of Imaging Sciences, University of HTML format Rochester Medical Center, Rochester, USA Journal of Clinical Imaging Science For entire Editorial Board visit : www.clinicalimagingscience.org/editorialboard.asp www.clinicalimagingscience.org PICTORIAL ESSAY Imaging of the Bursae Zameer Hirji, Jaspal S Hunjun, Hema N Choudur Department of Radiology, McMaster University, Canada Address for correspondence: Dr. Zameer Hirji, ABSTRACT Department of Radiology, McMaster University Medical Centre, 1200 When assessing joints with various imaging modalities, it is important to focus on Main Street West, Hamilton, Ontario the extraarticular soft tissues that may clinically mimic joint pathology. One such Canada L8N 3Z5 E-mail: [email protected] extraarticular structure is the bursa. Bursitis can clinically be misdiagnosed as joint-, tendon- or muscle-related pain. Pathological processes are often a result of inflammation that is secondary to excessive local friction, infection, arthritides or direct trauma. It is therefore important to understand the anatomy and pathology of the common bursae in the appendicular skeleton. The purpose of this pictorial essay is to characterize the clinically relevant bursae in the appendicular skeleton using diagrams and corresponding multimodality images, focusing on normal anatomy and common pathological processes that affect them. The aim is to familiarize Received : 13-03-2011 radiologists with the radiological features of bursitis. Accepted : 27-03-2011 Key words: Bursae, computed tomography, imaging, interventions, magnetic Published : 02-05-2011 resonance, ultrasound DOI : 10.4103/2156-7514.80374 INTRODUCTION from the adjacent joint. The walls of the bursa thicken as the bursal inflammation becomes longstanding. -

Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: a Case Report Matthew Eh Rring Governors State University
Governors State University OPUS Open Portal to University Scholarship All Capstone Projects Student Capstone Projects Spring 2015 Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: A Case Report Matthew eH rring Governors State University Follow this and additional works at: http://opus.govst.edu/capstones Part of the Physical Therapy Commons Recommended Citation Herring, Matthew, "Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: A Case Report" (2015). All Capstone Projects. 124. http://opus.govst.edu/capstones/124 For more information about the academic degree, extended learning, and certificate programs of Governors State University, go to http://www.govst.edu/Academics/Degree_Programs_and_Certifications/ Visit the Governors State Physical Therapy Department This Project Summary is brought to you for free and open access by the Student Capstone Projects at OPUS Open Portal to University Scholarship. It has been accepted for inclusion in All Capstone Projects by an authorized administrator of OPUS Open Portal to University Scholarship. For more information, please contact [email protected]. MULTIMODAL PHYSICAL THERAPY MANAGEMENT OF A 24 YEAR-OLD MALE WITH CHRONIC RETROCALCANEAL PAIN: A CASE REPORT By Matthew Herring B.S., Lewis University, 2006 Capstone Project Submitted in partial fulfillment of the requirements For the Degree of Doctor of Physical Therapy Governors State University University Park, IL 60484 2015 ABSTRACT Background and Purpose: The multimodal approach reflects the type of individualized treatment commonly used in the clinical setting, in which many different interventions are available to the physical therapist. The purpose of this case report is to describe the physical therapy management process for a patient with chronic retrocalcaneal pain using a multimodal intervention approach. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -

ESSR 2013 | 1 2 | ESSR 2013 Essrsport 2013 Injuries Musculoskeletal Radiology June 13–15, MARBELLA/SPAIN
Final Programme property of Marbella City Council ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN Content 3 Welcome 4–5 ESSR Committee & Invited Speakers 6 General Information 11/13 Programme Overview ESSR 2013 | 1 2 | ESSR 2013 ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN from the ESSR 2013 Congress President ME Welcome LCO On behalf of the ESSR it is a pleasure to invite you to participate in the 20th Annual Scientific Meeting WE of the European Skeletal Society to be held in Marbella, Spain, on June 13–15, 2013, at the Palacio de Congresos located in the center of the city. The scientific programme will focus on “Sports Lesions”, with a refresher course lasting two days dedicated to actualised topics. The programme will include focus sessions and hot topics, as well as different sessions of the subcommittees of the society. There will be a special session on Interventional Strategies in Sports Injuries. The popular “hands on” ultrasound workshops in MSK ultrasound will be held on Thursday 13, 2013, during the afternoon, with the topic of Sports Lesions. Basic and advanced levels will be offered. A state-of-the-art technical exhibition will display the most advanced technical developments in the area of musculoskeletal pathology. The main lobby will be available for workstations for the EPOS as well as technical exhibits. Marbella is located in the south of Spain, full of life and with plenty of cultural and tourist interest, with architectural treasures of the traditional and popular Andalusian culture.